Preservation of superior rectal artery in laparoscopically assisted subtotal colectomy with ileorectal anastomosis for slow transit constipation
2021-06-24ChienWeiWuTaWeiPuJungChengKangChengWenHsiaoChaoYangChenJeMingHuKuanHsunLinTzuChiaoLin
Chien-Wei Wu, Ta-Wei Pu, Jung-Cheng Kang, Cheng-Wen Hsiao, Chao-Yang Chen, Je-Ming Hu, Kuan-Hsun Lin, Tzu-Chiao Lin
Abstract
Key Words: Slow transit constipation; Superior rectal artery; Anastomosis leakage;Laparoscopic-assisted colorectal surgery; Iliorectal anastomosis; Colonic transit time
INTRODUCTION
Constipation means the incapacity to evacuate the bowel. Patients cannot evacuate completely and spontaneously at least three or more timesperweek although it is commonly one or fewer bowel movementsperweek. Most patients with constipation have one or more of the following symptoms: Hard infrequent stools, excessive straining, incomplete evacuation, excessive time attempting to evacuate or dissatisfaction with defecation[1 -4 ].
Slow transit constipation (STC) has been traditionally considered and classified as a functional disorder. However, clinical and manometric evidence has been accumulating that suggests most of the motility abnormalities in STC might be neuropathic[5 ].
Radiopaque markers with a transit colon test showed delayed of the transpiration of the colon is used for making the diagnosis[2 ,3 ,6 ]. If the conservative treatment is failed and pelvic outlet obstruction was ruled out, surgical procedure with a subtotal colectomy may be effective[7 ]. The most unwanted complication of the procedure is an anastomotic leak (AL). AL is a serious complication of colorectal surgery and can be defined as: ‘the luminal contents leaking from a surgical connection between 2 hollow viscera’[8 ]. AL is responsible for up to 40 % of the postoperative mortality rate,prolonged hospitalization, and an increase in the costs of healthcare due to the treatment of sepsis and the need for re-operation[9 ]. The main aim of this study is to make known a feasibility and functional outcome of laparoscopically assisted subtotal colectomy with the preservation of the superior rectal artery (SRA) in ileorectal anastomosis for STC.
MATERIALS AND METHODS
This investigation is an observational single-center study. The decision on whether to preserve the SRA was left to the discretion of the surgeon. Of the patients who were treated at the Division of Colon and Rectal Surgery at the Taiwan Adventist Hospital between January 2016 and January 2017 , patients diagnosed with constipation(compatible with the Rome II criteria)[10 ] were tested with laboratory studies including a thyroid-function test, serum calcium, serum glucose, and complete blood count. All cases had clinical evaluation, such as a digital rectal examination and a psychological consultation. We excluded secondary causes (colonic obstruction,metabolic disorders, and drug-induced constipation).
The STC diagnostic workup includes a colonic transitional test, pressure measurement of anorectal, a balloon exploration test, and a barium enema. We defined a positive colonic transit test as patients who had greater than 20 % of radiopaque marker stasis in the colorectum after 96 h. Anorectal pressure measurement and the balloon exploration test were arranged to assure there was no outlet obstructed defecation and to rule out pelvic floor dysfunction. Patients underwent a barium enema to ensure there were no mechanical obstruction problems, and this investigation showed redundant colon in all cases. Colonoscopy was normal and anal ultrasound showed no disruption of the external anal sphincter in all cases. Suitable patients were those in complete accord with the colonic transition test greater than 96 h, but who had normal results on the barium enema, balloon exploration test, anal pressure measurement, colonoscopy, and anal ultrasound. Informed consent was provided before all examinations. The operations were performed by the same team.
In all, 32 patients were diagnosed with STC and were treated by laparoscopically assisted subtotal colectomy with preservation of the SRA in ileorectal anastomosis between January 2016 and January 2017 . Data on age, body mass index, preoperative laxative dependency, preoperative defecation duration, colonic transit time, operative time, estimated volume of blood loss, surgical complications, postoperative bowel movements, length of hospital stay, and functional outcome were recorded.
This study protocol was reviewed and approved by the Institutional Review Board of the Taiwan Adventist Hospital (TAHIRB No. 105 -E-10 ). It was conducted in compliance with the Helsinki Declaration. The patients provided written informed consent before surgery and patient information was anonymized and de-identified before analysis.
Patient characteristics are summarized using total number, percentages, and mean ±SD. All statistical analyses were performed with IBM SPSS statistical software version 22 for Windows (IBM Corp., Armonk, NY, United States).
Surgical technique
All the laparoscopic surgical procedures for preservation of SRA in STC patients were performed by two experienced colorectal surgeons who have experience of more than 100 laparoscopic and open colorectal cancer procedures annually. In all cases, the planned procedure was a laparoscopic subtotal colectomy with ileorectal anastomosis.The patients were placed in the modified lithotomy position under general anesthesia.Five trocars were used with the insertion of the primary trocar with a 10 mm port to gain access to the peritoneal cavity and establish the pneumoperitoneum above the umbilicus for the 30 ° laparoscope. The other four working ports were a 12 mm port in the right iliac fossa, a 10 mm port in the left iliac fossa, and a 5 mm port was placed in each of the right and left upper quadrants of the abdomen. Mobilization of the colonic segments was started at the right side of the colon. Mobilization was performed with the Endoshears (LigaSure device).
After the colon was fully mobilized, the colon was resected to the level of the junction of the rectosigmoid with a laparoscopic linear stapler. The rectal stump was mobilized to facilitate the transanally inserted circular stapler or Hegar dilator. The SRA was preserved in all patients (Figure 1 ).
A 4 -5 cm Pfannenstiel incision was made, and the mobilized bowel segment was brought out (Figure 2 ). The terminal ileum was divided a few centimeters proximal to the ileocecal valve with the anvil of a circular stapling device inserted into the lumen of the ileum. The ileum, with the anvil secured, was placed into the abdominal cavity.Finally, we performed the transanal end-to-end anastomosis using the circular stapling device. One Jackson Pratt drain was inserted into the pelvis, and the abdominal wall wounds were closed.
RESULTS
Thirty-two patients diagnosed with STC who had undergone laparoscopically assisted subtotal colectomy with preservation of the SRA in ileorectal anastomosis were included in the study. The preliminary data of these patients are presented in Table 1 .Eighteen of them (56 .2 %) were women. The mean age of our patients was 42 .6 ± 10 .4 years. The mean body mass index was 26 .6 ± 3 .1 kg/m2 .
All patients had severe constipation, the mean defecation duration was 9 .3 d and 3 (9 .4 %) patients had previous abdominal surgery. All patients complained of intermittent abdominal pain preoperatively. The mean operative time was 151 ± 29 .9 min. The mean estimated blood loss was 119 .1 ± 40 .7 mL (Table 2 ).
The mean time to the first flatus was 3 .0 ± 0 .8 d, and the average time to the first stool was 2 .5 ± 0 .5 d. The average time to first oral intake was 2 .8 ± 0 .8 d. The mean time of discharge from the ward was 10 .6 ± 2 .9 d. The satisfaction of post-operative patients was excellent in 28 (90 %) patients. The satisfaction was poor in 2 (5 %) patients due to a wound infection and an incisional hernia.
There were no intraoperative complications. Post-operative complications included 1 wound infection (Pfannenstiel incision wound), prolonged ileus (over 5 d) in 2 patients and three patients developed a urinary tract infection. One patient had an incisional hernia (Table 3 ). All cases could be fed orally with a clear liquid diet on the 4thpostoperative day. There was no major surgical complication and no patient required conversion to an exploratory laparotomy.
DISCUSSION
Constipation is a common condition. Most patients with constipation are treated with changes in their diet and the use of laxatives. If the condition proves recalcitrant, we should exclude secondary causes which may be underlying metabolic, organic or pharmacological factors. The mechanisms of slow transit include fewer colonic highamplitude propagated contractions or a reduced colonic contractile response to a meal[1 ]. The cause for STC is, however, unclear.
STC means a prolonged time in the transit of stools through the colon without an underlying systemic metabolic or pathologic disorder or pelvic floor dysfunction[11 ].Delays due to major dysfunction or innervation of colonic smooth muscle[12 ]. Patients with STC have an incorrect expression of serotonin receptors and incorrect responses to cholinesterase inhibitors[13 ,14 ]. The disease induced by a reduction in the interstitial cells of Cajal, which have a role in intestinal innervation and are situated in the submucosal and myenteric plexus of the bowel wall[15 ].
The enrollment criteria was done by the following steps. First, physiologic examinations for constipated patients are needed and include colonic transit studies with radiopaque markers, balloon tests, check anorectal pressure and defecation test[16 ].The radiopaque marker test is very helpful. Physiologic examination should include anorectal manometry to rule out the problem of pelvic floor dysfunction. All of our patients had anorectal manometry which revealed no abnormal anorectal inhibitory reflexes. A colonoscopy or barium enema is a good tool to provide evidence of any pathologic disease or structural lesions[17 ,18 ].
The incidence of AL following gastrointestinal surgery varies according to the site of anastomosis (all resections: 4 .3 %-13 %)[19 ]. Ischemia of the anastomotic region is one of the most significant factors leading to AL. Therefore, the preservation of the anatomical blood supply of the rectum is important. The effect of SRA-sparing on anastomotic healing and perioperative complications is poorly investigated. Sohnet al[20 ] have demonstrated that preservation of the SRA seems to be associated with a reduction of the leak rate in patients undergoing laparoscopic sigmoid resection for diverticular disease[20 ]. Beyond AL, an SRA sparing technique leads to preservation of the hypogastric nerves and thereby could potentially improve functional outcomes[20 ]. However, no studies have focused on the preservation of SRA with subtotal colectomy in STC patients. We observed no AL in our 32 STC patients who underwent an SRA-sparing operation. Although our study had a small sample size, the preservation of the SRA seems to have an excellent surgical outcome.
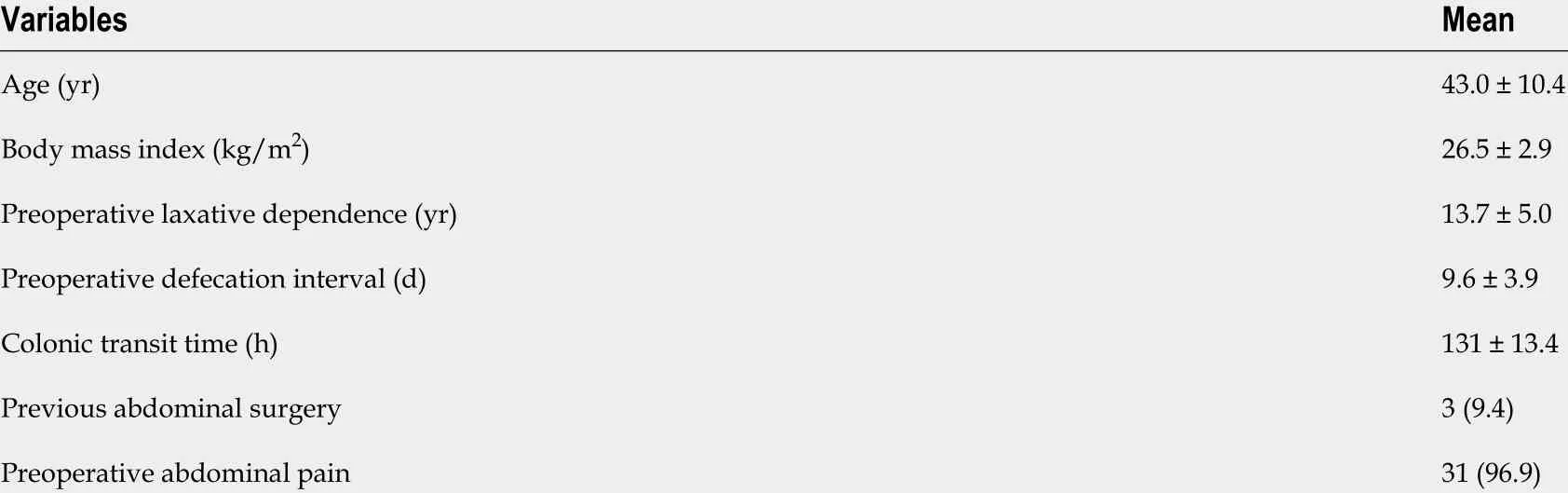
Table 1 Preoperative variables
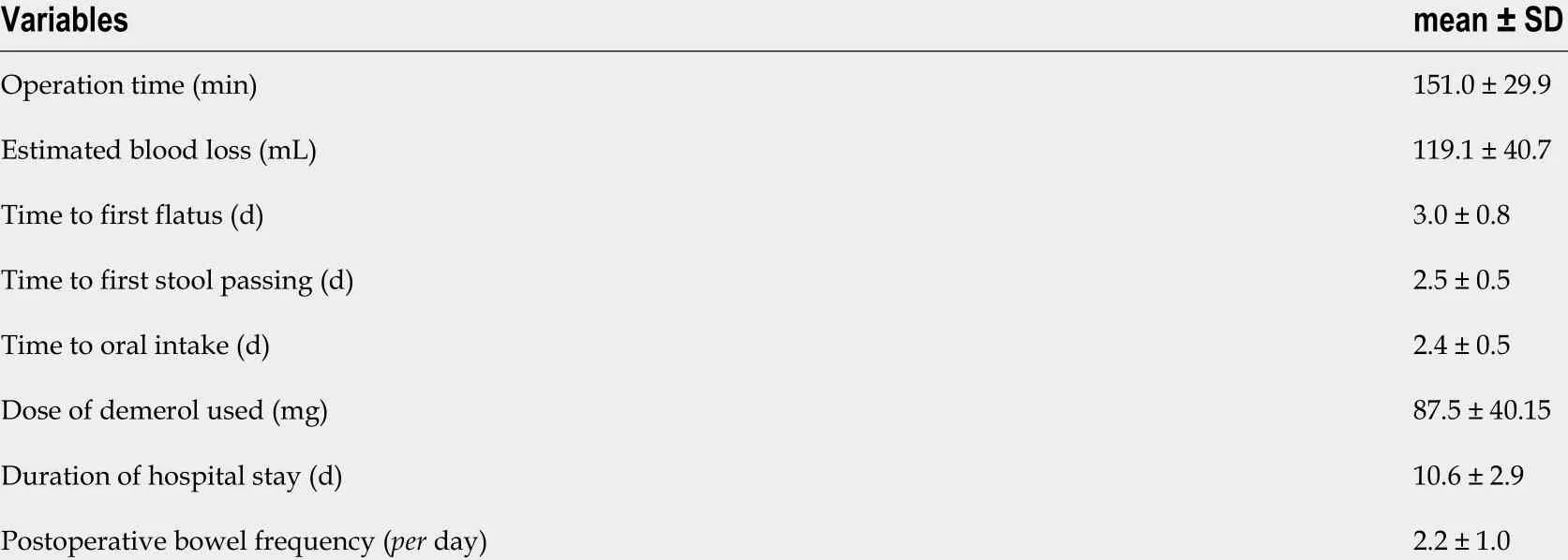
Table 2 Surgical and postoperative variables
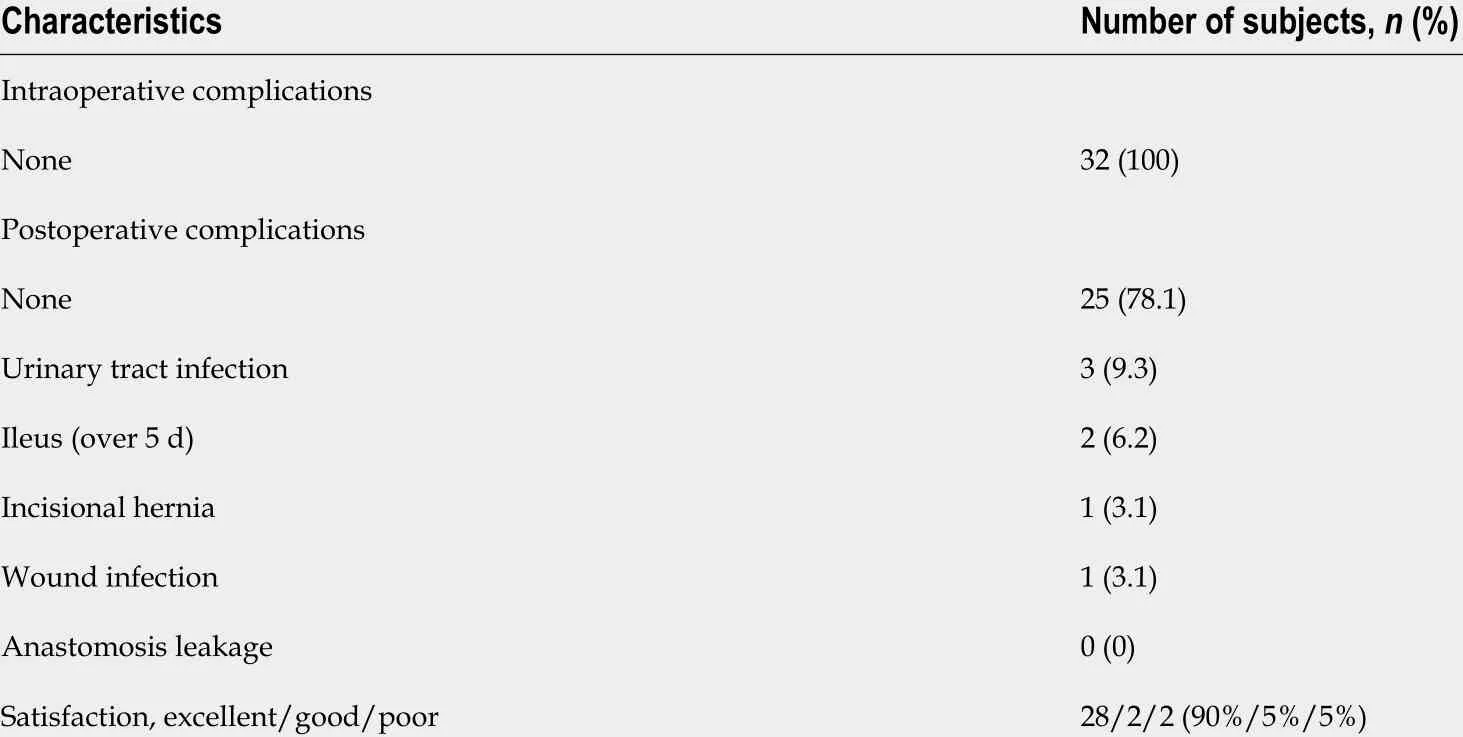
Table 3 Intraoperative and postoperative complications
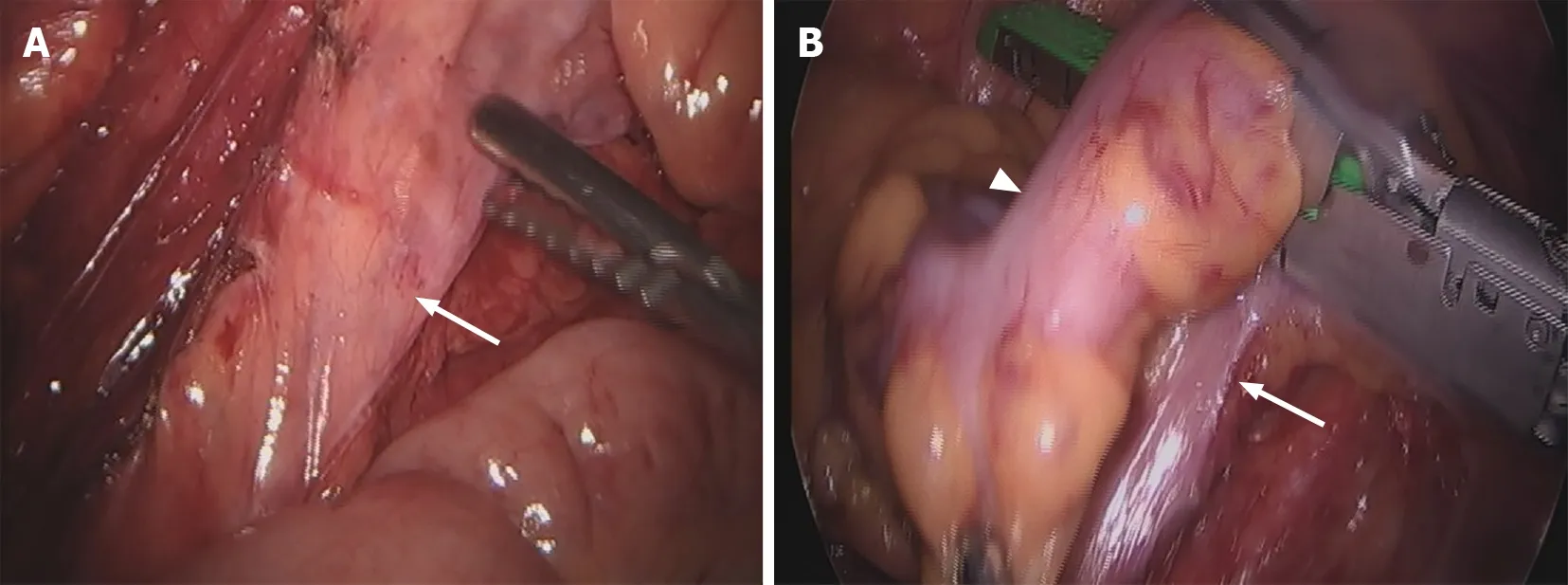
Figure 1 Colon. A: Preservation of superior rectal artery (arrow) in laparoscopically assisted subtotal colectomy with ileorectal anastomosis; B: Sigmoid-rectal junction (arrowhead) and sparing of the superior rectal artery (arrow).

Figure 2 Specimen after laparoscopic-assisted subtotal colectomy.
Laparoscopic techniques have been successfully used in colon surgery, thereby reducing morbidity, mortality and length of hospital stay[21 ,22 ]. The length of hospital stay is in the range of 7 to 13 d in STC patients[13 ,23 ,24 ], with postoperative ileus complicating the treatment course in many of them[7 ]. In our study, the mean hospital stay was 10 .6 ± 2 .9 d, and the mean number of days to the first flatus was 3 .0 ± 0 .8 d.
Abdominal distention with pain and vomiting all improved after surgery[25 ]. In a study by FitzHarriset al[26 ], although subtotal colectomy for slow-transit constipation increased bowel-movement frequency, the persistence of abdominal pain and diarrhea or postoperative incontinence adversely affected the quality of life following the surgery[26 ].
Preoperative counseling and an integrated post-operative functional and rehabilitational follow-up is important in patient underwent anterior rectal resection[26 ]. In a study by Sturialeet al[27 ], patients with defecation disorders, should receive an adequate re-educational process which often results in relevant clinical improvement for the patient[27 ]. Biofeedback therapy also shows effective treatment for fecal incontinence patient after anorectal operation[28 ].
A key limitation of the present study is its retrospective character. Moreover,technical aspects could have influenced the dissection technique. Thus, sparing of the mesosigmoid and the mesorectum can be performed much more easily today than at the beginning of the laparoscopic era, constituting a possible bias. This also explains the late publication of our data. Despite these limitations, and the bias involved through missing randomization, small sample size and surgeon preference of technique, we report the largest patient sample with vascular preservation in STC patients.
CONCLUSION
In conclusion, laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA is tolerated and can have better results with significant improvement in bowel function with careful patient enrollment criteria. No anastomosis leakage was noted in any of our patients; preservation of the SRA appears to result in excellent surgical outcomes.
ARTICLE HIGHLIGHTS
杂志排行
World Journal of Gastroenterology的其它文章
- Fecal microbiota transplantation for irritable bowel syndrome: An intervention for the 21 st century
- Hepatocellular carcinoma in viral and autoimmune liver diseases: Role of CD4 + CD25 + Foxp3 + regulatory T cells in the immune microenvironment
- Application of artificial intelligence-driven endoscopic screening and diagnosis of gastric cancer
- Mucosal lesions of the upper gastrointestinal tract in patients with ulcerative colitis: A review
- Early serum albumin changes in patients with ulcerative colitis treated with tacrolimus will predict clinical outcome
- Idiopathic mesenteric phlebosclerosis associated with long-term oral intake of geniposide