Associations of accelerometer-determined physical activity and sedentary behavior with sarcopenia and incident falls over 12 months in community-dwelling Swedish older adults
2021-10-09DvidScottJonsJohnssonAnoohyGndhmPtrEblingPtrNordstromAnnNordstrom
Dvid Scott,Jons Johnsson,Anoohy Gndhm,Ptr R.Ebling,Ptr Nordstrom,Ann Nordstrom
a Department of Medicine,School of Clinical Sciences at Monash Health,Monash University,Clayton,VIC 3168,Australia
b Department of Medicine and Australian Institute of Musculoskeletal Science,Melbourne Medical School-Western Campus,the University of Melbourne,St Albans,VIC 3021,Australia
c Department of Public Health and Clinical Medicine,Section of Sustainable Health,Umea° University,Umea° SE-901 87,Sweden
d Department of Community Medicine,UiT the Arctic University of Norway,Tromsø 9010,Norway
e Department of Community Medicine and Rehabilitation,Geriatric Medicine,Umea° University,Umea° SE-901 87,Sweden
f School of Sport Sciences,UiT the Arctic University of Norway,Tromsø 9010,Norway
Abstract Purpose: This study was aimed to determine associations of accelerometer-determined time and bouts of sedentary behavior, light physical activity(LPA),and moderate-to-vigorous PA(MVPA)with sarcopenia and incident falls over 12 months.Methods: A total of 3334 Swedish 70-year-olds were assessed for sarcopenia, as defined by the revised definition of the European Working Group on Sarcopenia in Older People.Assessments were based on low scores for appendicular lean mass (dual-energy X-ray absorptiometry),hand grip strength,and the Timed Up and Go test.For 7 days after baseline,total time and total number of bouts(≥10 min of continuous activity at a given intensity) of activity performed at sedentary, LPA, and MVPA intensities were assessed by accelerometer.Incident falls were self-reported 6 months and 12 months after baseline.Results:Only 1.8%of participants had probable or confirmed sarcopenia.After multivariable adjustment for other levels of activity,only greater MVPA time was associated with a decreased likelihood of having low appendicular lean mass,low hand grip strength,and slow Timed Up and Go time as defined by the European Working Group on Sarcopenia in Older People criteria(all p<0.05),and only MVPA time was associated with lower likelihood of probable or confirmed sarcopenia(odds ratio=0.80,95%confidence interval:0.71-0.91 h/week).Similar associations were identified for total number of bouts,with no evidence of threshold effects for longer duration of bouts of MVPA.A total of 14%of participants reported ≥1 fall,but neither total time nor bouts of activity was associated with incident falls(all p>0.05).Conclusion: Higher amounts of accelerometer-determined MVPA are consistently associated with a decreased likelihood of sarcopenia and its components,regardless of the length of bouts or amounts of sedentary behavior.
Keywords: Accelerometer;Falls;Older adults;Physical activity;Sarcopenia
1.Introduction
Sarcopenia, a muscle disease arising from adverse muscle changes accruing across the lifetime, recently received an updated operational definition from the European Working Group on Sarcopenia in Older People (EWGSOP).1The revised EWGSOP definition (EWGSOP2) differs from the original one (EWGSOP1) in terms of suggested measurements, cut-off points, and case-finding algorithms.In EWGSOP2, physical performance assessments are used only to assess the severity of sarcopenia.This is in contrast to EWGSOP1, where physical performance was a primary component of sarcopenia, and to the definition given by the U.S.Foundation for the National Institutes of Health, where physical performance is considered an outcome of sarcopenia.2These different approaches may partly explain controversial findings in terms of the relationships between sarcopenia and falls in older adults.3Nonetheless, we recently reported that older adults with sarcopenia,as defined by the EWGSOP2,are more than twice as likely to experience falls over 12 months compared with those without sarcopenia.4
Current World Health Organization physical activity (PA)guidelines recommend that adults 65 years and older complete 150 min/week of moderate PA, 75 min/week of vigorous PA,or an equivalent amount of combined moderate-to-vigorous PA (MVPA), with aerobic activities performed in bouts (continuous activity performed above the MVPA threshold)5of≥10 min.6Accelerometers are a useful tool for objectively estimating total duration and total bouts of sedentary behavior,light PA(LPA),and MVPA.We previously reported that total amount and intensity of accelerometer-determined PA is positively associated with lean mass and muscle strength in older adults, whereas sedentary behavior demonstrates inconsistent associations.7Despite concerns that greater amounts of MVPA may expose older adults to an increased risk of falls, older women with low accelerometer-determined MVPA demonstrate increased falls rates.8It is unclear whether the length of bouts of different activity intensities influences their associations with sarcopenia and falls, so determining whether a threshold effect exists is important for public health messaging.
Exercise, particularly resistance training, is recommended as the primary treatment strategy for sarcopenia,9and functional activities and balance training seem to be key for the prevention of falls.10While strength training is recommended in current PA guidelines, they focus primarily on general PA rather than targeted exercise.11It is therefore important to understand associations of general PA with sarcopenia and falls.The aim of this study was to determine associations of accelerometer-determined total duration and number of bouts of sedentary behavior, LPA, and MVPA with EWGSOP2-defined sarcopenia and its components, as well as their associations with incidence of falls over 12 months.
2.Materials and methods
2.1.Study design and participants
The Healthy Ageing Initiative is an ongoing observational study of 70-year-old adults residing in the Umea°municipality in northern Sweden.The primary objectives of the Healthy Ageing Initiative are to investigate traditional and novel risk factors for cardiovascular disease and injurious falls and fractures in 70-year-old men and women.Only 2 eligibility criteria apply: specifically, that the individual is residing in the Umea°municipal area and is 70 years of age at the time of testing.Potentially eligible individuals were sent written information about the study,with contact information drawn from population registers.Individuals either accepted or declined to participate during a follow-up phone call.The study participation rate was 69.5%.The Healthy Ageing Initiative was approved by the Umea°University Research Ethics Committee and complied with the World Medical Association’s Declaration of Helsinki.All participants provided written informed consent.The current analysis included the first 3334 participants with complete data for demographics, components of sarcopenia,and accelerometer-determined PA.
2.2.Baseline clinic appointment
Participants attended a hospital near Umea°University for a baseline clinic appointment, where they completed assessments (detailed elsewhere in this article) and also had fasting blood tests from which plasma glucose was analyzed.Height and weight were assessed by stadiometer (Holtain Limited,Crymych, Dyfed, UK) and scales (Avery Berkel HL 120,Smethwick,West Midlands,UK),respectively,and body mass index (BMI; kg/m2) was calculated.Participants also completed a questionnaire that assessed demographics, lifestyle,and medical history.A Lunar iDXA (GE Healthcare Lunar,Madison,WI,USA)whole body scan was performed to assess soft-tissue composition (total fat mass and appendicular lean mass (ALM)).Hand grip strength (HGS) was assessed using an isokinetic hand dynamometer (Jamar; Patterson Medical,Warrenville, IL,USA).Research nurses instructed the participant to hold the hand dynamometer in their nondominant hand, maintain a 90° angle at the elbow joint, and keep the elbow in close proximity to the waist.The research nurses further instructed the participant to,on command,start squeezing the hand dynamometer as forcefully as possible.The best of 2 attempts was subsequently recorded.The Timed Up and Go(TUG) test12was performed once to assess physical performance; participants were asked to rise unaided from an armchair and walk forward 3 m,then to turn around and return to a seated position in the chair.Research nurses provided instructions and a demonstration of the task, and measured TUG time using a stopwatch.
2.3.Accelerometer-determined PA
Participants wore a triaxial accelerometer (GT3X+; Actigraph,Pensacola,FL,USA)for 7 days after the clinic appointment as described previously.13Participants were instructed to wear the accelerometer on their nondominant hip and to remove it only when showering,swimming,or in bed at night.To obtain representative accelerometer measurements,participants were also instructed to be normally active in accordance with their current lifestyle.Participants who did not provide≥4 days (including ≥10 h/day) of valid measurements had accelerometer data excluded (approximately 10% of participants were excluded due to nonvalid wear time).14Accelerometer data were collected at a frequency of 30 Hz,and data were transformed into counts of movement with an activity threshold of 100 counts per min (cpm).Collected data were downloaded using ActiLife software (Version 6.11.2; Actigraph,Pensacola,FL,USA)in epoch lengths of 60 s,with subsequent wear time validation performed.Periods of ≥60 min with 0 activity were marked as nonwear time.Sedentary behavior was classified as 1-99 cpm,LPA was classified as 100-1951 cpm,and MVPA was classified as ≥1952 cpm,as proposed by Freedson et al.15MVPA was calculated as the sum of moderate and vigorous PA; these PA intensities were combined due to low amounts of vigorous activity in this cohort.16Total time(h/week)was calculated for each activity threshold,as well as the total number of bouts (instances of continuous activity within the respective activity threshold for each of sedentary behavior,LPA,and MVPA)performed for each of the following durations: 10-19 min, 20-29 min, 30-39 min, 40-49 min,50-59 min,and ≥60 min.
2.4.Definition of sarcopenia
The EWGSOP2 categorizes probable sarcopenia as low muscle strength only, confirmed sarcopenia as low muscle strength and low muscle mass, and severe sarcopenia as low muscle strength, low muscle mass, and poor physical performance.1The authors recently acknowledged a reporting error with the published cut-point for ALM normalized to height.17Due to this confusion,absolute ALM was used as the measure of low muscle mass in this study.Hence,low muscle strength was defined as an HGS of<27 kg(men)or<16 kg(women),low muscle mass as an ALM of <20.0 kg (men) or <15.0 kg(women), and low physical performance criteria as a TUG time of ≥20 s.1Due to the fact that there were low numbers of probable and confirmed sarcopenia, and no participants with severe sarcopenia, in this cohort, participants were classified as having either no sarcopenia or probable or confirmed sarcopenia for the purposes of the present analysis.
2.5.Incident falls over 12 months
At 6 months and 12 months after the baseline clinical appointment, participants were contacted by a research nurse by telephone to determine incident falls since the appointment.18Participants were asked whether they experienced any falls that were low energy(i.e.,falls from standing height),where they had unexpectedly come to rest on the ground (rather than any lower level) by himself or herself.Individuals who reported ≥1 falls over 12 months were classified as fallers, and individuals who reported ≥2 falls were additionally classified as multiple fallers.19
2.6.Statistical analyses
All statistical analyses were performed using SPSS (Version 25.0;IBM Corp.,Armonk,NY,USA).Data were initially checked for normality, and nonparametric tests were used where appropriate.Descriptive data were presented as mean±SD or median(interquartile range)for continuous variables or frequencies for categorical variables.Differences in participant characteristics according to sarcopenia status (no sarcopeniavs.probable or confirmed sarcopenia) were determined using independent samplesttests or Mann-WhitneyUtests(continuous variables),and χ2tests(categorical variables).
Multivariable binary logistic regression models were used to determine odds for sarcopenia and its components,and 12-month incident falls, per 1-h increase in sedentary,LPA, and MVPA.An initial model was adjusted for sex,BMI, and smoking status, and a subsequent model was further adjusted for other activity variables (e.g., sedentary behavior was adjusted for LPA and MVPA).Additionally,given that sedentary behavior, LPA, and MVPA may have U-shaped associations with incident falls and multiple falls,these outcomes were compared across quartiles of sedentary behavior, LPA, and MVPA using χ2tests and multivariable binary logistic regression analyses.
Independent samplesttests were used to compare means for total number of bouts per week at each duration for sedentary behavior,LPA,and MVPA between participants without sarcopenia and those with probable or confirmed sarcopenia.Multivariable binary logistic regression analyses were then performed to determine likelihood of sarcopenia and falls for each additional bout per week of sedentary behavior,LPA,and MVPA lasting for durations of 10-19 min,20-29 min,30-39 min, 40-49 min, 50-59 min, and ≥60 min.These analyses were adjusted for sex, BMI, smoking status, and number of bouts of the same duration for other activity variables(i.e.,sedentary bouts lasting 10-19 min were adjusted for LPA bouts lasting 10-19 min and MVPA bouts lasting 10-19 min).
Finally, multivariable linear regression models explored the associations of total time and number of bouts of sedentary behavior,LPA,and MVPA with components of sarcopenia(continuous variables).These analyses were adjusted for sex,BMI,and smoking status,as well as for total accelerometer wear time(total time analyses)or number of bouts of the same duration for other activity levels (bout analyses).For all analyses, collinearity diagnostics, including variance inflation factors and tolerance values,were used to check for multicollinearity.Values ofp<0.05 were considered statistically significant.
3.Results
Of 3633 participants initially recruited for this study, 3334(50.5% women) had complete anthropometric, accelerometer,and physical function data.Table 1 presents characteristics for participants classified as nonsarcopenic (98.2%), compared with probable(0.8%)or confirmed sarcopenic(1.0%).No participant met the criteria for severe sarcopenia.There were no differences in the proportion of men and women for the sarcopenic and nonsarcopenic groups, but sarcopenic participants were significantly more likely to be smokers.Sarcopenic participants tended to have lower BMI, but higher total body fat percentage,although these differences did not achieve statistical significance.As expected, sarcopenic participants had significantly lower ALM and HGS, and higher TUG time, than nonsarcopenic participants.There were no differences between groups for the total time spent wearing accelerometers,sedentary behavior, or LPA.However, the mean time spent in MVPA was significantly lower in the sarcopenic group compared to the nonsarcopenic group.
Table 2 reports the odds ratios for sarcopenia and its components according to time(h)spent in sedentary behavior,LPA,or MVPA.After adjustment for sex, BMI, and smoking status(Model 1), each 1 h/week increase in sedentary behavior was associated with a 1% reduced likelihood of having low ALM,but this association was not significant after further adjustment for LPA and MVPA (Model 2).Conversely, both LPA andMVPA were associated with a reduced likelihood of having low ALM after full adjustment (2% and 12% reductions 1 h/week increase, respectively).Only MVPA was associated with HGS,with each 1 h/week increase in MVPA associated with a 20%reduced likelihood of having low HGS after full adjustment.In the fully adjusted models, all intensities were associated with TUG; each 1 h/week increase in sedentary behavior was associated with a 4% increased likelihood of a high TUG time, and each 1-h increase in LPA and MVPA was associated with a 12% and 66% reduced likelihood of high TUG time, respectively.However, only MVPA was associated with probable or confirmed sarcopenia status.Each 1 h/week increase in MVPA was associated with a 20% reduced likelihood for presence of sarcopenia in the fully adjusted model.
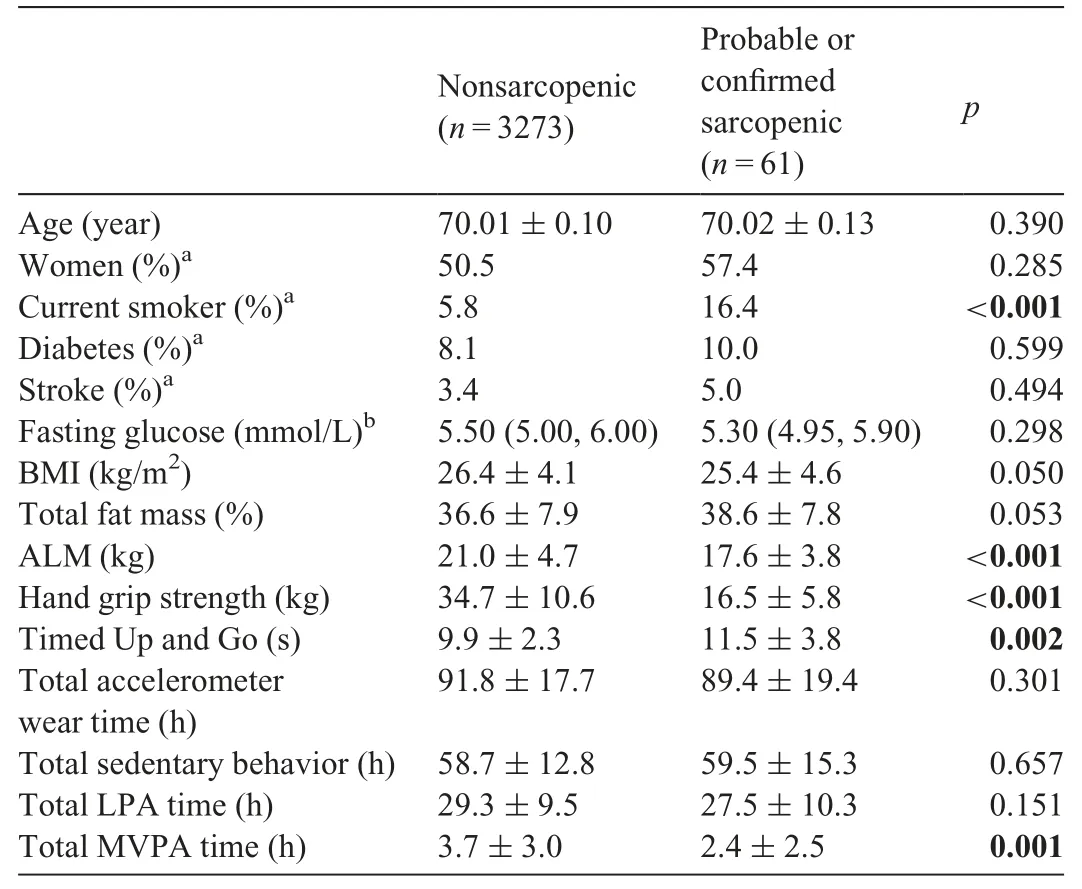
Table 1Participant characteristics according to sarcopenia status.
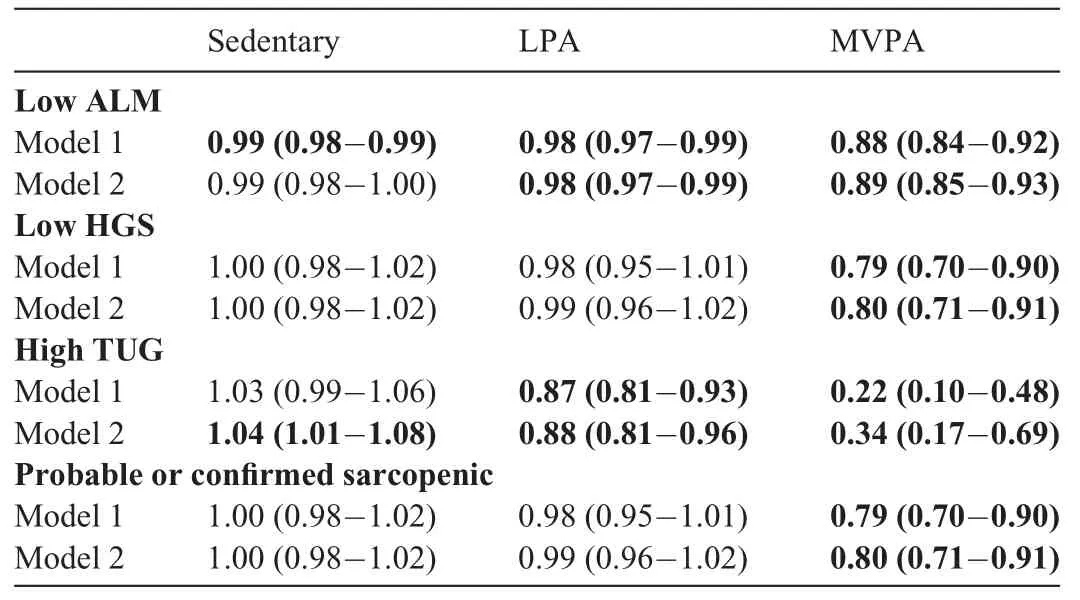
Table 2Odds ratios (95% confidence interval) for sarcopenia and its components per 1-h increase in sedentary behavior,LPA,and MVPA.
At 12 months after the clinic appointment, a total of 2748 participants(82.4%)provided valid falls data,with 14%of these participants reporting ≥1 fall and only 1% reporting multiple falls.After adjustment for sex,BMI,smoking,sarcopenia status,and time spent at other intensities, time spent in sedentary behavior, LPA, and MVPA were not associated with likelihood of any incident fall, or multiple falls, over 12 months (allp>0.05).Incident falls were further compared over quartiles of sedentary behavior, LPA, and MVPA.The χ2tests revealed that there were no differences in incidence of any falls across quartiles of sedentary behavior, LPA, or MVPA (allp> 0.05).There were also no differences in incidence of multiple falls across quartiles of sedentary behavior or LPA (p=0.213 andp=0.321, respectively).The incidence of multiple falls was highest in the lowest quartile of MVPA (Fig.1), although not after adjustment for confounders in multivariable binary logistic regression analyses(p=0.241).
For the entire cohort, the mean ± SD numbers for MVPA bouts of 10-19 min, 20-29 min, 30-39 min, 40-49 min,50-59 min,and ≥60 min were 8.5±8.8 per week,3.4±4.4 per week,1.7±2.7 per week,1.0±1.8 per week,0.5±1.2 per week, and 0.3 ± 0.8 per week, respectively.The numbers of light activity bouts of the same duration were 66.8 ± 33.9 per week,14.2±11.8 per week,4.6±5.2 per week,1.9±2.8 per week,0.9±1.7 per week,and 0.4±1.0 per week,respectively.Unsurprisingly,the numbers of sedentary bouts of these durations were substantially greater: 186.2 ± 45.1 per week,83.4±25.4 per week,43.2±16.1 per week,24.6±10.8 per week, 14.2 ± 7.5 per week, and 7.7 ± 4.9 per week, respectively.The numbers of bouts of all durations for MVPA were significantly higher in nonsarcopenic compared with sarcopenic participants(Fig.2):10-19 min(8.6±8.8 per weekvs.4.9±6.8 per week;p<0.001),20-29 min(3.5±4.4 per weekvs.1.9±3.2 per week;p<0.001),30-39 min(1.8±2.7 per weekvs.0.8±1.6 per week;p<0.001),40-49 min(1.0±1.8 per weekvs.0.4±0.9 per week;p<0.001),50-59 min(0.5±1.3 per weekvs.0.2±0.5 per week;p<0.001),and ≥60 min(0.3±0.8 per weekvs.0.1±0.3 per week;p<0.001).There were no differences in the numbers of bouts of any duration for LPA or sedentary behavior between nonsarcopenic and sarcopenic participants (allp>0.05).
As demonstrated in Table 3, after adjustment for covariates,including bouts of the same duration for sedentary behavior and LPA, higher numbers of MVPA bouts per week of 10-19 min,20-29 min,30-39 min,40-49 min,and 50-59 min retained an association with lower likelihood for probable or confirmed sarcopenia.Sedentary behavior and LPA bouts demonstrated no association with sarcopenia after multivariable adjustment,and bouts of all intensities were not associated with incident falls.
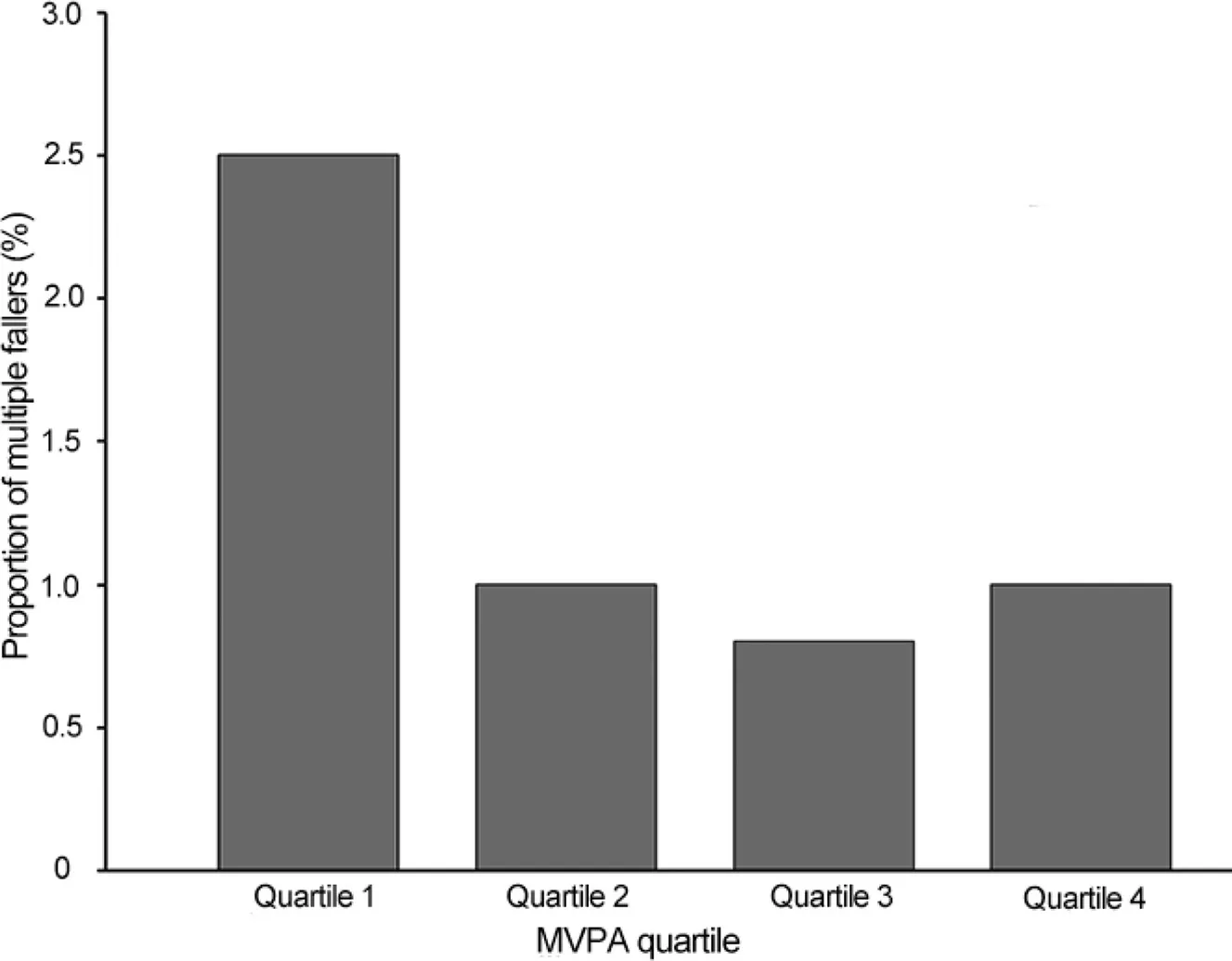
Fig.1.Proportions of multiple fallers within each quartile of MVPA.Value of p=0.032 before adjustment.Quartile 1:0-1.47 h/week;Quartile 2:1.48-3.12 h/week; Quartile 3: 3.13-5.27 h/week; and Quartile 4: 5.28-28.32 h/week.MVPA=moderate-to-vigorous physical activity.
Table 4 reports associations of sedentary behavior, LPA,and MVPA time and bouts with continuous variables for the components of sarcopenia.These multivariable linear regression analyses were adjusted for covariates, including total time of accelerometer wear or bouts of the same duration for other intensities.Sedentary behavior time and bouts were not associated with ALM or HGS,but were significantly positively associated with TUG time, with the exception of 10-19 min bouts.LPA time and bouts were positively associated with ALM but not HGS, and negatively associated with TUG time.MVPA time and bouts were positively associated with both ALM and HGS,but only for bouts up to and including 40-49 min for HGS.MVPA time and bouts were negatively associated with TUG time.With the exception of MVPA and HGS,where bouts of>50 min demonstrated nonsignificant associations and also lower coefficients than bouts of shorter duration, there did not seem to be threshold effects in the associations of increasing bout durations with sarcopenia components.
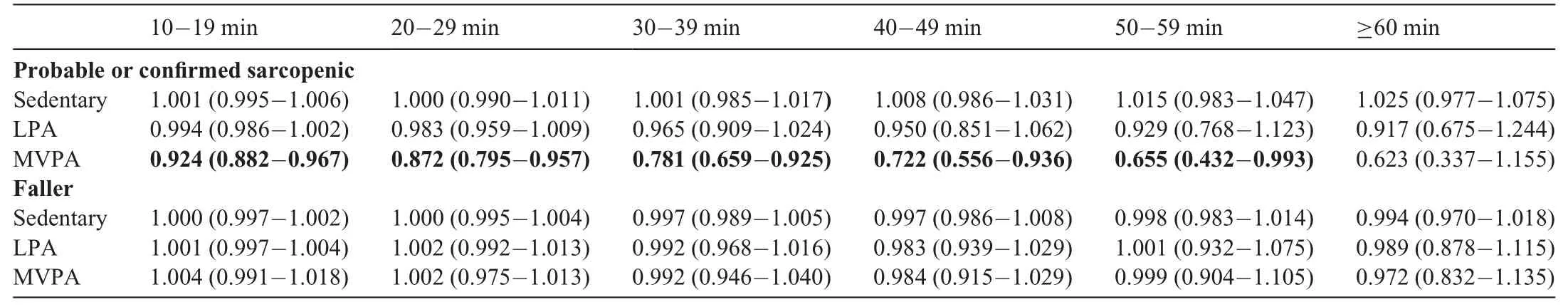
Table 3Odds ratios(95%confidence interval)for sarcopenia and falls according to number of bouts of sedentary behavior,LPA,and MVPA of differing duration.
4.Discussion
This population-based study of Swedish communitydwelling 70-year-olds demonstrated that higher total amounts and bouts of accelerometer-determined MVPA are consistently and independently associated with a reduced likelihood of probable or confirmed sarcopenia, but not 12-month incident falls.There was generally no evidence of a threshold effect for bouts of increasing duration in terms of their associations with sarcopenia and its components.
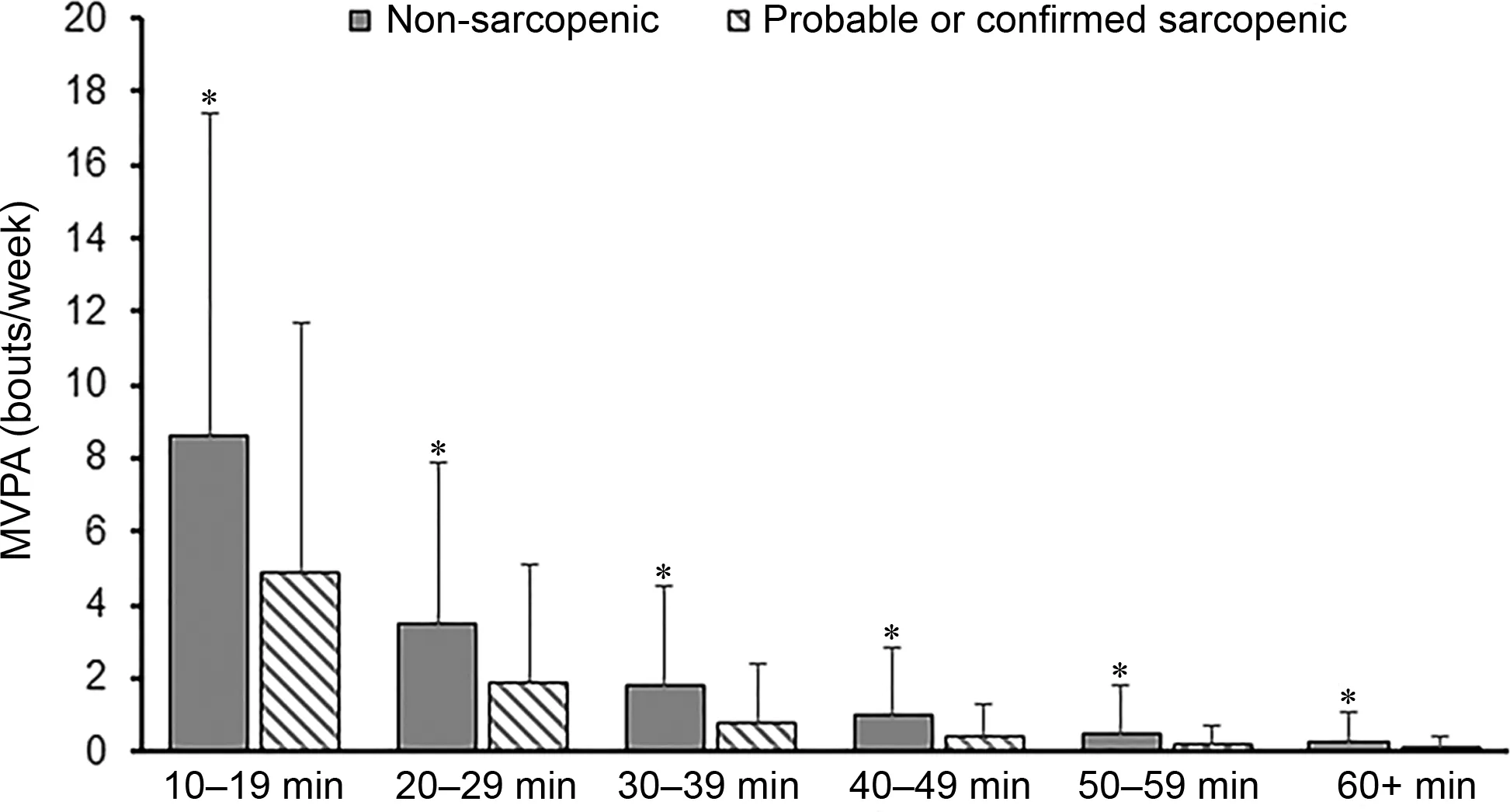
Fig.2.Total number of bouts of MVPA according to duration for nonsarcopenic and probable or confirmed sarcopenic participants.*p<0.001,significant difference of mean number of bouts for each duration between non-sarcopenic and probable or confirmed sarcopenic(independent samples t tests).MVPA=moderateto-vigorous physical activity.
To the best of our knowledge,this study is the first to report associations of accelerometer-determined PA and sedentary behavior with odds for sarcopenia according to the revised EWGSOP2 definition.1The primary differences between EWGSOP2 and the original EWGSOP1 definition include the recommended cut-off points for low muscle mass and strength,as well as the conceptual stages of sarcopenia (EWGSOP1:pre-sarcopenia, sarcopenia, and severe sarcopenia; EWGSOP2: probable sarcopenia, confirmed sarcopenia, and severe sarcopenia).1,20We combined probable and confirmed sarcopenic participants due to the very low numbers of 70-year-olds with EWGSOP2 sarcopenia in this cohort, which may reflect the generally more conservative cut-off points of EWGSOP2 compared with EWGSOP1, potentially resulting in low observed prevalence and limiting opportunities for early intervention in community-dwelling older adults.4Associations of accelerometer-determined PA with each conceptual stage of sarcopenia may be different than that observed for combined sarcopenia stages.Indeed, Aggio et al.21reported no association between accelerometer-determined MVPA and EWGSOP1 sarcopenia in older men, but reported a significant decrease in the risk of severe sarcopenia.Similarly, higher MVPA was not associated with a lower likelihood of having sarcopenia according to EWGSOP1 in the UK Hertfordshire cohort study,22but the Toledo Study of Healthy Aging demonstrated a 48%reduction in likelihood of sarcopenia per 1 h/day increase in objectively determined MVPA, according to U.S.Foundation for the National Institutes of Health criteria(which include more conservative cut-off points for muscle function than EWGSOP1).23Taken together with our own observation of a consistent association between MVPA total time and bouts with EWGSOP2 sarcopenia, it is possible that the benefits of MVPA for preventing sarcopenia are most apparent for sarcopenia definitions that use more conservative cut-off points.
Previous research has also demonstrated that accelerometer-determined MVPA is associated with individual components of sarcopenia.In Tasmanian older adults,accelerometerdetermined PA performed at light and moderate intensity was positively associated with ALM, whereas sedentary behavior had inconsistent associations with ALM.7This finding is in agreement with the findings of the present study, where total time and bouts of LPA and MVPA,but not sedentary behavior,were consistently positively associated with ALM.A study of 123 community-dwelling older Australians observed an association of longer sitting time with greater absolute lean mass(1.2 kg per 1 h of sitting time, 95% confidence interval:0.44-1.96;p< 0.01), but with significantly lower lean mass percentage,suggesting that perhaps sedentary behavior is associated more strongly with increases in total body mass rather than muscle mass specifically.24
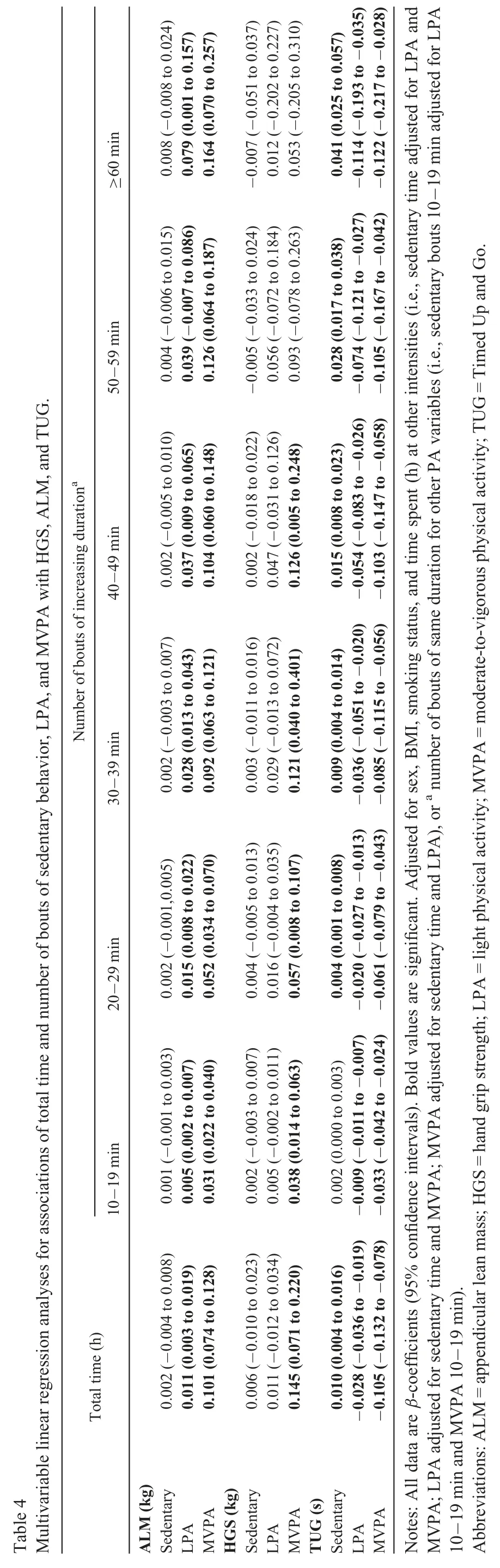
≥60 min 0.008(-0.008 to 0.024)0.079(0.001 to 0.157)0.164(0.070 to 0.257)-0.007(-0.051 to 0.037)0.012(-0.202 to 0.227)0.053(-0.205 to 0.310)0.041(0.025 to 0.057)50-59 min 0.004(-0.006 to 0.015)0.039(-0.007 to 0.086)0.126(0.064 to 0.187)-0.005(-0.033 to 0.024)0.056(-0.072 to 0.184)0.093(-0.078 to 0.263)0.028(0.017 to 0.038)Number of bouts of increasing durationa 40-49 min 0.037(0.009 to 0.065)0.104(0.060 to 0.148)0.002(-0.005 to 0.010)0.002(-0.018 to 0.022)0.047(-0.031 to 0.126)0.126(0.005 to 0.248)0.015(0.008 to 0.023)0.002(-0.003 to 0.007)0.092(0.063 to 0.121)30-39 min 0.003(-0.011 to 0.016)0.028(0.013 to 0.043)0.029(-0.013 to 0.072)0.121(0.040 to 0.401)0.009(0.004 to 0.014)20-29 min 0.015(0.008 to 0.022)0.052(0.034 to 0.070)0.002(-0.001,0.005)0.004(-0.005 to 0.013)0.016(-0.004 to 0.035)0.057(0.008 to 0.107)0.004(0.001 to 0.008)0.001(-0.001 to 0.003)10-19 min 0.005(0.002 to 0.007)0.031(0.022 to 0.040)0.002(-0.003 to 0.007)0.005(-0.002 to 0.011)0.038(0.014 to 0.063)0.002(0.000 to 0.003)Total time(h)0.002(-0.004 to 0.008)0.011(0.003 to 0.019)0.006(-0.010 to 0.023)0.011(-0.012 to 0.034)0.145(0.071 to 0.220)0.010(0.004 to 0.016)-0.028(-0.036 to-0.019) -0.009(-0.011 to-0.007) -0.020(-0.027 to-0.013) -0.036(-0.051 to-0.020) -0.054(-0.083 to-0.026) -0.074(-0.121 to-0.027) -0.114(-0.193 to-0.035)-0.105(-0.132 to-0.078) -0.033(-0.042 to-0.024) -0.061(-0.079 to-0.043) -0.085(-0.115 to-0.056) -0.103(-0.147 to-0.058) -0.105(-0.167 to-0.042) -0.122(-0.217 to-0.028)Table 4 Multivariable linear regression analyses for associations of total time and number of bouts of sedentary behavior,LPA,and MVPA with HGS,ALM,and TUG.ALM(kg)Sedentary LPA MVPA0.101(0.074 to 0.128)HGS(kg)Sedentary LPA MVPA TUG(s)Sedentary LPA MVPA Notes:All data are β-coefficients (95% confidence intervals). Bold values are significant.Adjusted for sex, BMI,smoking status, and time spent(h) at other intensities (i.e., sedentary time adjusted for LPA and MVPA;LPA adjusted for sedentary time and MVPA;MVPA adjusted for sedentary time and LPA),or a number of bouts of same duration for other PA variables(i.e.,sedentary bouts 10-19 min adjusted for LPA 10-19 min and MVPA 10-19 min).Abbreviations:ALM=appendicular lean mass;HGS=hand grip strength;LPA=light physical activity;MVPA=moderate-to-vigorous physical activity;TUG=Timed Up and Go.
Foong et al.7also observed that light,moderate,and vigorous PA,but not sedentary behavior,were all positively associated with lower limb strength.In the present study, only MVPA was positively associated with HGS, and this may reflect differences in common activities undertaken at different intensities;for example,MVPA may be more likely than LPA to include exercise involving upper limb contractions,whereas LPA may most commonly involve walking.In support of this possibility, we observed that LPA (as well as MVPA) was independently associated with better TUG time.TUG was the only sarcopenia component for which sedentary behavior demonstrated a significant association; greater amounts of sedentary behavior were associated with poorer TUG time independent of LPA and MVPA.The Toledo Study of Healthy Aging reported that only MVPA was associated with gait speed,23but a separate study found that greater sedentary behavior is associated with slower TUG time in a cohort of British 60-year-olds to 64-year-olds.25
The U.S.Physical Activity Guidelines Advisory Committee recently published an umbrella review concluding that regular PA delays loss of physical function and mobility and reduces risk of fall-related injuries.26Our results support the concept that greater amounts of MVPA, for which the coefficients were of substantially greater magnitude compared with LPA and sedentary behavior, are associated with better physical function(handgrip strength, TUG, and probable or confirmed sarcopenia).It is unclear, however, why no associations were observed with 12-month incident falls in multivariable models.This finding may be related to the fact that injurious falls were not assessed and/or the low overall incidence of falls observed.Also, greater amounts of sedentary behavior, although likely to deleteriously effect physical function and mobility,likely protect against falls by reducing ambulation and therefore exposures that may cause falls.The incidence of multiple falls was lowest in the quartile with the greatest sedentary behavior (although this difference was nonsignificant) and was significantly higher in the lowest quartile of MVPA in unadjusted, but not adjusted,analyses.Similarly, in a study of women aged 63-99 years,those in the lowest accelerometer-determined MVPA quartile had 18%increased falls rates compared with those in the highest quartile,8although sensitivity analyses demonstrated that the association was only present in women with poorer physical function or with a history of ≥2 falls.Importantly, the findings of the previous study and our own demonstrate that greater amounts of MVPA do not increase risk for falls.Given the clear benefits of MVPA for functional and other health outcomes,clinicians should have confidence in recommending that older patients participate in activities at higher intensities.
This study is the first we are aware of to examine whether thresholds exist for associations of PA bouts of increasing duration with sarcopenia and its components, as well as incident falls.Current guidelines recommend accumulation of PA in bouts of ≥10 min based on data for cardiometabolic risk factors,but accumulation of more PA bouts lasting ≥10 min is not beneficial beyond total volume of activity for reducing all-cause mortality in older men.27We observed similar associations for sarcopenia and its components in the present study; significant associations between levels of activity and sarcopenia components were consistently observed for both total time of activity as well as number of bouts, suggesting that the pattern in which activity is accumulated does not influence these associations.Furthermore,there did not seem to be a threshold at which the strength of association between bouts of increasing duration with sarcopenia outcomes was diminished.The only exception was the association between MVPA and HGS, where the magnitude of the coefficient decreased and became nonsignificant for bouts of>49 min.It is possible that this finding is explained by the low numbers of MVPA bouts recorded at longer durations, and so it is likely that increasing benefits are obtained for lean mass and physical function with increasing duration bouts of activity of ≤1 h.
The primary limitation of the present study is that the associations among PA, sedentary behavior, and sarcopenia and its components are cross-sectional.Although higher PA is likely to contribute to improved muscle function,it is equally likely that better muscle function enables participation in greater volumes and intensities of PA.28Falls were assessed prospectively at 6 months and 12 months,but only low-energy falls that resulted in coming to rest at ground level were recorded, rather than falls resulting in coming to rest at any lower level (i.e., partial falls not resulting in falling to the ground), as commonly defined in other studies.29The accelerometer cut-points for activity intensities used have been validated previously,15but derived associations with sarcopenia and falls may not be comparable with studies using different accelerometer devices and cut-points.30Finally,as discussed previously,there was a low number of participants with sarcopenia as defined by EWGSOP2 in this community-dwelling cohort, and it is likely that our results cannot be generalized to other older adult populations.
5.Conclusion
The findings of this cohort study of Swedish older adults suggest that clinicians should encourage older adults to participate in longer durations of weekly MVPA to reduce the risk for developing sarcopenia,and that this type of activity can be performed without exposing older adults to increased falls risks.Further prospective studies are required to determine causality in the relationship between MVPA and sarcopenia, and whether benefits of MVPA persist over the long term.
Acknowledgments
This work was supported by the Swedish Research Council(Grant number 2011-2976).DS is supported by an Australian National Health and Medical Research Council (NHMRC)R.D.Wright Biomedical Career Development Fellowship(Grant number GNT1123014).The funding sources had no involvement in the study design, collection analysis or interpretation of data,writing of the manuscript, or the decision to submit for publication.
The authors thank Healthy Ageing Initiative research personnel Magnus Lindblom, David Lapvetel¨ainen, and Jim Viklund,who were responsible for data collection.
Authors’contributions
DS conceived the manuscript idea, performed statistical analyses,and drafted the manuscript;JJ completed accelerometer data analysis and revised the manuscript; AG performed statistical analyses and revised the manuscript; PRE revised the manuscript;PN and AN conceived and designed the study,and revised the manuscript.All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
杂志排行
Journal of Sport and Health Science的其它文章
- A systematic review of running-related musculoskeletal injuries in runners
- Most ankle sprain research is either false or clinically unimportant:A 30-year audit of randomized controlled trials
- Effects of plyometric vs.resistance training on skeletal muscle hypertrophy:A review
- Pacing profiles and tactical behaviors of elite runners
- Exercise attenuates bone mineral density loss during diet-induced weight loss in adults with overweight and obesity:A systematic review and meta-analysis
- Adverse associations of sedentary behavior with cancer incidence and all-cause mortality:A prospective cohort study
