Seroprevalence of anti-HBs antibodies and the need for booster vaccination in children under 5 years of age born to HBsAg-negative mothers
2021-10-23JannatinNisaArninditaMuhammadMiftahussururBagusSetyoboediJuniastuti
Jannatin Nisa Arnindita,Muhammad Miftahussurur,Bagus Setyoboedi,Juniastuti
1Medical School,Faculty of Medicine,Universitas Airlangga,Indonesia
2Department of Internal Medicine,Dr.Soetomo General Hospital/Faculty of Medicine,Universitas Airlangga,Indonesia
3Department of Pediatrics,Dr.Soetomo General Hospital/Faculty of Medicine,Universitas Airlangga,Indonesia
4Department of Medical Microbiology,Faculty of Medicine,Universitas Airlangga,Indonesia
ABSTRACT Objective:To determine the proportion of HBV surface antigen(anti-HBs) antibody positive children under five years of age born to HBsAg-negative mothers and to analyze the possible related factors following implementation of a hepatitis B vaccination program for infants in Indonesia 22 years ago.Methods:Blood samples were taken from children under five years of age born to HBsAg-negative mothers who have completed primary vaccination series.Anti-HBs antibodies were determined by using rapid test.Data of age,gender,nutritional status,vaccination timing or vaccination compliance,and booster vaccination were collected from vaccination card.Results:Ninety children were enrolled,consisting of 47 females and 43 males with a mean age of 2.3 years.Twenty two (24.4%)children received booster vaccine between 18 and 24 months and 55 (61.1%) were anti-HBs positive.Among factors of age,gender,nutritional status,compliance to vaccination and booster vaccine,only administration of booster vaccine was significantly associated with anti-HBs status (OR 5.45,95% CI 1.45,20.52).Children who received booster vaccine at age of 18-24 months were 5.45 times more likely to be anti-HBs positive than that of children who did not receive booster vaccine.Conclusions:Booster vaccine rate is low among children under 5 years of age but is associated with anti-HBs positivity.Booster vaccination may be required to improve anti-HBs seropositivity.
KEYWORDS:Hepatitis B vaccination;Booster vaccine;Children under five years
Significance
This study shows that less than two thirds of vaccinated children under five years of age are anti-HBs positive.Booster vaccine at age of 18-24 months is significantly associated with anti-HBs seropositivity.The administration of booster vaccines in accordance with national immunization policy should be routinely performed and monitored.
1.Introduction
Indonesia has been considered as a country with moderate to high hepatitis B endemicity[1].Prevention of hepatitis B infection in infants requires special attention because transmission from-motherto-child is the majority cause of the chronic infections,especially in countries with high level of endemicity such as Indonesia[2].The development of chronic infection is very common in infants infected from their mothers or by horizontal transmission before the age of five years[3].The younger the age at which the infection is acquired,the greater the predisposition to the carrier state,chronic liver disease and subsequent development of cirrhosis and hepatocellular carcinoma[4,5].Vaccination for infants and children is the most efficient method in providing long-term protection against hepatitis B virus (HBV) infection[6,7].
In 1992,the World Health Organization (WHO) established a goal for all countries with HBV carrier rates of over 8% to integrate hepatitis B vaccination into their routine immunization programs by 1995 and for all countries to establish such programs by 1997[8].Taiwan is perhaps one of the regions showing the best success from universal hepatitis B immunization,as reported that 9.8% children under 15 years old in Taiwan were HBV carriers[9],then 30 years after vaccination program (2004) had been implemented,the number significantly decreased to 0.9%[10].
In Indonesia,the universal hepatitis B vaccination program has been implemented since 1997 and it was reported that the prevalence of HBsAg decreased from 9.4% in 2007 to 7.2 % in 2013[1].In 1997,a recombinant hepatitis B vaccine replaced plasma-derived vaccine[11,12].In 1999,Indonesia introduced an innovative policy by using a prefilled single-use injection device of hepatitis B vaccine that is stable even when placed outside the cold chain.This approach has improved hepatitis B vaccine coverage and reduced hepatitis B carrier rates[13].In 2000,Indonesia introduced a program for using the device for the birth dose in seven provinces and in 2003 the program expanded to target all of Indonesia’s five million annual births[14].
Previous studies reported that some factors related to antibody against HBV surface antigen (anti-HBs) development after vaccination include age,gender,nutritional status,vaccination compliance and booster vaccination[15-19],however,similar studies in Indonesia are still limited.Data from Elementary Health Research,Indonesia showed that higher anti-HBs titer existed in male population than female,but age factor had higher significance with anti-HBs titer than gender factor[20].Difference in nutritional status also has an impact on anti-HBs (immune response) as reported that children with marasmus and kwashiorkor showed significantly poorer response than healthy children in Egypt[17].Currently,national program in Indonesia implements four weeks interval for each dose of vaccine primary series.A systematic study revealed that longer vaccination interval showed higher final anti-HBs concentrations while other studies conducted in Padang found no difference between different vaccination schedules[21,22].Booster vaccine was considered unnecessary in immunocompetent children after primary doses,while a recent study found that around more than a third of children who have received three doses of primary vaccine series were low and non-responders,thus needed additional booster vaccine[18,19].Plenty debates about vaccine schedules and doses are still ongoing while birth dose remained as a crucial determinant of vaccine immune reaction as children without birth dose proved to be 3.5 times more likely to be infected with hepatitis B[23].
Vaccination against HBV immediately after birth prevents neonatal infection which transmitted vertically by HBV carrier mothers[24].However,if the mother is HBsAg negative,the infant may still be exposed to HBV postnatally from another family member or caregiver.This occurs in two-thirds of the cases of childhood transmission,especially in high endemicity countries[25].A previous study showed that immunization of newborns does not only protect vaccinated children but also decreases horizontal transmission as children do not form a reservoir anymore for virus transmission at school and at home to susceptible adults[26].Meanwhile,children born to HBsAg-positive mothers showed high positivity of anti-HBs might be due to hepatitis B infection occur through vertical transmission[27],or simply there were some amounts of anti-HBs delivered[28].These children might also show poor immune response to HB vaccine due to hepatitis B immunoglobulin (HBIG)administration[29].
Sidotopo Wetan,a district in Surabaya (a capital of East Java province,Indonesia) has performed a national vaccination program and reached up to 99.78% coverage for hepatitis B vaccine in 2017 but it was ranked as the area with the greatest number (9.6% of 219 positive cases) of HBsAg prevalence in Surabaya[30].The aim of this study was to determine the proportion of anti-HBs positive in children under five years of age born to HBsAg-negative mothers who have completed primary hepatitis B vaccination series in Sidotopo Wetan and to analyze the possible related factors.
2.Subjects and methods
2.1.Ethical approval
Ethical clearance of this study was obtained from Ethical Committee of Faculty Medicine,Universitas Airlangga,Indonesia(No.100/EC/KEPK/FKUA/2019).Written informed consent was obtained by the parents or guardians of each child.
2.2.Sample and data collection
In this cross-sectional study,children aged 1-<5 years who attended Sidotopo Wetan Primary Health Care were enrolled.Participants recruitment,sample and data collection were conducted from May to July 2019.Inclusion criteria were children who have completed hepatitis B primary vaccination series (four doses) which was recorded in the vaccination card.Exclusion criteria were children born to HBsAg-positive mothers or received HBIG after birth.A total of 100 participants was obtained,but it was eliminated into 90 samples due to missing data in their vaccination cards.
Data obtained from vaccination cards include age,gender,nutritional status (WHO weight/age chart),vaccination timing orvaccination compliance with a schedule of 0,2,3,4 months in age(based on national vaccination program),also booster vaccination[31].
Capillary blood samples were drawn using finger-prick method and examined the anti-HBs status using MONOTESHBsAb Rapid Test Cassette (PT.Bintang Mono,Tangerang,Banten,Indonesia).Approximately 5-10 drops amount of blood was transferred to the cassette then the result appeared after 15-30 minutes.The sample was considered positive if anti-HBsAg ≥10 mIU/mL.
2.3.Statistical analysis
Statistical analysis was performed using The IBM SPSS®software (Statistical Package for Social Sciences,Inc.,Chicago,IL)using Fisher's exact test and logistic regression test.The obtained association was further analyzed using odds ratio.P
≤0.05 was considered to indicate a statistically significant difference.3.Results
A total of 90 children under five years of age born to mothers with HBsAg negative were enrolled,consisting of 47 (52.2%) females and 43 (47.8%) males with a mean age of 2.3 years.A total of 55 children (61.1%) were anti-HBs positive and the rest (38.9%) were anti-HBs negative.There was a fluctuation of percentage of anti-HBs-positive children to age range respectively as follows:61.3%in those aged 1-<2 years,70.6% in those aged 2-<3 years,50.0% in those aged 3-<4 years and 68.8% in those aged 4-<5 years (Table 1).

Table 1.Characteristic and vaccination data of all 90 children.
Characteristics (age,gender,nutritional status) and vaccination information (compliance and booster vaccine) of the children based on age range were shown (Table 1).The majority of the children were classified as normal-weight (65.6%),followed by underweight(25.6%) and severely underweight (8.9%).No child was obese.Most children (65.6%) were not vaccinated on a schedule and variations in the timing of vaccine administration are shown in Table 2.Besides,most children (75.6%) did not receive booster vaccine at age 18-24 months (Table 1).
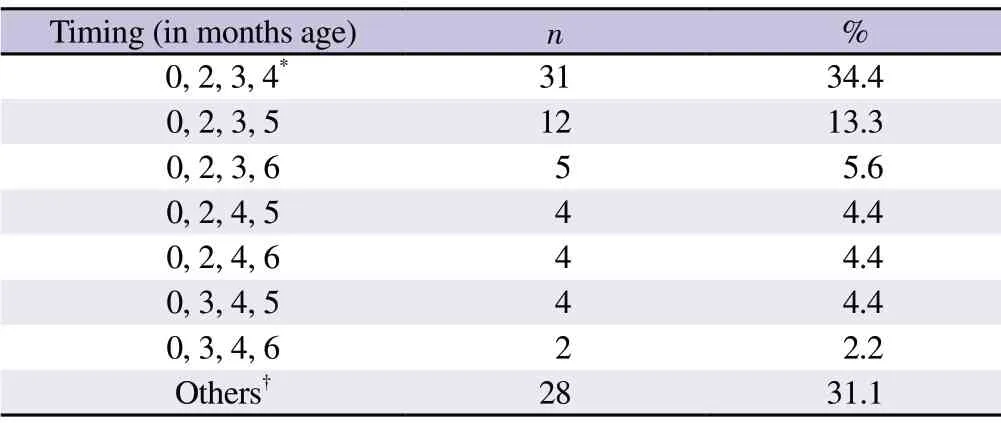
Table 2.Vaccination timing variation of samples.
Among those factors (age,gender,nutritional status,compliance to vaccination,and booster vaccine),only administration of booster vaccine at age of 18-24 months was significantly associated with anti-HBs status (P
=0.012).Children who received booster vaccine at age of 18-24 months was 5.45 times more likely to have anti-HBs positive than those who did not receive booster vaccine (P
≤0.05,OR
5.45,95%CI
1.45,20.52) (Table 3).Based on age groups,the seropositivity rate of anti-HBs in children who received booster vaccine ranged 60%-100%,greater than that in children who did not receive booster vaccine (range 42.9%-75.0%) (Table 4).The coverage of booster vaccine was only about 18.8%-29.4% in all age groups and most children received only one booster dose (Table 3 and 4).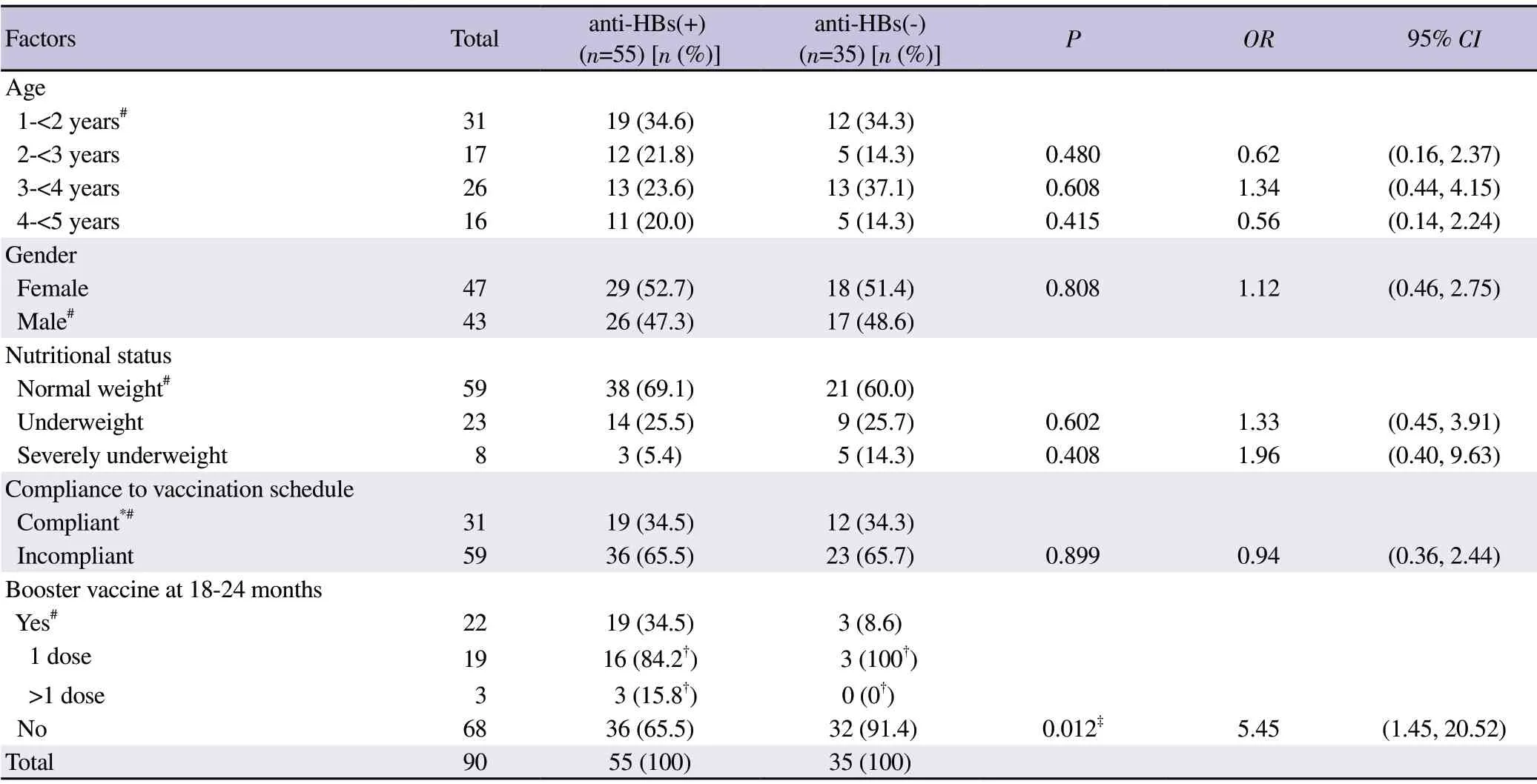
Table 3.Binary logistic regression analysis of variables for association with anti-HBs seropositivity of all children.
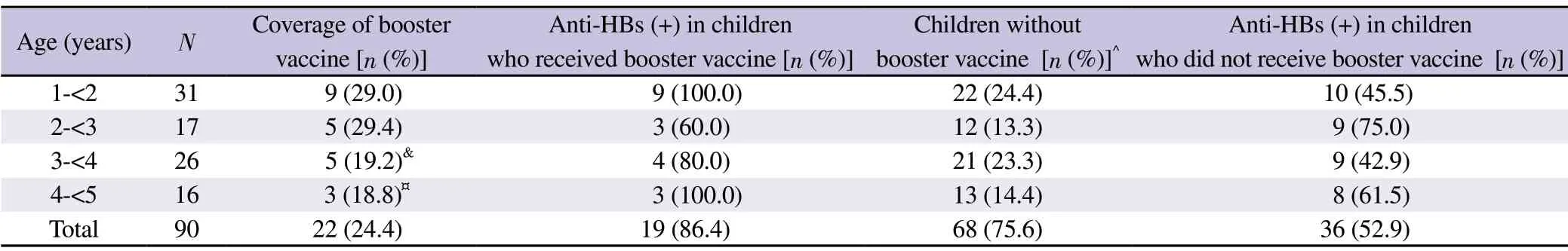
Table 4.Coverage of booster vaccine and anti-HBs seropositivity in children who received booster vaccine and those who did not receive booster vaccine according to age range.
4.Discussion
According to the national immunization policy in Indonesia,the single birth dose of the hepatitis B vaccine should be given withinseven days after birth and should be followed by three doses of combined vaccines including diphtheria,pertussis,tetanus and hepatitis B within the 2nd,3rd,and 4th months (DPT-HB3)[32].The policy also recommends the implementation of varied vaccine booster doses between 1 and 3 doses,with one booster dose implemented in national program,while children in certain area could receive 1-2 more booster doses when there was an outbreak of diphtheria,pertussis,tetanus,hepatitis B orHaemophilus influenzae
.Hepatitis B vaccination succeeded in covering a large population as it reached 91.7%,surpassed the target by 90% in 2017 in Indonesia[33].In the study in Sidotopo Wetan district,among 90 vaccinated children under five years of age born to HBsAg-negative mothers,only 61.1% of them appeared to be positive for anti-HBs.Similarly,the previous study held in Yogyakarta,Indonesia involving 57 infants and children aged five months-five years reported that protective anti-HBs titer was only shown by 73.1% samples[34].These data contradicts data from WHO which showed that more than 95% infants,children,and adolescents who have completed hepatitis B vaccination doses will remain positive for anti-HBs for at least 20 years[3].Due to the discrepancy,we investigated the possible factors influencing the low seropositivity of anti-HBs in this study.
This study showed fluctuating trend of anti-HBs-positive children percentage by age range (no significant difference) as follows:61.3%in those aged 1-<2 years,70.6% in those aged 2-<3 years,50.0% in those aged 3-<4 years and 68.8% in those aged 4-<5 years.It differed from a previous study in children aged eight months-five years in Bantul city,Indonesia,which reported that anti-HBs seropositivity was negatively correlated with age,although the correlation was weak.The seropositivity rate (anti-HBs ≥10 mIU/ mL) in children aged one year was 100% and in children aged 5 years was 37%[35].The results of another study in Taiwan showed that the seropositivity rate of anti-HBs declined from 99% at one year of age to 83% at 5 years of age[36] and further dropped to 71.1% at 7 years of age,37.4% at 12 years of age and 37% at 15-17 years of age[37].Further investigation is needed towards the unexpected result in Sidotopo Wetan.Some potential factors such as host (e.g.
comorbidities),extrinsic (e.g.
preexisting immunity,infections) and vaccine (e.g.
vaccine strain and vaccine quality) could be considered[38].No statistically difference between gender and anti-HBs seropositivity observed in this study,which was similar to other studies[39-41].Kwon and Jeong added that there was no statistically significant difference in the anti-HBs seropositivity rate based on gender in any age groups[41].
The immune status of an individual is well known as an important factor influencing antibody production.Our study showed that more children with normal weight (69.1%) performed anti-HBs positive than underweight/severely underweight children (P
>0.05).Similar results by other studies in varied population[42-44] reported that children with anti-HBs positive had better nutritional status compared to children in non-reactive group,but not significantly different.However,Kwon and Jeong showed a significant correlation between anti-HBs titer and body mass index (BMI) after the adjustment for age and sex.They indicated that BMI is a potential factor affecting anti-HBs titer in healthy children[41].Variation and limitation of those studies might contribute the obtained results.WHO recommended universal provision of three doses of hepatitis B vaccine for infants and universal birth dose vaccine.The birth dose of hepatitis B vaccine can be given only as monovalent hepatitis B vaccine,as diphtheria,pertussis,and tetanus vaccine is not recommended before the age of four weeks[45].However,there has not been any standard vaccine schedule.Different countries apply varied hepatitis B schedules in their national vaccination program,for instance in China,hepatitis B vaccination is given in three separated doses for infants aged 0,1,and 6 months,while in Germany,it is given in four separated doses for infants aged 2,3,4,and 11-14 months[46,47].Indonesia prioritizes compliance and completeness of vaccine administration in consecutive months at age 0,2,3,and 4 months then followed by booster vaccine at age 18-24 months.Most children (65.6%) in Sidotopo Wetan were not vaccinated on schedule.More children who were not vaccinated on schedule (65.5%) had anti-HBs positive than children who were vaccinated on schedule (34.5%) although there was no significant difference between schedule and anti-HBs seropositivity.In previous reports,no apparent effect on immunogenicity has been documented when minimum spacing of doses is not achieved precisely,while increasing the interval between the first two doses has little effect on immunogenicity or final antibody concentration.The third dose confers the maximum level of seroprotection but acts primarily as a booster and appears to provide optimal long-term protection.Longer intervals between the last two doses result in higher final antibody levels but might increase the risk for acquisition of HBV infection among persons who have a delayed response to vaccination[48].
CDC reported that after primary hepatitis B vaccination,anti-HBs concentrations declined rapidly within the first year and more slowly thereafter[48].A cohort study of hepatitis B vaccine in an endemic area of hepatitis B suggested to offer a second booster,five years after the first booster (one year after primary vaccination) to reach maximum protection[49].Booster vaccine can significantly increase anti-HBs titer in individuals who did not respond to hepatitis B vaccination and restore decreased anti-HBs to provide long-term protection against HBV[3,50,51].Booster vaccine is proved to further stimulate T follicular helper cells (Tfh) to produce more B cells and antibody against hepatitis B infection[52].When immune memory was present,the anti-HBs responses could be induced as early as one week following a booster,and such responders were likely to have protective titers after a single dose.The production of anti-HBs titers ≥10 mIU/mL one month after booster vaccination may result from either a primary immune response or anamnestic response[53].A previous study revealed that one dose of booster vaccine was enough to restore lost antibody while another study indicated that three booster doses were required to give seroprotection against HBV infection[50,54].Even primary dose vaccines alone had been proved to decrease HBsAg prevalence,some studies failed to prove that increased anti-HBs seroconversion after booster vaccine would decrease HBsAg prevalence[9,55-57].Recommendations on booster vaccine in children are still lacking.
In Indonesia,booster vaccination has been routinely recommended in children aged 18-24 months between 1 and 3 doses,with one booster dose included in national program[32];however,data explaining the protection of booster vaccine has not yet been available.This study showed administration of booster vaccine was significantly associated with anti-HBs status (P
=0.012).A number of children received booster vaccine were around 5.45 times more likely to have anti-HBs positive.The greater seropositivity rate of anti-HBs was also seen in almost all age groups of children who received booster vaccine.However,it should be concerned why a minimum of one booster vaccine has not been implemented well in all age groups (range 18.8%-29.4%).They did not receive any booster vaccine until at the time of the study.This condition might contribute the finding of low percentage of anti-HBs positive.There are some limitations in this study.This is only a pilot study.This study does not show the long-term follow up data (especially related with booster vaccine),therefore,the trend and the persistence of vaccine response (anti-HBs) by age could not be established well.Besides,only some factors associated with immune response to vaccine were evaluated.More other factors (not only host factors)such as extrinsic factors (e.g.
preexisting immunity and infections/comorbidities) and vaccine factors will provide more comprehensive data.Furthermore,this study included participants in an area.It requires a surveillance study to assess hepatitis B vaccine protection(vaccine effectiveness) with a larger sample size in other regions.In conclusion,only 61.1% vaccinated children born to HBsAgnegative mothers showed anti-HBs positive.Among factors of age,gender,nutritional status,compliance to vaccination and booster vaccine,only administration of booster vaccine was significantly associated with anti-HBs status.Accordingly,it was suggested to perform booster vaccine routinely according to the recommendation of the national immunization policy.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Authors’ contributions
J and JNA designed this study.JNA conducted data collection and laboratory examination.J and JNA analyzed and interpreted the data and also drafted the manuscript.J,MM and BS contributed to the critical revision of the manuscript.All authors contributed to the final version of the manuscript.J supervised this study.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Healthy tourism initiative in the age of COVID-19 in Indonesia
- Wolbachia-infected mosquitoes:The answer to the dengue endemic in Pakistan?
- Foodborne parasitic diseases in China:A scoping review on current situation,epidemiological trends,prevention and control
- Predictive modeling of 30-day readmission risk of diabetes patients by logistic regression,artificial neural network,and EasyEnsemble
