Acute upper gastrointestinal bleeding caused by esophageal right bronchial artery fistula:A case report
2021-11-20AlbertoMartinoGaspareOlivaFrancescoPaoloZitoMattiaSilvestreRaffaeleBennatoLuigiOrsiniRaffaellaNiolaLuigiaRomanoGiovanniLombardi
Alberto Martino,Gaspare Oliva,Francesco Paolo Zito,Mattia Silvestre,Raffaele Bennato,Luigi Orsini,Raffaella Niola,Luigia Romano,Giovanni Lombardi
Alberto Martino,Francesco Paolo Zito,Raffaele Bennato,Luigi Orsini,Giovanni Lombardi,Department of Gastroenterology and Digestive Endoscopy,AORN “Antonio Cardarelli”,Napoli 80131,Italy
Gaspare Oliva,Luigia Romano,Department of General and Emergency Radiology,AORN“Antonio Cardarelli”,Napoli 80131,Italy
Mattia Silvestre,Raffaella Niola,Department of Interventional Radiology,AORN “Antonio Cardarelli”,Napoli 80131,Italy
Abstract BACKGROUND Fistula between the esophagus and bronchial artery is an extremely rare and potentially life-threatening cause of acute upper gastrointestinal bleeding.Here,we report a case of fistula formation between the esophagus and a nonaneurysmal right bronchial artery (RBA).CASE SUMMARY An 80-year-old woman with previous left pneumonectomy and recent placement of an uncovered self-expandable metallic stent for esophageal adenocarcinoma was admitted due to hematemesis.Emergent computed tomography showed indirect signs of fistulization between the esophagus and a nonaneurysmal RBA,in the absence of active bleeding.Endoscopy revealed the esophageal stent correctly placed and a moderate amount of red blood within the stomach,in the absence of active bleeding or tumor ingrowth/overgrowth.After prompt multidisciplinary evaluation,a step-up approach was planned.The bleeding was successfully controlled by esophageal restenting followed by RBA embolization.No signs of rebleeding were observed and the patient was discharged home with stable hemoglobin level on postoperative day 7.CONCLUSION This was a previously unreported case of an esophageal RBA fistula successfully managed by esophageal restenting followed by RBA embolization.
Key Words:Upper gastrointestinal bleeding;Acute upper gastrointestinal bleeding;Esophageal fistula;Bronchial artery esophageal fistula;Esophageal stenting;Esophageal self-expandable metal stenting;Case report
INTRODUCTION
Acute upper gastrointestinal bleeding (UGIB) is a potentially life-threatening emergency with a reported incidence of about 100 per 100000 persons per year[1,2].Its etiology has been divided into variceal and nonvariceal bleeding.The most common causes of acute UGIB include peptic ulcer disease and esophageal varices,followed by Mallory–Weiss syndrome and neoplasms[1-3].Acute UGIB caused by esophageal bronchial artery fistula is extremely rare.To date,only a few cases of fistula formation between the esophagus and the right bronchial artery (RBA) have been reported worldwide.Here,we describe a previously unreported case of a fistula between the esophagus and a nonaneurysmal RBA,in the setting of palliative esophageal metallic stenting and previous left pneumonectomy.
CASE PRESENTATION
Chief complaints
An 80-year-old woman was admitted to our bleeding unit due to severe anemia(hemoglobin 7.1 g/dL) and hematemesis with signs of hemodynamic instability.
History of present illness
One episode of hematemesis with presyncope occurred 1 h prior to hospital admission.
History of past illness
The patient underwent left pneumonectomy with adjuvant chemoradiotherapy for lung cancer 6 years before.An uncovered self-expandable metallic stent (SEMS) had been placed 3 mo prior at another institution for the palliation of a locally advanced esophageal adenocarcinoma.
Personal and family history
The patient denied further medical history.There was no family history of GI cancer.
Physical examination
On presentation,the patient was hemodynamically unstable (pulse 115 bpm,blood pressure 90/60 mmHg).She was afebrile,with respiratory rate 17 breaths/min and oxygen saturation 94%.On general physical examination,she looked pale and dehydrated.Abdominal examination revealed nondistended,nontender abdomen with normal bowel sounds.The rectal examination exhibited melena.
Laboratory examinations
Complete blood count analysis was notable for hemoglobin of 7.1 g/dL and hematocrit of 23.6%.All remaining laboratory examinations,including liver enzymes,coagulation studies and renal function tests,were within normal limits.
Imaging examinations
After blood transfusion and hemodynamic stabilization,emergent computed tomography (CT) angiography was performed showing no active GI bleeding with the esophageal stent correctly placed.The RBA appeared tortuous,dilated and tightly adherent to the thickened middle esophagus wall.Although no contrast extravasation was noted,the tissue planes between the RBA and the esophagus appeared obliterated(Figure 1).

Figure 1 Arterial phase contrast-enhanced computed tomography.
MULTIDISCIPLINARY EXPERT CONSULTATION
After prompt multidisciplinary evaluation,involving a GI endoscopist,surgeon,and a diagnostic and interventional radiologist,a minimally invasive step-up approach with esophageal restenting followed,if necessary,by RBA embolization was planned.
FINAL DIAGNOSIS
Fistula formation between the esophagus and a nonaneurysmal RBA,in the setting of palliative esophageal metallic stenting and previous left pneumonectomy.
TREATMENT
Under fluoroscopic and direct endoscopic guidance,an over-the-guidewire partially covered SEMS was placed through the previously inserted uncovered SEMS.Immediately thereafter,diffuse esophageal bleeding controlled by the partially covered SEMS was endoscopically noted (Figure 2).On postoperative day (POD) 1,hematemesis with severe anemization (hemoglobin 5.7 g/dL) and hemodynamic instability occurred.After blood transfusion and hemodynamic stabilization,emergent CT angiography was repeated,showing the esophageal stents correctly placed with unmodified previous findings and no GI active bleeding.Esophagogastroduodenoscopy (EGD) revealed fresh blood within the esophagus and a large amount of dark blood under the partially covered SEMS,in the absence of identifiable active bleeding sites (Figure 3).Thus,operative angiography was performed.Selective RBA arteriography showed contrast extravasation within the esophagus and RBA was successfully embolized with microcoils (Figure 4).

Figure 2 Placement of partially covered self-expandable metal stent (white arrow) through the previously inserted uncovered metal stent(orange arrow).
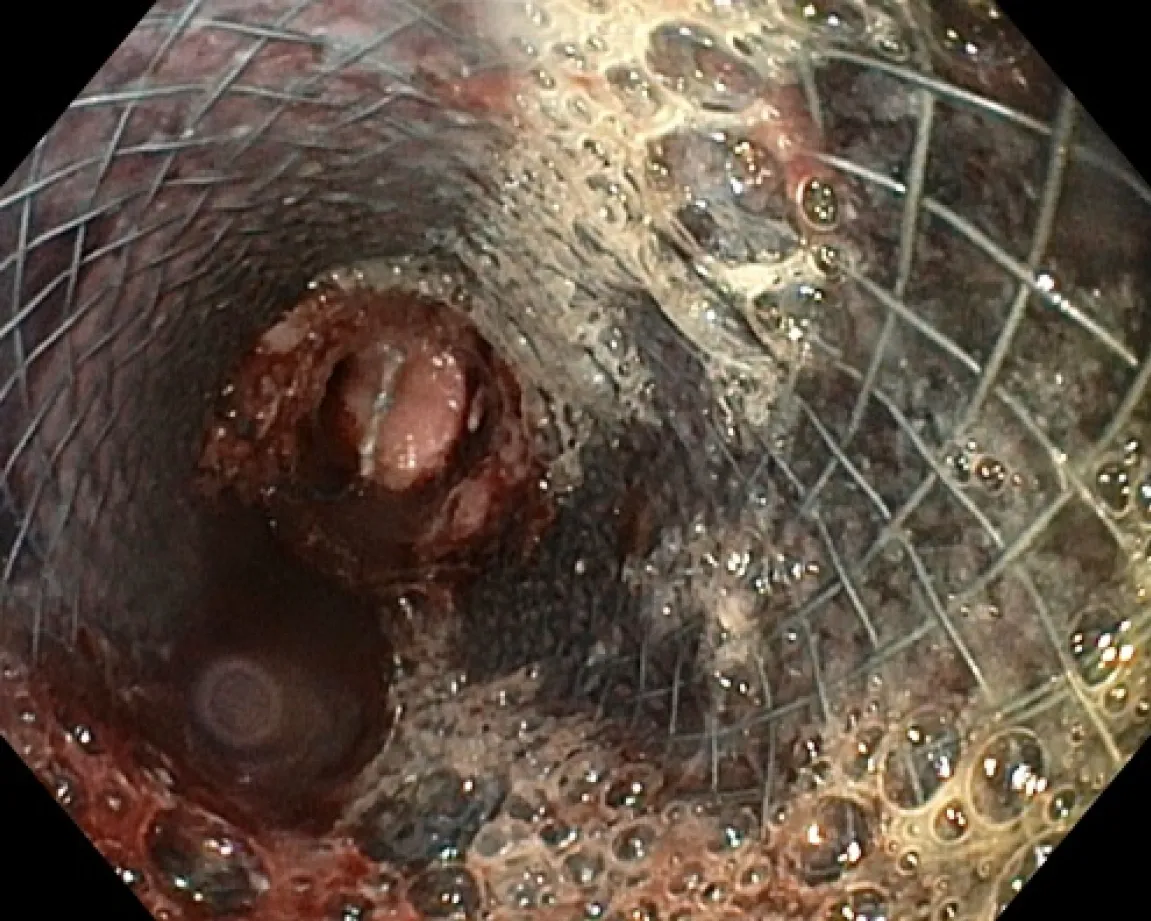
Figure 3 Second upper endoscopy showing fresh blood within the esophageal lumen and a diffuse amount of dark blood under the partially covered metal stent,in the absence of active bleeding sites.

Figure 4 Operative angiography.
OUTCOME AND FOLLOW-UP
Postoperative stay was complicated by the occurrence of pulmonary edema responsive to medical therapy.No rebleeding was observed and the patient was discharged home with stable hemoglobin level (9.1 g/dL) on POD 7.The patient died at home 1 mo postoperatively,in the absence of overt GI rebleeding or anemization.
DISCUSSION
Arterioesophageal fistulas (AEFs) are pathological communications between an arterial system and the esophagus,which may lead to exsanguination from massive UGIB if not recognized promptly.They develop most commonly due to aortic fistulization caused by foreign bodies,aortic aneurysm,or esophageal neoplasms[4-6].Nonaortic AEFs have been less frequently reported,with the bronchial artery being the most commonly involved vessel.Etiology includes foreign bodies,vascular surgery and thoracic arterial malformations,and chemoradiotherapy in esophageal cancer patients with invasion of the aorta[7,8].
Although extremely rare,an esophageal RBA fistula is a potentially life-threatening condition.To date,only a few cases of fistula formation between the esophagus and a bronchial artery aneurysm have been reported.Shaer and Bashist[9] first reported a fatal case of massive UGIB due to a bronchial artery aneurysm with an esophageal fistula (BAAEF).Later on,two cases of BAAEFs successfully treated with RBA coil embolization have been reported[10,11].In 2018,Nakada[12] reported a case of BAAEF caused by bronchial arterial embolization.Due to the unfeasibility of transcatheter coil embolization,hemostasis was achieved by emergent thoracic endovascular aortic repair.Subsequently,aneurysmotomy,debridement and pedicled omental flap repair were successfully performed.Finally,a case of fistula between the esophagus and a RBA pseudoaneurysm secondary to an endobronchial ultrasoundguided transbronchial needle aspiration has been recently reported.This was successfully managed by endoscopic clipping followed by transcatheter coil embolization[13].
Moreover,only four cases of esophageal fistulas with a nonaneurysmal RBA have been reported,including three patients with locally advanced esophageal cancer and one with Mallory–Weiss tear refractory to endoscopic hemostasis.In all cases,the esophageal bleeding was successfully controlled by means of transcatheter arterial embolization[14-16].
However,to our knowledge,this is the first reported case of a fistula between the esophagus and a nonaneurysmal RBA,in the setting of palliative esophageal metallic stenting and previous left pneumonectomy.
In our case,emergent CT showed no active GI bleeding with the esophageal stent correctly placed.Although no direct signs of fistulization were observed,the RBA appeared tortuous,dilated and tightly adherent to the thickened middle esophagus wall,with obliteration of the tissue planes between the RBA and the esophagus.Subsequent emergent EGD confirmed the absence of active bleeding without identifiable bleeding sources.After prompt multidisciplinary evaluation,a minimally invasive step-up approach with esophageal restenting followed,if necessary,by RBA embolization was planned.However,after esophageal restenting,rebleeding occurred.Thus,operative angiography was performed.Selective RBA arteriography showed contrast extravasation within the esophageal lumen and RBA embolization was performed.
CONCLUSION
Digestive endoscopists should be aware of this critical,albeit extremely rare,cause of UGIB,in order to provide prompt diagnosis and treatment.In our opinion,early diagnosis,multidisciplinary evaluation and prompt tailored treatment seem to be crucial for the proper management of an esophageal RBA fistula.