COVID-19 pneumonia: A review of typical radiological characteristics
2021-11-01MarChurrucaElisaMartnezBesteiroFelipeCouagoPedroLandete
María Churruca, Elisa Martínez-Besteiro, Felipe Couñago, Pedro Landete
María Churruca, Elisa Martínez-Besteiro, Pulmonology Department, Hospital Universitario de La Princesa, Madrid 28006, Spain
Felipe Couñago, Department of Radiation Oncology, Hospital Universitario Quirónsalud Madrid, Madrid 28223, Spain
Felipe Couñago, Department of Radiation Oncology, Hospital La Luz, Madrid 28003, Spain
Felipe Couñago, Clinical Department, Faculty of Biomedicine,Universidad Europea de Madrid,Madrid 28670, Spain
Pedro Landete, Department of Pneumology, Hospital Universitario de la Princesa, Universidad Autónoma de Madrid, Madrid 28006, Spain
Abstract Coronavirus disease 2019 (COVID-19) was first discovered after unusual cases of severe pneumonia emerged by the end of 2019 in Wuhan (China) and was declared a global public health emergency by the World Health Organization in January 2020. The new pathogen responsible for the infection, genetically similar to the beta-coronavirus family, is known as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), and the current gold standard diagnostic tool for its detection in respiratory samples is the reverse transcription-polymerase chain reaction test. Imaging findings on COVID-19 have been widely described in studies published throughout last year, 2020. In general, ground-glass opacities and consolidations, with a bilateral and peripheral distribution, are the most typical patterns found in COVID-19 pneumonia. Even though much of the literature focuses on chest computed tomography (CT) and X-ray imaging and their findings, other imaging modalities have also been useful in the assessment of COVID-19 patients. Lung ultrasonography is an emerging technique with a high sensitivity, and thus useful in the initial evaluation of SARS-CoV-2 infection. In addition, combined positron emission tomography-CT enables the identification of affected areas and follow-up treatment responses. This review intends to clarify the role of the imaging modalities available and identify the most common radiological manifestations of COVID-19.
Key Words: COVID-19; Radiology; Chest X-ray; Lung ultrasonography; Computed Tomography; Positron emission tomography-computed tomography
INTRODUCTION
On 31 December 2019, 27 cases of pneumonia of unknown aetiology were identified in the city of Wuhan (Hubei Province, China). A new pathogen, genetically similar to the beta-coronavirus family to which the coronaviruses that caused previous epidemics belong - severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome (MERS-CoV) - was isolated from collected respiratory samples and named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). In January 2020, the World Health Organization named the disease Coronavirus disease 2019 (COVID-19) and declared a global public health emergency[1,2]. At the beginning of December 2020, a total of 65.8 million cases had been diagnosed, with 1.5 million confirmed deaths since the start of the pandemic[3].
The clinical presentation and radiological findings of COVID-19, as well as various diagnostic tools for its detection, have been widely described in multiple studies published throughout 2020. Regarding its clinical pattern, it is generally nonspecific and variable between individuals. In approximately 80%-90% of cases, the disease is mild or even asymptomatic. However, in the remaining approximately 10% of cases,generally frail patients with coexisting medical conditions develop a severe course of infection with dyspnoea, hypoxaemia and extensive radiological lung involvement[4] .The current gold standard diagnostic tool for the detection of SARS-CoV-2 RNA in respiratory samples is the reverse transcription-polymerase chain reaction (RT-PCR)test. This test shows a non-negligible rate of false negatives results, which can be attributed to errors in the extraction of nasopharyngeal swab sampling and when the sample is collected[5], since its sensitivity varies depending on the time since exposure. Thus, some studies estimate the sensitivity of the RT-PCR test to be 33% four days after exposure, 62% the day clinical manifestations begin and 80% three days after the onset of symptoms[6]. A combination of the growing and rapid spread of COVID-19 and the lack of RT-PCR testing kits in some affected areas has made new diagnostic and screening methods necessary[7]. Radiological diagnosis constitutes an essential component in the initial assessment of the extension and severity of the infection, as it is a key element to guide treatment and monitor the evolution of the condition[8]. So far, much of the literature has predominantly focused on characterising the radiological findings most frequently seen in chest computed tomography(CT). However, other diagnostic modalities, such as chest X-ray, lung ultrasonography(LUS) and combined positron emission tomography-computed tomography (PET-CT),have also been useful in the assessment and management of COVID-19 patients[5].
Ultimately, clinicians will choose an imaging modality based on its advantages, the experience gathered with each diagnostic method and the local resources available[9].This review aims to clarify the diagnostic value of the different imaging modalities available and describe the most common radiological findings in COVID-19.
CHEST X-RAY
Chest X-ray is a frequently used method due to its low cost and wide availability,allowing various conditions to be studied in a simple and fast manner.
Furthermore, the existence of portable X-ray devices has enabled its use in intensive care units (ICUs). It is important that clinicians understand both the advantages and limitations of this imaging technique in terms of diagnosing COVID-19 pneumonia[10].
Some studies have proposed that chest radiography is a useful method both for the diagnosis and follow-up of the lung pathology generated by SARS-CoV-2 infection.The American College of Radiology (ACR) defends the application of portable X-rays in order to avoid collapses in imaging departments and minimise the risk of contamination associated with the intra-hospital mobilisation of COVID-19 patients and thus the spread of the disease[11].
Studies published during 2020 report a low sensitivity of chest X-rays in detecting pulmonary infiltrates during the initial phases of COVID-19 infection, as well as in mild forms of the disease (Table 1)[12]. In this regard, in a retrospective study of 64 patients, Wong[13] noted a chest radiography sensitivity of just 69%, compared to 91% for the RT-PCR test, and highlighted that 9% of cases in which X-ray detected abnormalities were initially RT-PCR negative. Both Ng[14] and Kim[15]found that chest X-ray has a low sensitivity when it comes to identifying lung alterations caused by SARS-CoV-2 infection. However, at the beginning of February,Chen[16] published a study which found a sensitivity of 100% with the use of chest radiography, with 74/99 patients presenting bilateral pneumonia and 25/99 unilateral involvement. However, these results can be explained by the overload that the health system was experiencing at that time, when the radiological screening of positive COVID-19 patients was limited to severe and advanced cases. For these reasons, the European Society of Radiology and the European Society of Thoracic Imaging recommend avoiding its use as a first-line technique in the diagnosis of COVID-19 pneumonia, restricting its use to the follow-up of patients admitted to the ICU, whose fragility would make it difficult to transfer them for a chest CT scan[11].
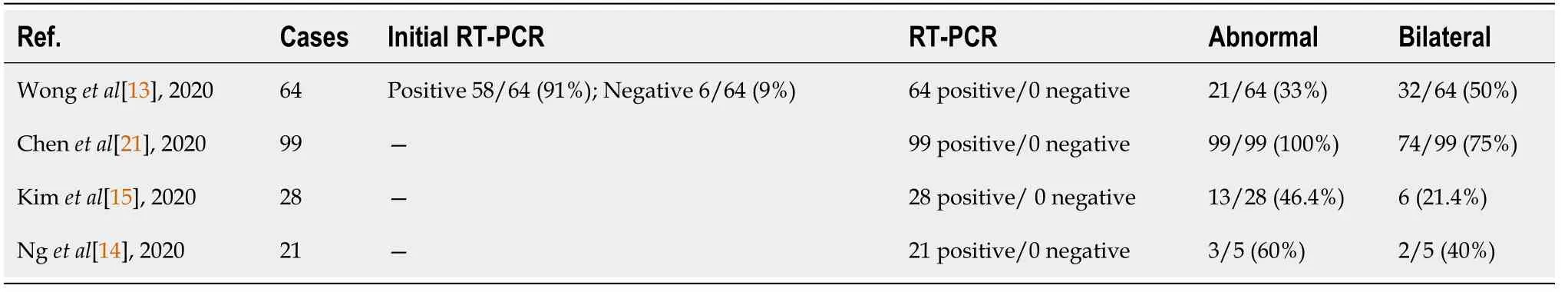
Table 1 Adapted from Chen et al[21] chest X-ray sensitivity in coronavirus disease 2019 pneumonia
The severity of COVID-19 pneumonia cannot be determined by a SARS-CoV-2-positive nasopharyngeal swab; therefore, it is necessary to conduct a complementary radiological study. Recently, Cellina[17] retrospectively studied the prognostic predictive value of radiographic imaging performed in the initial stages of the disease in 246 COVID-19 patients, establishing a significant correlation between lung parenchymal involvement - valued by a percentage of the areas affected by groundglass opacities (GGOs) or consolidation - and the severity of the disease.
The most common manifestations found in the chest radiographs of COVID-19 patients are GGOs - sometimes accompanied by reticular opacities - and lung consolidation, which, as in other atypical viral pneumonias, are typically multilobar and bilateral, generally involving the lower lobes (Table 2). One of the most specific signs of COVID-19 pneumonia is the peripheral and multifocal location of pulmonary infiltrates (Figure 1). Radiological impairments can rapidly evolve into a consolidative pattern, frequently reaching the peak of maximum severity and the worst pulmonary parenchymal involvement between 6-12 d after the onset of symptoms (Figure 2).Pleural effusion is extremely rare in patients infected by SARS-CoV-2, but if detected,is normally identified in the late stages of the disease. Lung cavitation images and pneumothorax are also unusual but can occur in some COVID-19 cases (Figure 3)[18].Lomoro[19] retrospectively studied the chest X-rays of 32 patients, describing consolidations in 46.9% of the cases and GGOs in 37.5%, without identifying pleural effusion in any of them. The distribution of these findings was predominately bilateral(78.1%) and unilateral only in 6.2% of the cases. Furthermore, the lower lobes were the most frequently affected (52%), followed by 34.4% of patients who presented similar involvement of both the upper and lower lobes, while just 3.1% presented involvement in the upper lobes.

Table 2 Most common findings of chest X-rays
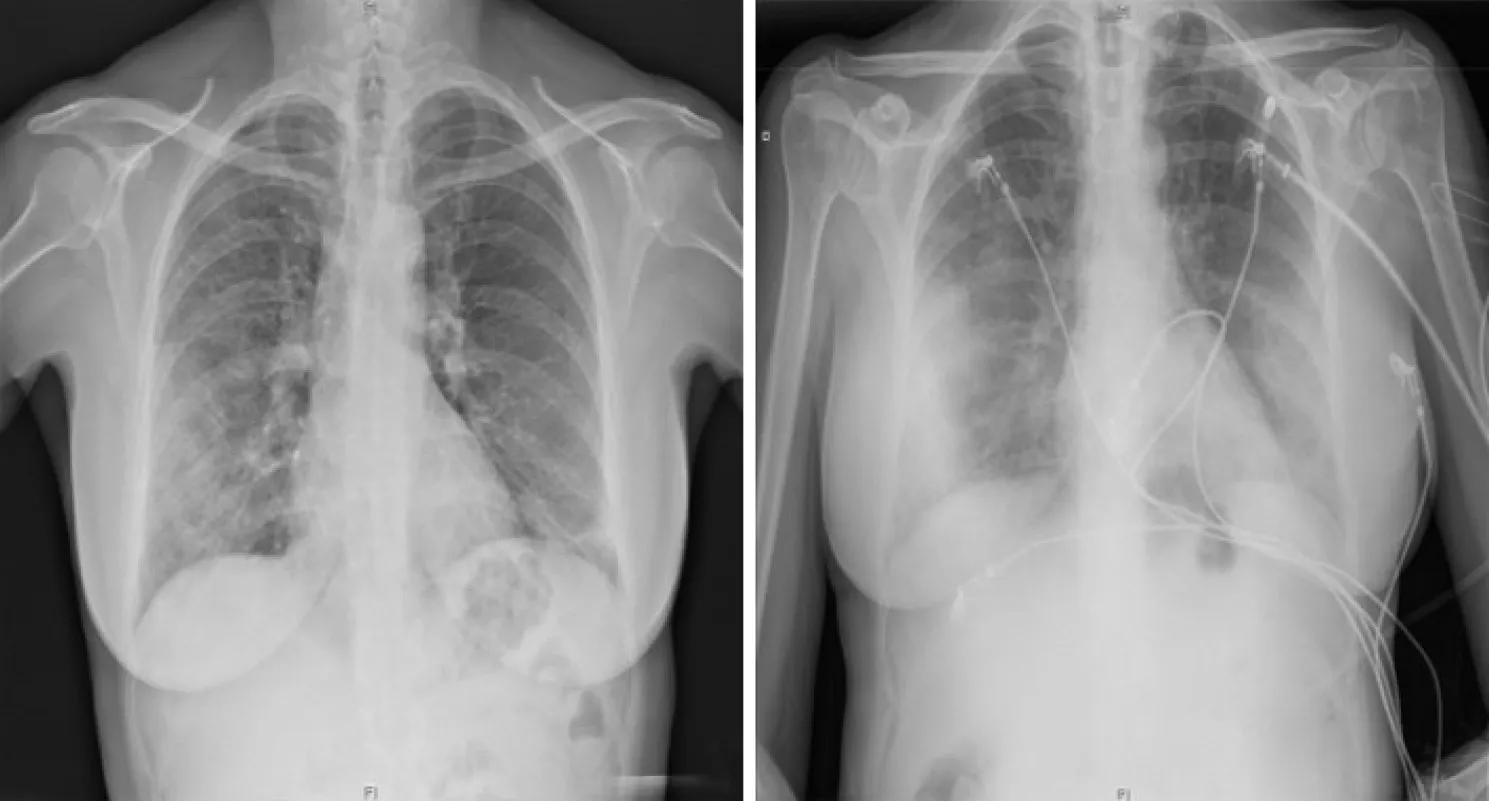
Figure 1 Chest X-ray findings in a 60-year-old woman with confirmed severe acute respiratory syndrome coronavirus-2 pneumonia(positive RT-PCR test). PA X-ray (left) with patchy right mid-to-lower and left lower lung opacities. AP X-ray (right) with peripherally distributed bilateral lung opacities.

Figure 2 PA Chest X-ray findings in a 55-year-old woman with varying degrees of coronavirus disease 2019 pneumonia defined by diffuse ground-glass and consolidative opacities, predominantly involving the lower zone in both lungs.
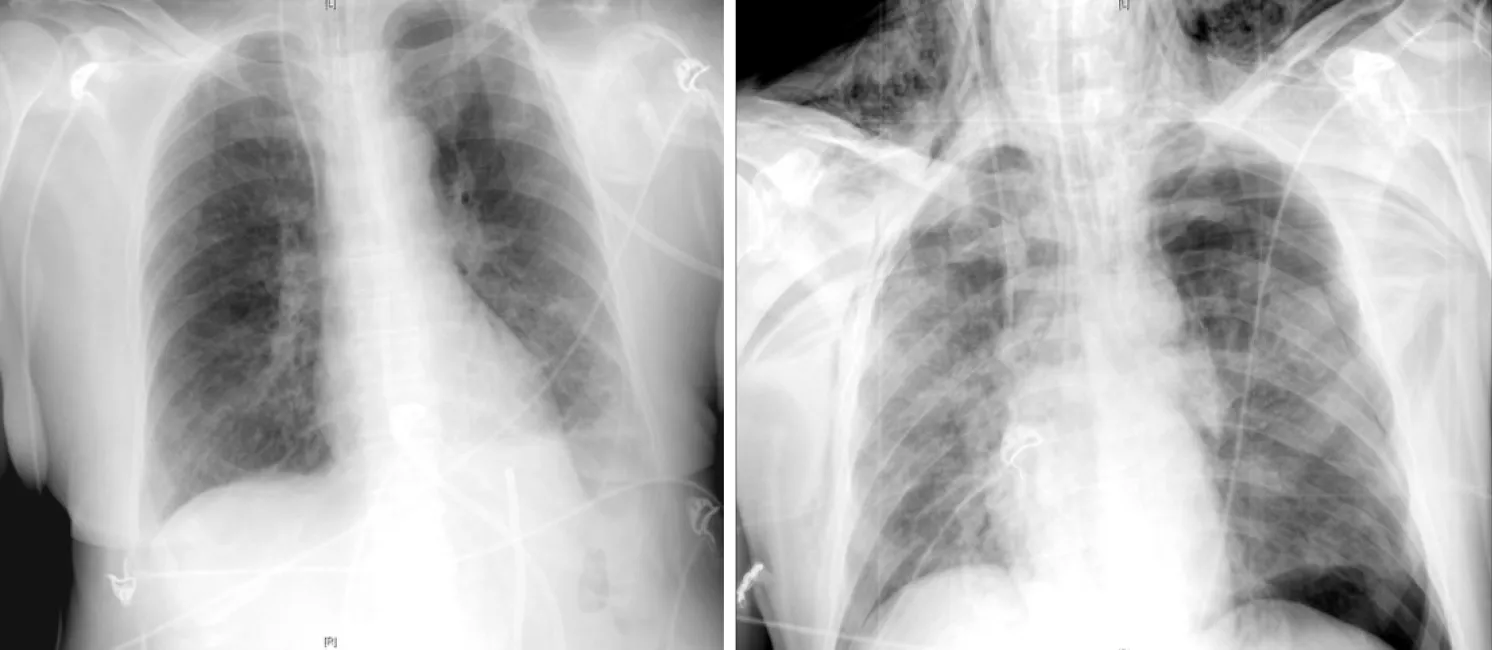
Figure 3 AP chest X-ray findings. AP chest X-ray findings (left) in an 80-year-old man with bilateral COVID-19 pneumonia and associated left pleural effusion.AP chest X-ray findings (right) in an 84-year-old man with bilateral alveolar infiltrates, diffusely distributed and left tension pneumothorax with subcutaneous emphysema.
The impact of pneumomediastinum and subcutaneous emphysema during the COVID-19 pandemic has been described by Lemmers[20], who detected these conditions in 13% of the patients in their study. While at the outset this was considered to be a consequence of the barotrauma produced by mechanical ventilation in critically ill respiratory patients, it is nevertheless believed that these findings could be attributed to the Macklin effect, characterised by the rupture of the pulmonary alveoli- fragile in these patients - which releases air that centripetally dissects through the pulmonary interstitium, reaching the mediastinum.
Ultimately, the published data suggest that chest radiography has a high utility in patients with SARS-CoV-2 infection, especially in those with moderate to severe pulmonary involvement and in the advanced stages of the disease. Moreover, it can serve as a first-line imaging tool when resources are limited, playing a key role in the monitoring of patients and the evaluation of eventual associated complications[21].
LUNG ULTRASONOGRAPHY IN THE COVID-19 ERA
Since the influenza A pandemic (H1N1) in 2009 and the avian influenza epidemic(H7N9) in 2013, LUS has become a significant diagnostic tool for the early detection of interstitial lung disease[22,23]. The current data published on COVID-19 support it as a safe and accessible emerging technique that can be applied to patients with either suspected or confirmed SARS-CoV-2 infection, both in the initial evaluation and the subsequent follow-up.
Traditionally, a healthy lung is considered invisible to ultrasonography. Since it is an aerated organ, it does not transmit ultrasound and therefore does not provide anatomical images. However, when lung tissue is occupied by fluid or cellular elements, its impedance varies resulting in artifacts that permit the identification of pathological findings.
The most basic of these artifacts aretransversal hyperechoic lines parallel to the pleural line - separated by a distance equal to that between the pleural line and the skin. They are the result of the reverberation of the pleural line in a healthy lung,representing normal lung aeration.
An additional and significant artifact in LUS are, which are described as vertical hyperechogenic artifacts that arise from the pleural line. They extend like a comet tail towards the deep parenchyma, hidingon their way and moving synchronously with pleural sliding[24]. They are considered to be the main ultrasound sign of interstitial lung disease, and their quantity increases as air content decreases and lung density intensifies. The presence of more than threeper intercostal space is considered pathological.
In normal conditions, the pleural line is hyperechogenic, thin and regular. However,in the presence of inflammation, thickening and/or fragmentation may occur if there are adjacent pulmonary consolidations. Additionally, there may be a decrease in pleural sliding.
One of the great advantages of LUS is its accessibility and immediacy, since it generates bedside and real-time images. Additionally, it is a non-invasive and innocuous technique that can be applied safely in certain population groups, such as pregnant women and paediatric patients.
Furthermore, LUS has a high sensitivity and outperforms chest X-rays in detecting the early stages of interstitial lung disease[25].
The main limitation of LUS is its operator-dependent nature, as its reliability is closely related to clinicians’ experience and ability. However, in experienced hands,the whole exploration can be performed in a few minutes, thus providing results faster in comparison with other imaging tests.
Lung ultrasound patterns in COVID-19
Before the outbreak of the COVID-19 pandemic, previous studies reported that LUS findings were highly consistent with chest CTs in patients with viral pneumonia[26].Similarly, in patients with SARS-CoV-2 pneumonia, there is a good correlation between both imaging techniques[27-31].
The common ultrasound findings described in patients with SARS-CoV-2 infection are summarised in Table 3 and Figure 4[32,33].
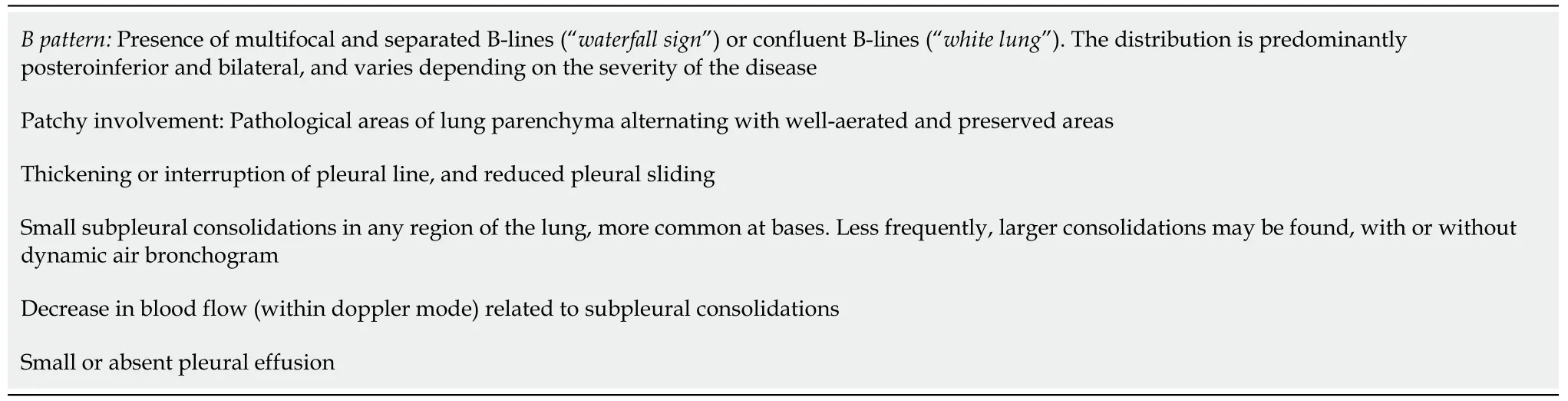
Table 3 Common ultrasound findings in coronavirus disease 2019
Gattinoni[34] describe two different ultrasound patterns in the hyperinflammatory phase of COVID-19: One phenotype of diffuse pulmonary infiltrates (type L),with normal or minimally decreased lung compliance, and therefore limited scope for alveolar recruitment, and a second phenotype of extensive consolidations (type H),with a low or very low compliance and with a clinical and prognostic behaviour analogous to the common acute respiratory distress syndrome (ARDS).
None of the findings described so far are pathognomonic for COVID-19; therefore,LUS cannot provide a confirmatory diagnosis. As such, it is essential to integrate the images with a clinical assessment and nasopharyngeal swab result.
Recently, some authors have discovered an unusual finding that could be more specific to COVID-19: The ‘[35]. This is a thick hyperechogenic band of confluentthat originates from a portion of the pleural line that is apparently preserved. It is usually found in the early stages of the disease and correlates with incipient GGOs on chest CT scan.
LUS findings vary depending on the stage of the disease (Figure 5)[36]. Thus, in the first days after the onset of symptoms, it is common to observe unilateral or bilateral focalAs the disorder progresses, the density of lung parenchyma increases along with the number of; diffuse and bilateralappear, starting from a pleural line that begins to thicken and becomes irregular, with small subpleural consolidations. Finally,may coalesce, creating a ‘white lung’ pattern of consolidation or hepatisation of the lung parenchyma - particularly in declining areas - with the respiratory failure that this implies.
Given its high sensitivity, LUS allows the detection of both deterioration and recovery in lung lesions during the final stage of the disease. Consequently, during the convalescent stage, there is a progressive regression ofand consolidations.Additionally,appear one again, in accordance with aeration improvement[31].
LUS is also efficient for the assessment of other events that, although not common,can occur in the course of SARS-CoV-2 pneumonia. These events include pleural effusion, pneumothorax - associated with mechanical ventilation or the insertion of a central venous catheter, among other causes - or a pulmonary embolism (PE). CT pulmonary angiogram remains the gold standard technique for the diagnosis of PE,but in critical, unstable patients with a suspected diagnosis, ultrasounds can provide valuable information on the presence of right ventricular dysfunction, acute pulmonary hypertension or deep vein thrombosis in the lower limbs.
Ultrasound scanning protocol
Evaluation of patients with acute respiratory failure using the Bedside Lung Ultrasound in Emergency Protocol (BLUE protocol), is one of the best-known applications of LUS[37]. In the particular case of COVID-19, one of its main challenges lies in standardising the technique to allow comparisons between study groups.
In clinical practice - and especially in ICUs - certain specific scanning protocols have been designed to quantify the extent of lung involvement by COVID-19[29,38-40]. We highlight the proposal of Soldati[38], which delimits seven explorationareas in each hemithorax, 14 zones in total. Each hemithorax is divided by three longitudinal lines - at the sternal, anterior and posterior axillary lines - and a transverse line at the nipple level, which separates a superior and an inferior area. Each one of the segments described receives a score between 0-3, according to the predominant findings in them, defining four different patterns (Table 4, Figure 4)[40].
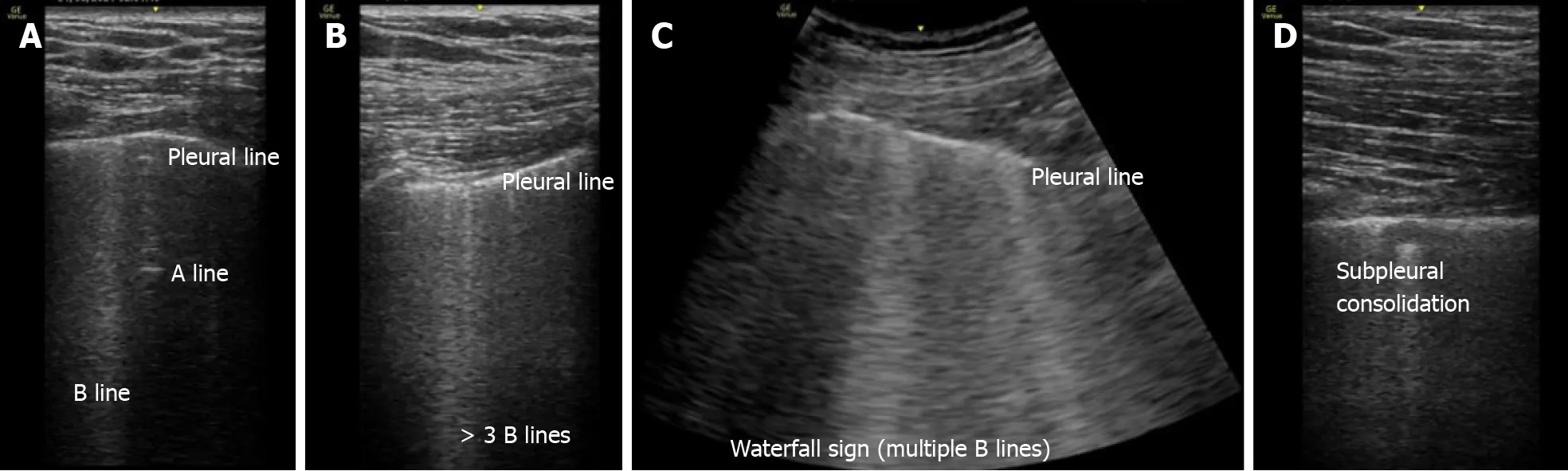
Figure 4 Images demonstrating the main changes in lung ultrasonography in coronavirus disease 2019 patients. A: Normal A-pattern with presence of 1 B line. B: Normal pleural line with presence of > 3 B lines. C: Irregular pleural line with coalescent B lines. D: Pleural involvement as sign of poor areation.
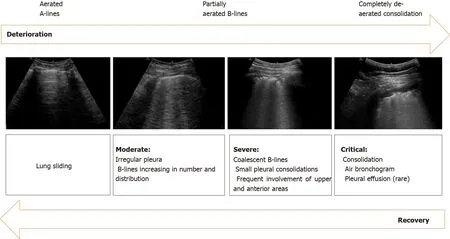
Figure 5 Sonographic characteristics of moderate, severe and critical pleural and parenchymal changes in patients with coronavirus disease 2019.
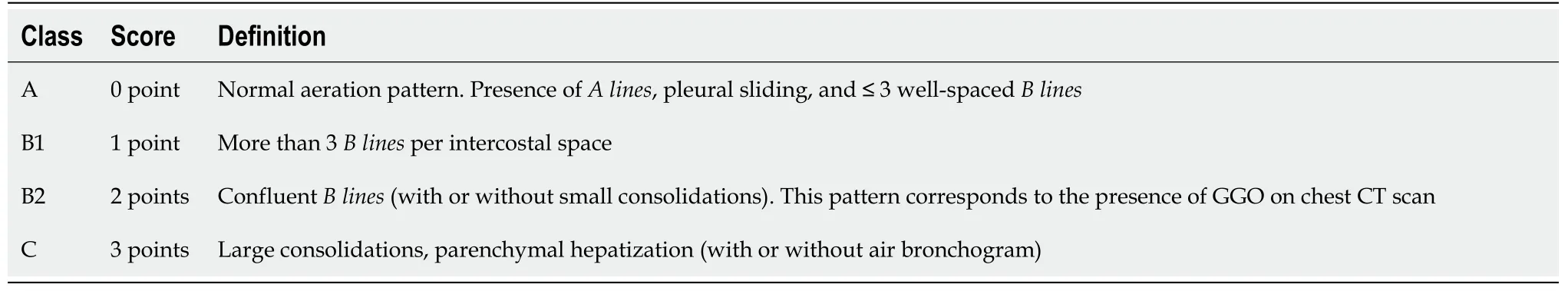
Table 4 Adapted from Vetrugno et al[39] proposal of lung ultrasonography score system in coronavirus disease 2019
At the end of the exploration, the score assigned to every explored area is accumulated, obtaining the final score. In the case of patterns B1 and B2, special attention must be paid to the pleural line, since the presence of pleural lesions is a severity sign that should be indicated by adding the letter ‘p’ to the score.
Ultimately, this scale allows the estimation of the extent of lung involvement in COVID-19 and provides clinical and prognostic information. Therefore, it could contribute to identifying those patients who require hospital admission, as well as to predict their response to certain therapies, such as prone positioning or mechanical ventilation. For example, the progressive reduction in the number ofthe reappearance ofor the regression of consolidations could suggest a favourable clinical evolution and support the decision to progress in the de-escalation of care.
A summary of the potential applications of LUS in COVID-19 pandemic is outlined below: (1) At triage: For risk stratification and initial screening of lung involvement in patients with suspected or confirmed SARS-CoV-2 infection; (2) In patients with symptoms consistent with COVID-19, but a negative nasopharyngeal swab (RT-PCR)and indeterminate chest X-ray: The presence of suggestive ultrasound findings could support the idea that the RT-PCR may represent a false-negative result; and (3) During hospital admission, to monitor the progression or regression of pulmonary lesions:Successive ultrasound explorations might result in accurate information that could be used to determine ventilation strategies and assess patients’ response to them. For example, those with posterolateral consolidations could benefit from early prone positioning[41,42], or lung aeration could be improved in those with coalescentby titrating positive end-expiratory pressure (PEEP). In addition, in critically-ill patients - respiratory or hemodynamically unstable - LUS could play a remarkable role in the early detection of complications, including superimposed bacterial pneumonia and pneumothorax, and as a guide for clinical decisions.
Therefore, LUS is becoming an increasingly valuable diagnostic tool due to its high sensitivity, safety, immediacy and accuracy. On this basis, it may play a key role in the management of patients with COVID-19. However, its low specificity for this pathology does not allow clinicians to distinguish COVID-19 from other viral infections. Therefore, LUS images must be evaluated in conjunction with clinical and microbiological data.
ROLE OF CHEST CT SCAN IN THE EVALUATION OF COVID-19 PNEUMONIA
Chest CT scan is a key element in the management of SARS-CoV-2 infection. It allows the detection of distinctive pulmonary manifestations, establishes their severity and enables the follow-up of their progression, differentiating early stages from more advanced ones based on the radiological findings identified. However, its role as a screening tool in COVID-19 pneumonia has yet to be fully defined[43].
Recent studies concerning COVID-19 pneumonia propose that chest CT is a more sensitive, practical and rapid diagnostic technique compared to the RT-PCR test,especially in the early stages of the disease (Table 5). Ai[44] reported a sensitivity for chest CT of 97%, taking RT-PCR as a reference, compared to 59% of RT-PCR performed in patients with suspected SARS-CoV-2 infection. However, chest CT specificity was only 25%. Furthermore, a meta-analysis conducted by Kim[45]produced similar results, with a higher chest CT sensitivity than the one found for RTPCR, 94% and 89%, respectively. However, a low specificity (37%) was encountered,which could be due to the fact that the nonspecific findings of COVID-19 pneumonia may overlap with those found in other viral pneumonias, so a high rate of false positives can be detected in chest CTs, especially in areas of low prevalence of the disease.

Table 5 Chest computed tomography and reverse transcription-polymerase chain reaction sensitivity in coronavirus disease 2019 pneumonia
Supporting these results, the Society of Thoracic Radiology, the ACR and the Radiological Society of North America recommend avoiding using chest CT as a routine screening test in patients with suspected SARS-CoV-2 infection[46]. Instead it should be saved for the assessment of symptomatic patients or those with a negative RT-PCR but high clinical suspicion, as it can help to characterise the disease by detecting typical pulmonary manifestations[47].
Thus, chest CT findings suggesting viral pneumonia, accompanied by a typical clinical presentation and compatible epidemiological data, should strongly indicate SARS-CoV-2 infection even though the RT-PCR may be negative[48].
There are currently few works on the use of artificial intelligence in the diagnosis of SARS-CoV-2. Although this technique could be useful in diagnosing COVID-19 pneumonia, there is little evidence so far to recommend it as a routine diagnostic approach[49].
Chest CT imaging features of COVID-19
SARS-CoV-2 infection causes direct lung damage through the angiotensin-converting enzyme. Interstitial pneumonia with alveolar edema in the early stages and diffuse alveolar damage in the most severe stages are the underlying pathological mechanisms responsible for the typical radiological images of COVID-19 pneumonia and its rapid progression[50,51].
A wide range of radiological findings have been reported in the multiple published studies (Table 6); however, the images may differ depending on the evolutionary stage of the disease. The main and most frequent finding of COVID-19 pneumonia is the presence of GGOs, typically subpleural (Figure 6)[52,53]. GGOs are defined as areas of slightly increased density without obscuration of bronchial and vascular structures,caused by a partial filling of the alveolar spaces and interstitial thickening. In an investigation conducted by Chung[53] with 21 COVID-19 patients, GGOs - being the most characteristic radiological finding in the early stages of the disease - were found in 57% of cases[54]. In accordance with these results, Pan[55] predominantly observed subpleural GGOs at the onset of the disease, with the subsequent development of a ‘crazy paving’ pattern and consolidations at two weeks of evolution.

Figure 6 59-year-old man with no clinical background and confirmed severe acute respiratory syndrome coronavirus-2 infection. Chest computed tomography imaging with peripherally distributed bilateral and multilobar ground-glass opacities.
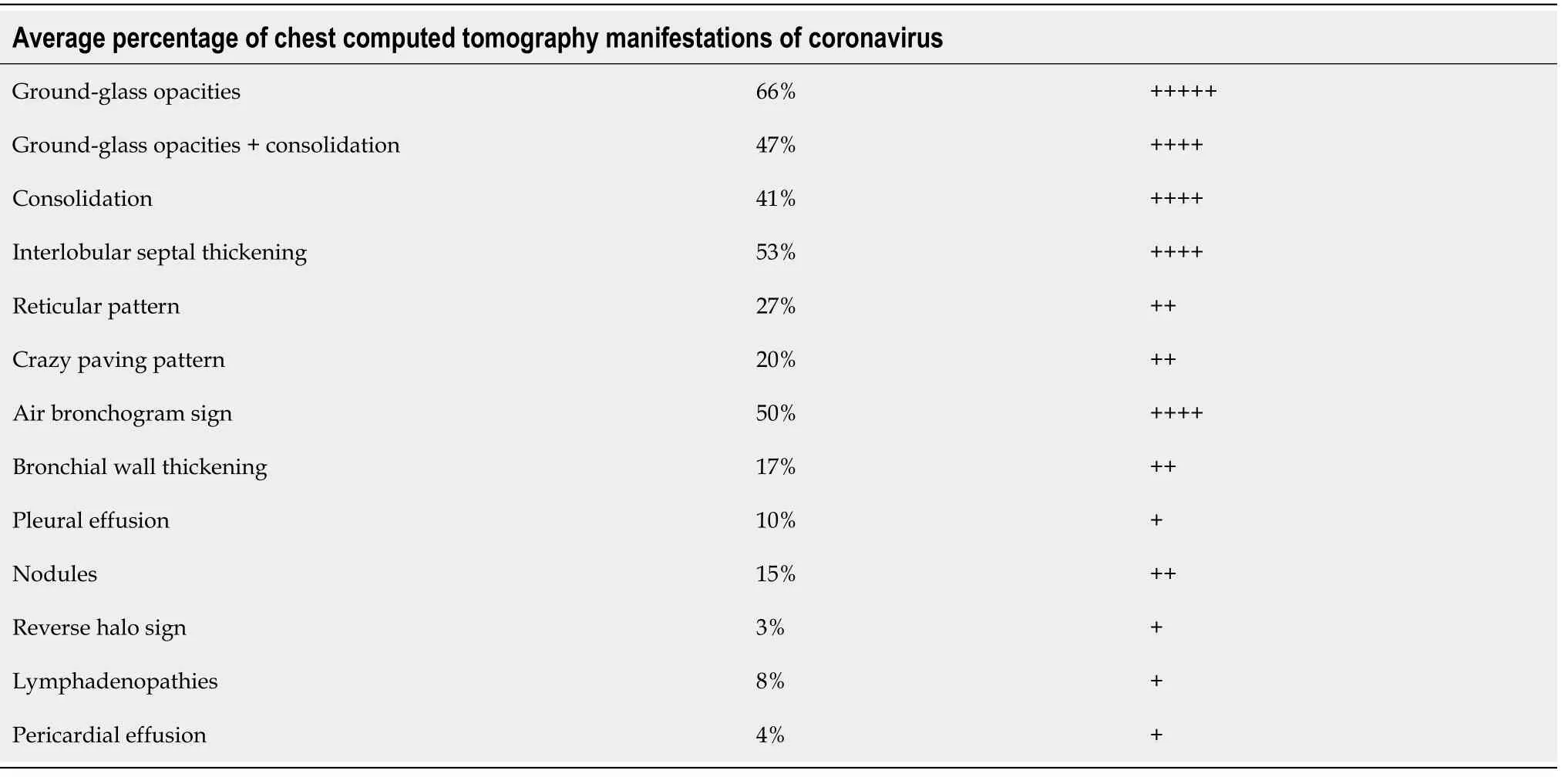
Table 6 Adapted from Carotti et al[57] average percentage of chest computed tomography manifestations of coronavirus disease 2019
Regarding the distribution of the radiological images encountered, a retrospective study of 101 patients[56] classified them as either bilateal (82.2%), peripheral (87.1%)or multifocal (54.5%), principally involving the lower lobes (54.5%) of the patients.These results are broadly in line with other published studies. In a study conducted by Salehi[57], pulmonary changes were bilateral (87.5%), with a peripheral distribution (76.0%) and a predominantly multilobar (78.8%) and posterior (80.4%)pulmonary infiltration.
Consolidation images have been described as the second most prevalent finding,reported in 2%-63% of cases. The involvement may be multifocal, patchy, or segmental, with a subpleural or peribronchovascular distribution. The development of this consolidation pattern may be in relation to the progression of the disease and can either coexist alongside or replace GGOs between week one to three of the clinical course, which could alert to the severity of the disease[55,58] (Figure 7).

Figure 7 45-year-old woman with coronavirus disease 2019-confirmed pneumonia. Chest computed tomography imaging. A: Bilateral and patchy ground-glass opacities involving upper and lower lobes. B: Crazy paving pattern involving upper and lower lobes. C: Alveolar consolidation mainly involving the lower lobes, with fibrous stripes associated.
Recent investigations have reported 5%-36% of COVID-19 patients with a crazy paving pattern on their imaging studies. This pattern refers to the appearance of GGOs with superimposed interlobular and intralobular septal thickening. While not observed as frequently as GGOs and consolidation, this pattern may be a sign that the disease is reaching its peak of maximum severity[54], which is described by Pan[55] as occurring 10 d after the onset of symptoms.
Other findings, such as the reverse halo sign (11.0%), the air bronchogram sign(14%), pleural thickening (15.0%), pleural effusion (4.0%) and the appearance of lymphadenopathies (2.7%), have been less frequently described[59]. Bronchial wall thickening and the presence of extrapulmonary lesions suggest severe inflammation and are characteristic of critical COVID-19 pneumonia (Figure 8)[60].

Figure 8 Unusual chest computed tomography findings in coronavirus disease 2019 pneumonia. A: Air bronchogram sign; B: Right paratracheal lymphadenopathy (marked) and right hilar lymphadenopathy; C: Pericardial effusion; D: Pleural effusion.
A reticular pattern associated with bronchiolectasis and irregular thickening of the interlobular septa has been identified with the progression of the disease, usually after the second week of evolution (Figure 9). These interstitial changes suggest the development of fibrosis. Pulmonary fibrosis is a relatively common consequence of ARDS. Approximately 40% of patients diagnosed with COVID-19 pneumonia are believed to develop ARDS, 20% of them severe. Although long-term studies have shown the existence of persistent interstitial alterations in patients who have suffered pneumonia due to other coronaviruses genetically similar to SARS-CoV-2 - SARS-CoV and MERS-CoV, first identified in 2002 and 2012 respectively[61,62], - the natural history of COVID-19 pneumonia has not yet been fully defined. Therefore, it is too early to classify these pulmonary changes as irreversible fibrotic changes, meaning that future prospective studies are necessary to confirm these preliminary results.

Figure 9 ReticuIar pattern and fibrous stripes showing coronavirus disease 2019 pneumonia in evoIution (> 2 wk after the onset of symptoms).
FLUORODEOXYGLUCOSE-POSITRON EMISSION TOMOGRAPHY IN COVID-19
PET-CT imaging with fluorodeoxyglucose (FDG) is a relevant and well-established diagnostic tool in tumoral pathology; in combination with CT, it provides anatomical and functional information that facilitates the study of tumoral extension and the evaluation of therapeutic response. This technique has also recently been gaining a certain importance in inflammatory and infectious pathologies. However, it has not yet been validated in this field and its use is not routinely recommended[63].
Several studies have suggested that PET-CT may be useful to evaluate the immune response to viral infections and their progression[64,65], since FDG uptake increases in neutrophils, lymphocytes, activated macrophages and granulocytes where there is inflammation. Therefore, it enables the localisation of where the immune response starts and how it develops.
Some authors have used PET-CT in animal models to study the development of viral infections, including MERS-CoV, H1N1, and HIV[66-68]. After exposure to the virus, in the absence of symptoms or abnormalities in chest CT scans, PET-CT is able to detect increased cellular metabolism in the lymph node stations directly involved in the lymphatic drainage of the lung tissue: the mediastinal and axillary nodes[66].Furthermore, this increase in FDG uptake is observed before massive viral replication occurs[68]; therefore, PET-CT could have a significant utility in early stages of infection.
In line with other inflammatory processes, the lung areas affected by COVID-19 show an increased FDG uptake (Figure 10)[69]. It has been postulated that there could be a correlation between greater FDG uptake and a slower progression towards improvement, as well as a higher erythrocyte sedimentation rate[70]. Various studies -which compare the findings of PET-CT and chest CT scans in COVID-19 patients -have also reported that despite the absence of lymphadenopathy in CT, PET-CT does detect an increased FDG uptake at the mediastinal and subclavicular lymph nodes[70-73]. Additionally, in some patients infected by SARS-CoV-2, mild inflammatory activity has been observed in the spleen and bone marrow, possibly in relation to a systemic inflammatory state. Finally, Lutje[74] proposed that PET-CT with FDG might help in detecting changes in other organs, including the heart, kidneys and gastrointestinal tract. However, all of the data published so far agree that the inflammatory process triggered by COVID-19 has a particular tropism for the lower respiratory tract.
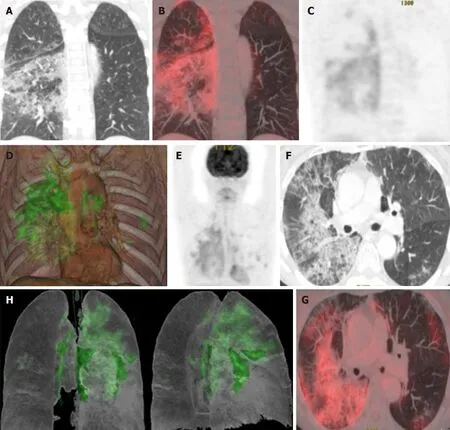
Figure 10 Taken from Landete et al[12], A 65-year-old patient with a history of invasive lepidic-predominant adenocarcinoma (stage pT1bNxM0) treated with surgery, chemotherapy and radiotherapy. A: Coronal computed tomography (CT) showing the crazy paving pattern with a markedly asymmetric bilateral distribution, mainly affecting the right side. B: Positron emission tomography-CT (PET-CT) coronal section. C: Metabolic PET. D:Volume rendering 3D PET-CT. E: MIP, PET. Images B-E reveal an increased cellular activity [standard uptake value (SUV) 4-6] related to the associated inflammatory process and a PET-CT pattern of bilateral coronavirus disease 2019 (COVID-19) with viral pneumonitis, predominantly right-sided. F: Axial CT showing crazy paving pattern with a bilateral, yet markedly asymmetric distribution, predominant right-sided. G and H: Axial section and 3D volume rendering from PET-CT metabolic imaging revealing increased cellular activity (SUV 4-6) related to the associated inflammatory process. PET-CT pattern of bilateral, predominantly rightsided, COVID-19 viral pneumonitis. Citation: Landete P, Quezada Loaiza CA, Aldave-Orzaiz B, Muñiz SH, Maldonado A, Zamora E, Sam Cerna AC, Del Cerro E,Alonso RC, Couñago F. Clinical features and radiological manifestations of COVID-19 disease. World J Radiol 2020; 12(11): 247-260. Copyright ©The Author(s)2020. Published by Baishideng Publishing Group Inc[12]”.
Preliminary studies have suggested that there is a certain correlation between the metabolic information provided by PET-CT and the degree of ventilation in different areas of the lung[75]. The collected data indicate that poorly ventilated areas of lung parenchyma show a greater FDG uptake than non-ventilated areas. This might mean that, within inflammatory processes, the better ventilated areas of the lung probably present higher infiltration by inflammatory cells[76].
PET-CT is not recommended as an initial test for diagnosing SARS-CoV-2 infection,as it involves greater irradiation to the patient than chest X-ray or chest CT scan, and the image acquisition periods are longer. Nonetheless, the structural and metabolic image that it provides could have an application in COVID-19 in the following situations[77]: (1) As a diagnostic tool for differential diagnosis in asymptomatic patients and in already diagnosed patients with a normal CT scan; (2) For monitoring responses to therapy, in combination with chest CT scan; (3) As a potential prognostic factor in the recovery stage of the disease; and (4) To evaluate extrapulmonary systemic involvement.
In conclusion, the studies published to date on the potential role of PET-CT in COVID-19 are limited. However, the existing data suggest that it may provide valuable information - complementary to the other imaging tests mentioned in this review - which helps to understand the pathophysiology of SARS-CoV-2 infection,define therapeutic strategies and assess the response to them.
CONCLUSION
Chest X-ray and CT play an important role in detecting abnormal lung changes, being the main imaging tests used to diagnose COVID-19 pneumonia. Other radiological modalities, such as lung ultrasonography and PET-CT, can provide further information for initial assessment and follow-up treatment response. Moreover, as we move through the pandemic, we believe that radiological findings of COVID-19 will be further explored, helping in determining diagnostic imaging features and guiding treatment.