Acute hepatitis associated with increased atypical lymphocyte
2021-11-08HiYnSunHiJingTongWeiCui
Hi-Yn Sun , Hi-Jing Tong , D-Wei Cui
a Department of Clinical Laboratory, Shaoxing Second Hospital, Shaoxing 3120 0 0, China
b Department of Blood Transfusion, The Fir st Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
TotheEditor:
HepatitisAand hepatitisEare acute infectious diseases caused by hepatitisAvirus (HAV) and hepatitisEvirus (HEV), which are mainly transmitted through the fecal-oral route [1] . The early clin-ical symptoms of patients with hepatitisAorEare nonspecific, in-cluding fever, chills, abdominal pain, diarrhea, and rash [2] . More-over, the levels of specific laboratory diagnostic biomarkers, such as serum anti-HAV/HEV IgM antibodies, are too low to be de-tectable which make the early diagnosis difficult [ 1,3 ]. These pa-tients are sometimes misdiagnosed in the early stage which re-sult in inappropriate treatments [1] . Atypical lymphocyte is most common in Epstein-Barr virus (EBV) infection [ 4,5 ]. However, there are few reports of atypical lymphocyte caused by hepatitis virus. In this study, we report two cases of acute hepatitis with atypical lymphocyte to provide values for the diagnosis of the disease.
Case 1: A 28-year-old male patient was admitted into Depart-ment of Infectious Diseases on May 1, 2020 due to “fever for a week”. A week ago, the patient began to have fever, slight chills, slight limb pain and fatigue without obvious etiology, he had no obvious cough, sputum and chest tightness. On May 1, laboratory results showed that the number of white blood cell (WBC) was 17.1 ×109/L, lymphocytes accounted for 78%, of which atypical lymphocyte accounted for 18% ( Fig. 1 A). Emergency biochemistry showed elevated alanine aminotransferase (ALT), aspartate amino-transferase (AST), lactate dehydrogenase (LDH), D-dimer, and hy-persensitive C-reactive protein (hs-CRP) ( Table 1 ). The patient was suspicious of infectious mononucleosis at admission. After admis-sion, the patient was given supportive treatments with drugs in-cluding oseltamivir capsule, glycyrrhizin, glutathione injection and polyene phosphatidylcholine capsule depending on the symptoms. On May 2, the number of WBC was 9.6 ×109/L, lymphocytes accounted for 75%, of which atypical lymphocyte accounted for 15%. Biochemical results showed decreased levels of ALT, AST, LDH, D-dimer, hs-CRP, compared to the results from May 1. Moreover, other results of pathogens were negative including hepatitis virus IgM antibodies, human immunodeficiency virus (HIV-1/2), syphilis, antinuclear antibody spectrum, and EBV antibody. Due to fever and high proportion of atypical lymphocyte, bone marrow examination was given to assist in diagnosis and treatment. On May 6, atypical lymphocyte accounted for<2% in lymphocytes. Some biochemical results continually decreased including ALT, AST, LDH, total biliru-bin (TBil) and D-dimer. Surprisingly, hepatitis virus antibody test showed that the level of HAV-IgM antibody was 37.36 S/CO, which indicated HAV infection for the patients. Therefore, final clinical di-agnosis was acute HAV infection based on clinical characteristics and laboratory results.
Case 2: A 38-year-old male patient was admitted into Depart-ment of Hepatology and Gastroenterology on January 18, 2021 due to “sore throat, fever and fatigue for 4 days”. The patient devel-oped sore throat, fever and discomfort with no obvious incentive 4 days ago. Laboratory results showed that the number of WBC was 4.2 ×109/L, lymphocytes accounted for 32%, of which atypi-cal lymphocyte accounted for 12% ( Fig. 1 B). Biochemical examina-tion showed elevated levels of ALT, AST, LDH, D-dimer, and hs-CRP ( Table 1 ). The patient was also suspicious of infectious mononu-cleosis at admission. However, viruses-related examinations were negative. The patient was given supportive treatment including os-eltamivir capsule, glycyrrhizin, glutathione injection and polyene phosphatidylcholine capsule according to the symptoms. On Jan-uary 20, blood results showed that the number of WBC was 8.8 ×109/L, lymphocytes accounted for 74%, of which atypical lymphocyte accounted for 16%. Additionally, liver biochemistries were still abnormal. By January 26, the blood routine examination showed that atypical lymphocytes accounted for<2% in lympho-cytes. The levels of ALT and AST were significantly decreased, and other results returned to the normal reference value. Interestingly, the serum level of HEV-IgM antibody was 10.45 S/CO, indicating that the patient was recently infected with HEV. Therefore, final clinical diagnosis was acute HEV infection according to clinical and laboratory results.
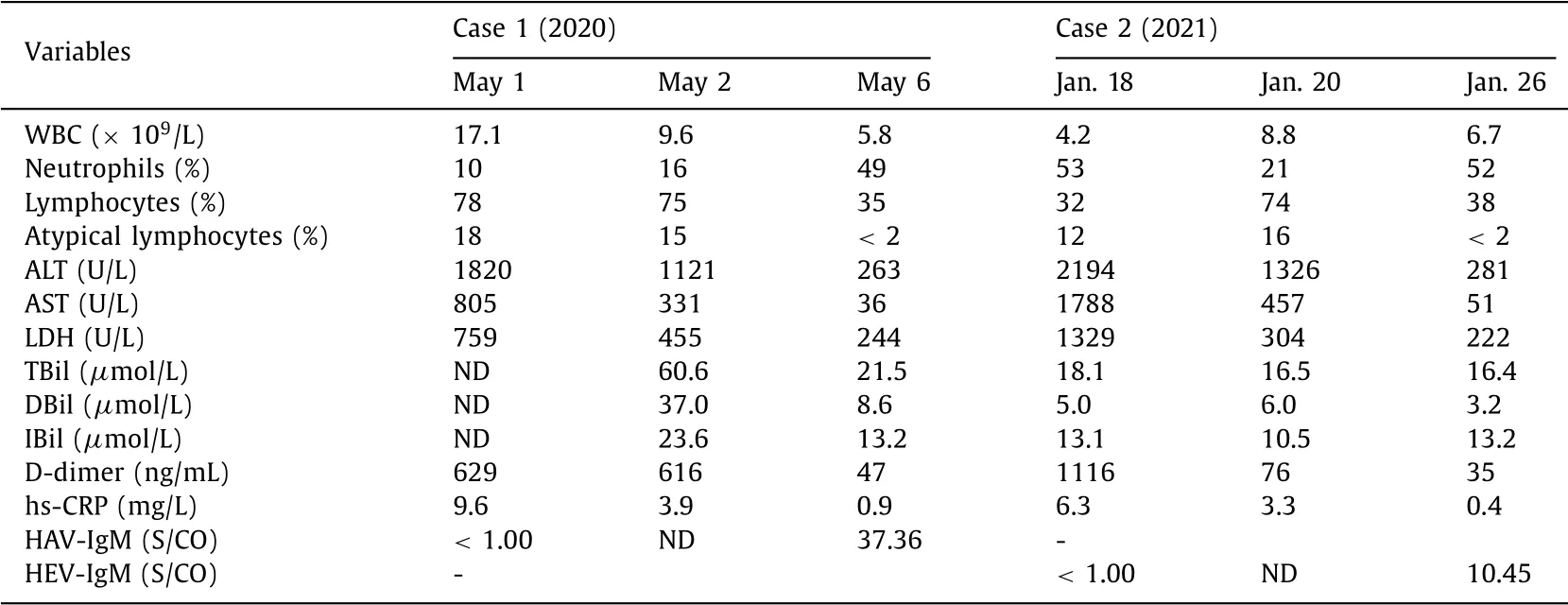
Table 1 Laboratory results of two cases with high ratio of atypical lymphocytes.
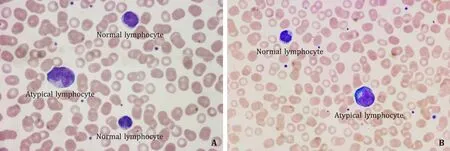
Fig. 1. Atypical lymphocyte in peripheral blood smear (Wright’s staining, original magnification ×10 0 0). A: Case 1 with HAV infection; B: case 2 with HEV infection.
General population is susceptible for hepatitis A which impact adults instead of early childhood due to vaccines around the world [ 2,3 ]. Hepatitis E is mainly found in young adults, middle-aged and elderly, but children and adolescents are mainly with subclin-ical infection, which is now recognized as an important factor of chronic, progressive liver disease in individuals with compromised immunity in developed countries [ 3,6 ]. In patients with HAV or HEV infection, ALT and AST are increased in the short-term, and the increased level of ALT is higher than that of other chronic hep-atitis. Moreover, patients with HEV infection tend to have higher serum bilirubin and a longer clotting time than those with HAV infection [ 2,3 ]. The two cases were adults with high ALT, AST and LDH levels. However, TBil level was low in HEV case compared to that in HAV case during acute stage. The two kinds of hepatitis are basically acute and self-limited, generally do not turn into chronic. However, with the increase of onset age, the course of disease is prolonged, and there is a trend of chronic and severe hepatitis [ 2,6–8 ]. Therefore, early diagnosis and treatment are of great sig-nificance, which can avoid aggravating hepatocyte damage due to misdiagnosis and mistreatment, and also reduce unnecessary med-ical costs.
Acute viral hepatitis is easy to be misdiagnosed in the early stage [ 1,9 ]. The reasons for misdiagnosis may be as follows: (i) lack of specificity in early clinical symptoms. Two patients in this re-port were treated for fever, chills, sore throat and sore limbs in the early stage, which were difficult to distinguish from common respiratory virus infection. (ii) Lack of specificity in early labora-tory tests. There are many causes that lead to liver function im-pairment, such as virus, drug, alcohol and other factors [1] . In this report, except for the elevated liver biochemistries, the number of atypical lymphocyte was also increased significantly in blood smear, which indicated that atypical lymphocytes are stimulated by antigens (viruses or allergens), resulting in various morpho-logical changes. The increased number of atypical lymphocytes in blood smears is more common in viral infections including EBV, cytomegalovirus and dengue fever virus [ 4,10,11 ]. However, atypi-cal lymphocytes are very rare in viral hepatitis. (iii) Methodolog-ical limitations of virus antibody and RNA detection. The titer of HAV/HEV IgM antibody is often undetectable in the early stage [6] . The detection of viral RNA is less useful because the window of viremia is very narrow [1] . On the other hand, there are many fac-tors influencing the detection, which makes it difficult to diagnose early. These findings indicate that continuous screening of hepatitis viruses is critical for early diagnosis of patients with liver damage.
The obvious increase of atypical lymphocytes is more common in infectious mononucleosis in children [ 5,6 ]. Infectious mononu-cleosis is an infectious disease caused by EBV, which often mani-fests as fever, sore throat, enlarged lymph nodes, liver and spleen, and impaired liver function [5] . However, the percentage of atyp-ical lymphocyte is often>10%, which is also called lymphoid leukemia reaction. Blood routine examinations of two cases in this report showed high lymphocyte ratio, significantly increased atyp-ical lymphocyte and liver damage, which were similar to infec-tious mononucleosis. However, EBV infection is common in chil-dren and adolescents, and liver is slightly damaged with ALT and AST slightly elevated [4] . For the two patients in this report, ALT was up to about 20 0 0 U/L, and AST was also significantly ele-vated. These results help us rule out infectious mononucleosis. With the characteristics of liver biochemistries in mind, we should pay more attention to the diagnosis of hepatitis instead of infec-tious mononucleosis. Moreover, we found that with the improve-ment of liver function, atypical lymphocytes were also decreased, which also indicate the diagnosis of hepatitis.
In summary, this report reviewed typical cases encountered in real life, combined with literature to improve understanding of the disease and reduce the rate of misdiagnosis. At the same time, early diagnosis and early isolation of patients can avoid large-scale epidemics.
Acknowledgments
None.
CRediT authorship contribution statement
Hai-Yan Sun:Data curation, Formal analysis, Writing –origi-nal draft.Hai-Jiang Tong:Methodology, Writing –review & edit-ing.Da-Wei Cui:Conceptualization, Funding acquisition, Supervi-sion, Writing –review & editing.
Funding
This study was supported by a grant from the National Natural Science Foundation of China ( 81871709 ).
Ethical approval
This study was approved by the Ethics Committee of the Shaox-ing Second Hospital. Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the sub-ject of this article.