The impacts of resilience on the association between illness uncertainty and sleep quality among patients with type 2 diabetes mellitus
2021-06-25XinGeWANGYuQiongWENHuiBingKUANGLiXiaLINHongCUIDivisionofEndocrinologyGuangdongProvincialPeopleHospitalGuangdongAcademyofMedicalSciencesGuangzhouChinaDivisionofNephrologyGuangdongProvincialPeopleHospitalGuangdongAcademyo
Xin-Ge WANG, Yu-Qiong WEN,Hui-Bing KUANG, Li-Xia LIN, Hong CUIDivision of Endocrinology, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences,Guangzhou, China; Division of Nephrology, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, China; Cardiology Care Unit, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, China; Nursing Administraion, Guangdong Provincial People’s Hospital,Guangdong Academy of Medical Sciences, Guangzhou, China
ABSTRACT
Objective: The objective was to investigate the relationship between resilience, illness uncertainty, and sleep quality in patients with type 2 diabetes mellitus (T2DM).
Methods:This cross-sectional study was conducted from September 2019 to August 2020 from a tertiary hospital in Guangzhou, China. Totally,205 participants completed questionnaires concerning demographic characteristics, Pittsburgh sleep quality index, Mishel uncertainty in illness scale (MUIS), and Connor–Davidson Resilience Scale (CD-RISR) were collected by convenience sampling. Multiple hierarchical regression analysis was used to evaluate the interaction of illness uncertainty, resilience, and sleep quality. The mediating role of resilience was also tested.
Results: The total score of illness uncertainty was 94.68 ± 11.19 in T2DM patients, which was proved in the medium level. There was a significant negative correlation between the total CD-RISR score and total MUIS score (r = −0.716, P < 0.01); there was a significant negative correlation between the total CD-RISR score and total PISQ score (r = −0.806, P < 0.01); total MUIS score was positively correlated with PISQ score (r = 0.872, P < 0.01). Psychological resilience could partially mediate the association between sleep quality and the level of illness uncertainty, and the mediating effect was 0.293, accounting for 34.20% of the total effect.
Conclusion: Patients with T2DM have a moderate level of illness uncertainty, and it was negatively correlated with mental resilience level and positively associated with sleep quality. Medical staff should strengthen psychological intervention for T2DM patients to reduce the sense of uncertainty.
Keywords: Disease uncertainty, mental resilience, psychological intervention, sleep quality, type 2 diabetes mellitus
INTRODUCTION
Recently, the significance of positive psychological resources has aroused increasing attention in the chronic disease field.Resilience is the ability to gradually and successfully recover from stressful events, such as frustrations and failures that threaten the stability, the function, or the development of the mental system.[1]Evidence indicated that individuals with high resilience appear to be in a high capability for flexible adaptation to impinge challenges.[2]Based on previous studies,high resilience could alleviate abnormal sleep quality state among clinical patients.[3]Moreover, it is documented that resilience served as a “moderator” to alleviate the side effect of abnormal psychological condition.[4]Given on previous study, resilience could moderate the effect of perceived stress on sleep quality among residents.[5]Furthermore, a previous study has shown that resilience could play a mediate role on the association of stressor with sleep quality.[6]
Sleep problems are increasing dramatically in patients with type 2 diabetes mellitus (T2DM).[7]The limitations of T2DM treatment including repeated insulin injections, high costs,strict diet plan, and possibility of recurrent infections and repeated hospitalizations cause the negative emotions[8]such as depression, anxiety and restless, and abnormal peripheral nervous function,[9]which may impair sleep quality in patients with T2DM. Larcheretal.[10]have suggested that T2DM patients reported the higher prevalence rate of sleep difficulties than in nondiabetic subjects. Previous studies[11,12]with written self-report have shown that the poor and insufficient sleep state in T2DM patients may aggravate abnormal metabolic health function, endocrine system, as well as immune system. Furthermore, poor sleep quality contributes to cardiovascular complications in T2DM patients.[13]Therefore, identifying the possible factors contributing to or preventing sleep problems in patients with T2DM is of vital significance.
Uncertainty as a psychological assessment factor refers to the inability to identify abnormal events related diseases.[14]In accordance with illness uncertainty theory, illness uncertainty mainly defines a condition when individual is incapable of classifying the implication of events associated with illnesses, including the difficulties of interpreting disease relevant symptoms and predicting the outcomes of treatment.[15]Recent evidence found that illness uncertainty negatively impacted sleep quality.[16]Furthermore, other studies have shown that awareness of illness uncertainty could affect patients to be in uncertain situations, which results in T2DM patients to be addicted in a panic state and significantly impact their quality of life, as well as contribute to psychological distress.[16,17]
In recognition of the current situation, this study aimed to investigate the impacts of illness uncertainty and resilience on sleep quality and to explore whether resilience mediated the relationship of illness uncertainty with sleep quality among patients with T2DM.
METHODS
Participants
This study was conducted from September 2019 to August 2020, and patients with T2DM were selected from Guangdong Provincial People’s Hospital by convenience sample. Inclusion criteria were (1) in line with the diagnostic criteria for T2DM established by the WHO in 1999; (2) age ≥18 years; and (3)participants who volunteered to participate and signed informed consent. Exclusion criteria were (1) patients diagnosed with mental illness or emotional disorders; (2) patients suffering other serious medical conditions (such as cancer); and (3)complications of acute diabetes mellitus.
Measurement tools and procedure
The questionnaire was designed including four sections:demographic characteristics, measurement of illness uncertainty,Pittsburgh sleep quality index (PSQI), and the Chinese version of Connor–Davidson Resilience Scale. All patients who participate in this study were required to fill it out.
Demographic characteristics
Demographic variables included age, marital status, education level, monthly income, employment status, suffering T2DM duration, and having children in the present study. Marital status was classified as divorced/widowed, married, and single. Education background was categorized as junior high school and lower, senior high school, and junior college,and bachelor. Monthly income was split as <6000 China Yuan (CNY) and ≥12,000 CNY.
Measurement of illness uncertainty
We used the Chinese version of the Mishel Uncertainty in Illness Scale (MUIS) to measure illness uncertainty,which contains 33 items in 4 dimensions, including the sense of ambiguity, complexity, lack of information, and unpredictability.[18]Each item is rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The total score of MUIS-A ranges from 32 to 160, and the higher the score, the higher the patient’s level of disease uncertainty was. Among them, 32.0–74.0 indicates low level, 74.8–117.4 indicates medium level, and 117.5–160.0 indicates high level.The internal consistency Cronbach’s alpha coefficient was 0.889 in the present study.
Pittsburgh sleep quality index
We used the PSQI to assess sleep quality in T2DM patients in previous months, which includes 19 items, divided into seven dimensions, namely subjective sleep quality, sleep latency,sleep duration, habitual sleep efficiency, sleep disturbance,use of sleeping medication, and daytime dysfunction.[19]Each dimension has score range from 0 (no dysfunction) to 3 (severe dysfunction). The total score has a possible range of 0–21 points, and >5 points indicating poor sleep quality.The Cronbach’s alpha coefficient was 0.843 in the study.
Chinese version of Connor–Davidson Resilience Scale
We used the Chinese version of Connor–Davidson Resilience Scale (CD-RISC) to evaluate the level of resilience in patients with T2DM, compiled by Connoretal.,[20]which comprises 25 items in three dimensions (tenacity, self-improvement,and optimism) that assess resilience or capacity to change and cope with adversity. Each item is scored on a five-point scale ranging from 0 (not true at all) to 4 (true nearly all the time). The total score ranges from 0 to 100, and higher score indicates stronger levels of resilience. The Cronbach’s alpha coefficients of resilience and its three dimensions were 0.921,0.869, 0.833, and 0.597, respectively.
Procedure
The researcher explained the purpose of the survey to the subjects. For dyslexic patients, the researcher would read for them one by one and assisted them to finish the questionnaire. All surveys were completed and collected on the spot. Finally, a total of 210 participants took part in the study, 4 provided incomplete data, and 1 was diagnosed with depression. Thus, 205 (97.61%) participants completed valid questionnaires.
Ethical considerations
This cross-sectional study was supported by the Ethics Committee on Human Experiment of Guangdong Provincial People’s Hospital and in accordance with the ethical standards. The questionnaire is anonymous and just used to do this study. Informed consent was obtained from all participants before the study.
Statistical analysis
SPSS 22.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis, measurement data were expressed by mean ± standard deviation, comparison between groups was analyzed usingt-test, analysis of variance, Pearson correlation analysis, and stepwise regression analysis, andP< 0.05 was considered statistically significant.
RESULTS
Demographic data
The demographic characteristics of 205 patients with T2DM are presented in Table 1.
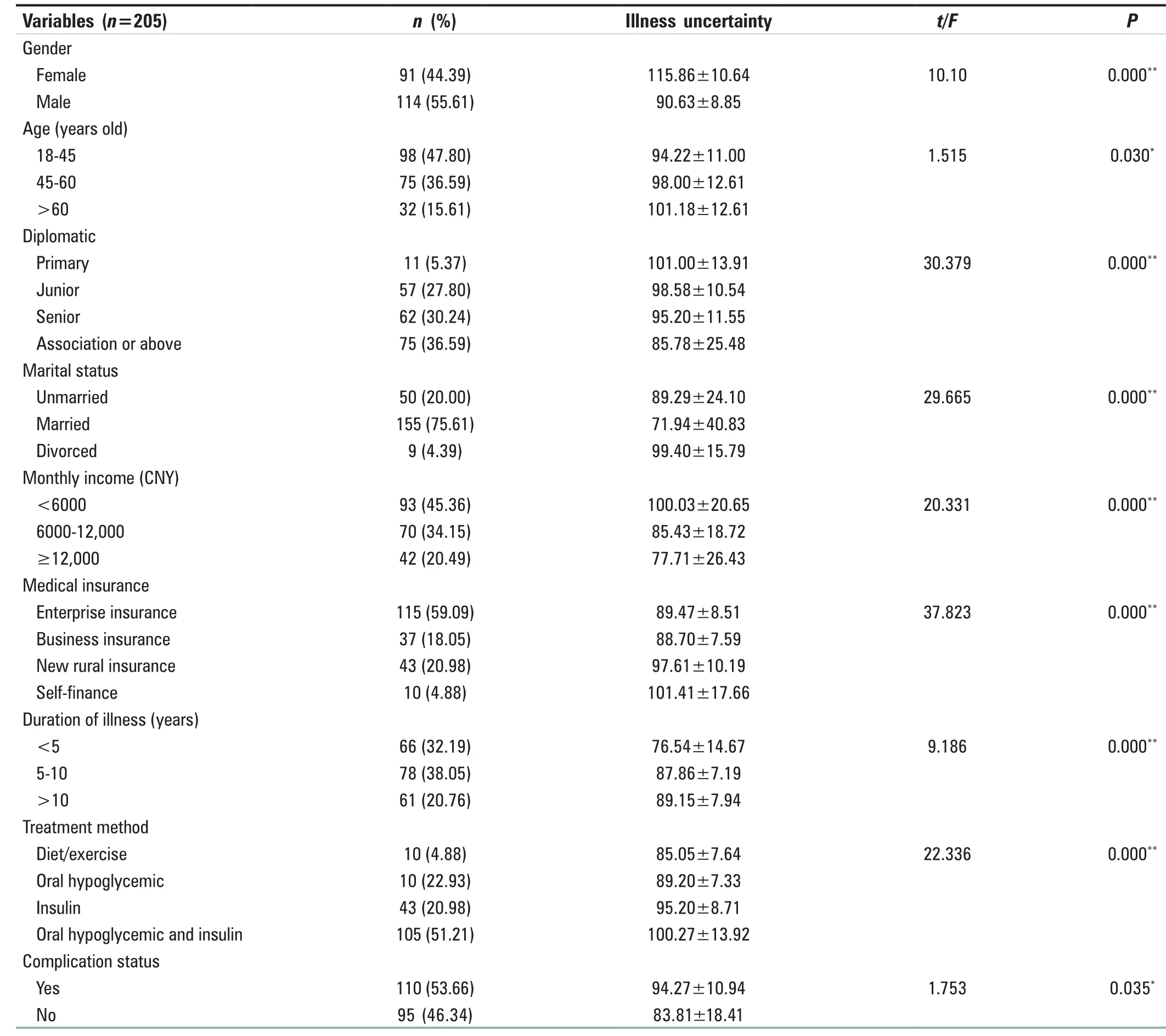
Table 1: Characteristics of 205 patients with type 2 diabetes mellitus
The total mean score of MUIS of T2DM patients was 94.68 ± 11.19, which was in the medium level. Among them, the mean of the sense of ambiguity dimension was 34.03 ± 7.38, disease information lacking dimension was 19.44 ± 3.77, complexity dimension was 19.57 ± 3.16,and unpredictability dimension was 15.51 ± 6.64. It is documented that the respondents with the highest degree of illness uncertainty were generally males who aged over 60,in lower education level, and divorced, besides, patients with monthly income <6000 CNY were also vulnerable. In addition, the glycosylated hemoglobin level ranges from 5.5% to 15%, with a mean level of (8.93 ± 1.30)%. The total mean score of CD-RISC was 56.29 ± 5.17, which was in a middle level, and the total mean score of PISQ was 12.06 ± 3.72.
Correlations of continuous variables of type 2 diabetes mellitus patients
In Table 2, the coefficients (r) between these continuous variables (illness uncertainty, resilience, and sleep quality)are displayed. The results showed that the total MUIS score was negatively correlated with the total Connor–Davidson Resilience Scale (CD-RISR) score (r= −0.716,P= 0.000);however, the total MUIS score was positively correlated with the total PISQ score (r= 0.872,P= 0.000). Moreover, the total CD-RISC score was negatively correlated with the total PISQ score (r= −0.806,P< 0.01).
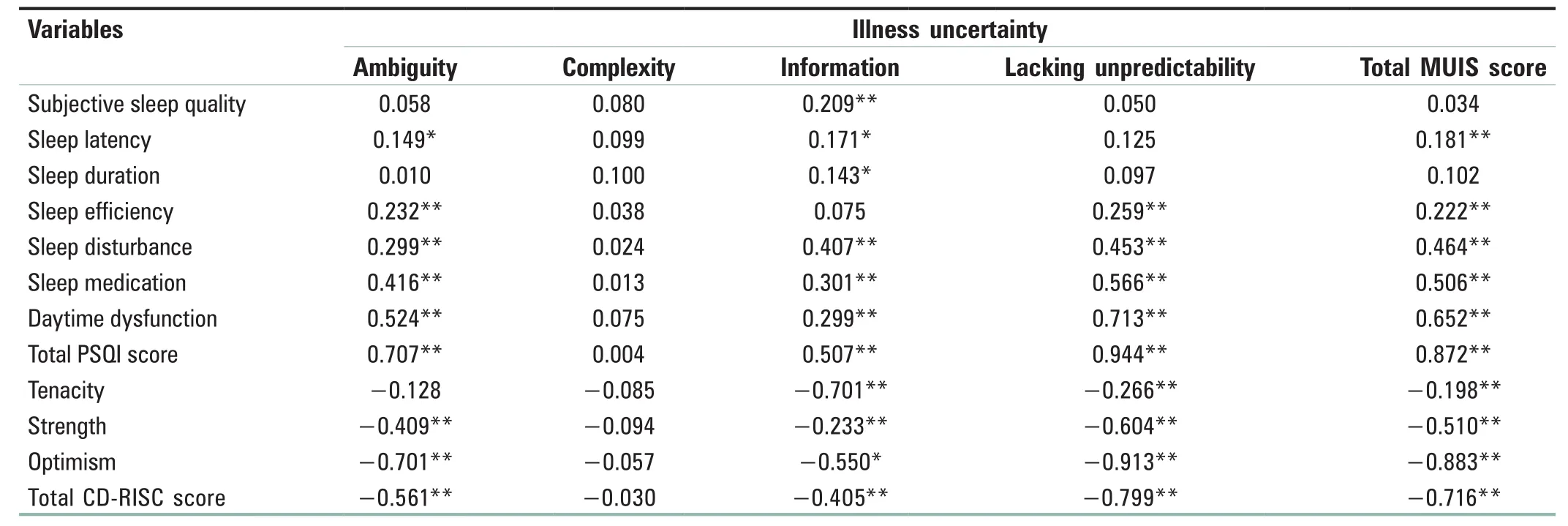
Table 2: Pearson’s correlations (r) between Mishel uncertainty in illness scale, Pittsburgh sleep quality index, and Chinese version of Connor-Davidson resilience scale scores among type 2 diabetes mellitus (n=205)
Linear regression results among Mishel uncertainty in illness scale, Connor–Davidson Resilience Scale, and Pittsburgh sleep quality index of type 2 diabetes mellitus patients
In this study, the three metrics of illness uncertainty composed the dependent variables, while resilience (including its three metrics) and sleep quality (including its seven metrics) comprised the independent variables. Stepwise regression analysis was conducted and the values for “the alpha to enter” and “the alpha to remove” were 0.05 and 0.10, respectively. Table 3 shows the linear regression results for the relationship among illness uncertainty,resilience, and sleep quality characteristics, illustrating that low level of strength, poor sleep quality and sleep efficiency were of a predictor of a high level of ambiguity (F=18.666,P< 0.001,R2=0.218,adjustedR2= 0.206); a low-level optimism, severe sleep disturbance mainly predicted a high level of complexity (F= 49.882,P< 0.001,R2= 0.331,adjustedR2= 0.324); low levels of strength and tenacity,and highly frequent sleep disturbance mainly predicted a high level of high unpredictability level (F= 31.179,P< 0.001,R2= 0.318, adjustedR2= 0.307); low levels of strength and tenacity, and the state of sleep latency and daytime dysfunction were the main predictor of a high level of total illness uncertainty level (F= 70.488,P< 0.001,R2= 0.585, adjustedR2= 0.577).
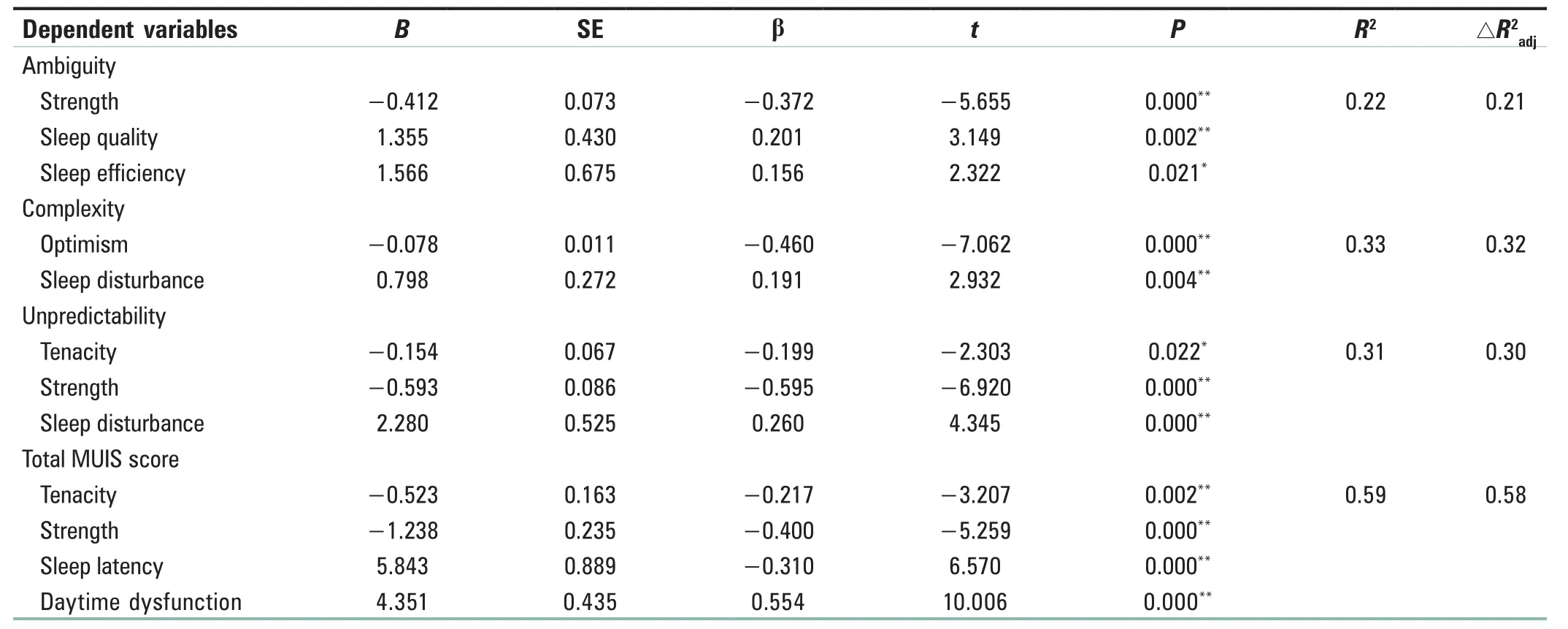
Table 3: Multiple linear regression coefficients among Mishel uncertainty in illness scale, Pittsburgh sleep quality index, and Chinese version of Connor-Davidson resilience scale scores and sociodemographic variables (n=205)
The moderation of resilience
The linear regression analysis was used to explore the mediating role of psychological resilience. Direct effects were found between illness uncertainty and sleep quality (β = 0.869,P< 0.01). Furthermore, the direct effect of sleep quality on resilience was evaluated, demonstrating that sleep quality was negatively associated with resilience (β = −0.806,P< 0.01), while resilience negatively predicted illness uncertainty state (β = −0.691,P< 0.01). In the last step,after controlling the impact of psychological resilience on illness uncertainty, sleep quality could negatively predict illness uncertainty (β = −0.563,P< 0.01). Meanwhile,standardized regression coefficients were reduced from β = 0.869 to β = 0.563 after the inclusion of psychological resilience, which proved that resilience partially mediated the influence of sleep quality on the illness uncertainty variable. Furthermore, the total effect of sleep quality on illness uncertainty was 0.856, and the mediating effect of psychological resilience on the association illness uncertainty and sleep quality was 0.293, accounting for 34.20% covariance of the total effect.
DISCUSSION
This study investigated the associations of illness uncertainty with sleep quality, and this is the first exploration on the mediating roles of resilience in the association of illness uncertainty with sleep quality among patients with T2DM.Finally, 205 subjects were recruited, with a high response rate (97.61%), indicating a reasonable demonstration of this research.
In this study, it is mainly revealed that T2DM patients suffered from medium illness uncertainty (94.68 ± 11.19), which was similar with the previous survey,[21]revealing that the condition of illness uncertainty should be improved. Previous studies have shown that the state of illness uncertainty was higher in patients with T2DM, including a serial of negative emotions such as anxiety,[22]depression,[23]helpless,[8]low medication compliance rate[24]and undermines self-esteem.[25]Moreover,long-term continuous treatment for T2DM would form a vicious cycle to lead to psychological problems including increasing illness uncertainty among T2DM.[26]It has been shown that illness uncertainty of T2DM was higher than other chronic diseases,[27]and the critical reason is that the clinical manifestations of T2DM showed major heterogeneity,which make the patients incapable of predicting the disease’s development or the severity of complications related with T2DM;[28]this adversely contributes to illness uncertainty.Furthermore, individual with high illness uncertainty is the inability of seeking for useful information about treatment,which brings about confusion[29]and worries for T2DM patients,[30]which in turn decreases sleep quality.
The study illustrated that the total mean PSQI score in T2DM patients was 12.06 ± 3.72, which was higher compared with Thailand (7.86 ± 5.42),[31]Canada (6.98 ± 4.03),[32]and Germany (7.2 ± 3.6),[33]respectively, indicating a poor sleep quality of T2DM patients. Studies have demonstrated that blood glucose control is influenced by sleep quality in patients with T2DM,[34]and the state of sleep quality could be an important indicator of abnormal blood glucose, which could vividly illustrate the reasonable cause of abnormal glycosylated hemoglobin level, and furthermore, emphasize the significance of improving the poor sleep quality among T2DM group. Another study has shown that the poorer sleep quality of type 2 diabetes is, the worse self-management ability is.[35]In addition, sleep quality was found to negatively associated with illness uncertainty, which was in accordance with previous study,[36]in other words, patients with poor sleep quality may suffer from higher illness uncertainty. The correlation analysis of this study showed that the total MUIS score was positively correlated with the total PISQ score, that is showing that the higher illness uncertainty patients had,the poorer sleep quality was, which was consistent with the previous researches.
Furthermore, the total mean score of CD-RISC was 56.29 ± 5.17, which was also in a medium level, which was similarly reported in studies undertaken in other countries.As a developable and positive resource, resilience could reduce abnormal mental health, such as illness uncertainty,[16]depression and stress,[37]enhance health-related life quality,[38]and increase sleep quality.[5,39]In this study, the total CD-RISC score was negatively correlated with the total PISQ score in patients with T2DM, indicating the higher the level of resilience, the better the sleep quality was, which further proved that patients can enhance sleep quality by improving resilience. In addition, the total MUIS score was negatively correlated with the total CD-RISR score in patients with T2DM,which revealed the higher the level of resilience, the lower the illness uncertainty is, that is, patients could reduce illness uncertainty by improving the level of resilience. The findings of Friborgetal.[40]also demonstrated that compared to patients in poor psychological resilience, individual in high-level psychological resilience perceived less psychological pain or distress, with a higher mental health level.
Regarding to the effects of resilience, it has been revealed that resilience partially mediated the association between illness uncertainty and sleep quality; the result was also documented in previous research.[16]That means that T2DM with lower illness uncertainty showed higher resilience and therefore,better sleep quality. It has been reported that individual with high level of resilience is able to have high coping self-efficacy to positively adapt and maintain good sleep quality in the face of stressors.[41,42]Thereby, T2DM with high resilience could maintain good sleep quality and avoid sleep problems. Briefly,targeted psychological interventions based on resilience should be undertaken to increase resilience so as to improve sleep quality among patients with T2DM.
In sum up, some strengths should be emphasized in this study. Theoretically, our study confirmed the association between resilience, illness uncertainty, and sleep quality,besides, the mediation role of resilience on illness uncertainty and sleep quality among T2DM patients were also detected,which provided the robust basis for future interventions.In practice, low illness uncertainty and poor sleep quality are relatively prevalent in T2DM. Medical staff should offer targeted information support to increase illness perception and reduce illness uncertainty and. Moreover, targeted relevant interventions based on resilience also should be implemented, such as mindfulness-based skill or cognitive behaviors, thus improving sleep quality.
However, several limitations also should be mentioned.First, sleep quality, illness uncertainty, and resilience were measured by self-report questionnaires, which may affect the associations of them due to possible response bias. Second,our study was only carried out in the area of Guangdong Province, the southeastern region of China. Hence, further study should be taken when attempting to extrapolate the results to T2DM in other regions of China.
CONCLUSION
In summary, patients with T2DM suffered from high illness uncertainty and poor sleep quality. Moreover, resilience could mediate the association of illness uncertainty and sleep quality.Hence, in practice, targeted information support should be offered to increase illness perception. Moreover, more targeted psychological interventions should be provided to enhance resilience in order to improve sleep quality.
Acknowledgments
All members of the research team would like to thank all the participants in the study who assisted in obtaining written informed consent for the survey.
Financial support and sponsorship
Nil.
Con flicts of interest
There are no conflicts of interest.
杂志排行
Journal of Integrative Nursing的其它文章
- Effect of health locus of control on the quality of life among hemodialysis patients
- Scienti fic publications in nursing journals from East Asia:A survey of literature
- Mediating effect of undergraduate nursing students’professional commitment on positive psychological capital and learning burnout
- Correlation between psychological factors and the expression of galanin and 5-hydroxytryptamine in different subtypes of gastroesophageal re flux disease
- A nursing study on five-animal frolics in improving anxiety and depression of inpatients
- Teaching traditional Chinese medicine classics to clinical nurses: Taking Treatise on Cold Damage for example
