Barriers to the Implementation of Primary PCI in the Management of STEMI in Egypt
2021-06-08SamehShaheenAymanHelalandIslamAnan
Sameh Shaheen , Ayman Helal , and Islam Anan
1 Faculty of Medicine, Ain Shams University, Cairo, Egypt
2 Faculty of Medicine, Fayoum University, Fayoum, Egypt
3 Queen Alexandra Hospital, Portsmouth, UK
4 Faculty of Pharmacy, Ain Shams University, Cairo, Egypt
Abstract Introduction: Evidence-based guidelines recommend primary percutaneous coronary intervention (PPCI) be the mainstay reperfusion strategy for the treatment of ST-segment elevation myocardial infarction (STEMI) if it is performed in the proper time window.However, the Egyptian health care system is still struggling to provide such an important service.The aim of the present study, through a quantitative questionnaire, is to explore the current practice of STEMI management in Egypt, and to identify the barriers, opportunities, and potential areas for improvement.Methods and Results: The questionnaire was conducted in Egypt via face-to-face qualitative in-depth interviews with cardiologists from 14 PPCI-capable hospitals and 26 non-PPCI-capable hospitals.Participants were selected in view of their experience and knowledge.The study identified potential barriers to the implementation of PPCI among STEMI patients in Egypt.These barriers included the prehospital patient delay and emergency medical service delay,delay in the emergency department and delay in patient transfer to the CCU, unavailable equipment, catheterization laboratory activation delay, lack of trained interventional cardiologists, lack of regional STEMI networks and hospital policies, and insufficient ICU beds.Conclusion: Limited resources and health care system inadequacies have led to potential barriers that prevent suboptimal implementation of PPCI in Egypt.Efforts from all health care providers should be directed to overcome these identified barriers.
Keywords: ST-segment elevation myocardial infarction; primary percutaneous coronary intervention; barriers; Egypt
Introduction
Evidence-based guidelines recommend primary percutaneous coronary intervention (PPCI) be the mainstay reperfusion strategy for the treatment of ST-segment elevation myocardial infarction(STEMI) if it is performed in the proper time window.However, PPCI is performed in less than 25%of acute care hospitals [1].Many patients with STEMI present to hospitals that do not have on-site percutaneous coronary intervention (PCI) capabilities and therefore cannot undergo PCI within the time frames recommended in the guidelines;instead, they receive fibrinolytic therapy as the initial reperfusion therapy [2].Despite the availability and affordability of intravenous thrombolysis, the usefulness of this therapy is greatly limited by a high incidence of failed reperfusion and a substantial rate of reocclusion [1].In a recent study, the percentage of STEMI patients receiving PPCI in Egypt was much less than that of STEMI patients in European countries [3].
Study Objectives
The aim of the present study is to explore the current practice in STEMI management in Egypt, to assess the resources and capabilities of governmental hospitals, and to identify the most common gaps, barriers, and potential areas for improvement to widely provide PPCI in Egypt.
Study Design
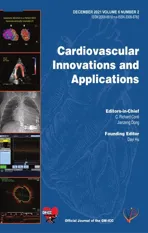
This survey was conducted in Egypt in January 2020 via face-to-face qualitative in-depth interviews that included a previously prepared unified questionnaire.Our team interviewed cardiologists from 14 PPCI-capable hospitals and 26 non-PPCIcapable hospitals in the Greater Cairo, Alexandria,Upper Egypt, and Delta and Suez Canal regions(Table 1).All hospitals were governmental public hospitals that are the main providers of health care services in Egypt.A hospital was considered to be a PPCI-capable center if it provides PPCI 24 h per day, 7 days per week (24/7).To include a wide range of hospitals, we included hospitals from different geographical locations and with differing ICU/CCU bed capacities: 6- 12 beds (43%), 15- 29 beds(29%), 31- 50 beds (2%), and more than 100 beds(7%).Also, among participating hospitals, the number of emergency department physicians ranged from 2 to 20, the number of ICU physicians ranged from 1 to 60, the number of interventional cardiologists ranged from 1 to 90, the number of qualified nurses ranged from 3 to 60, and the number of catheterization laboratory technicians ranged from 1 to 30.
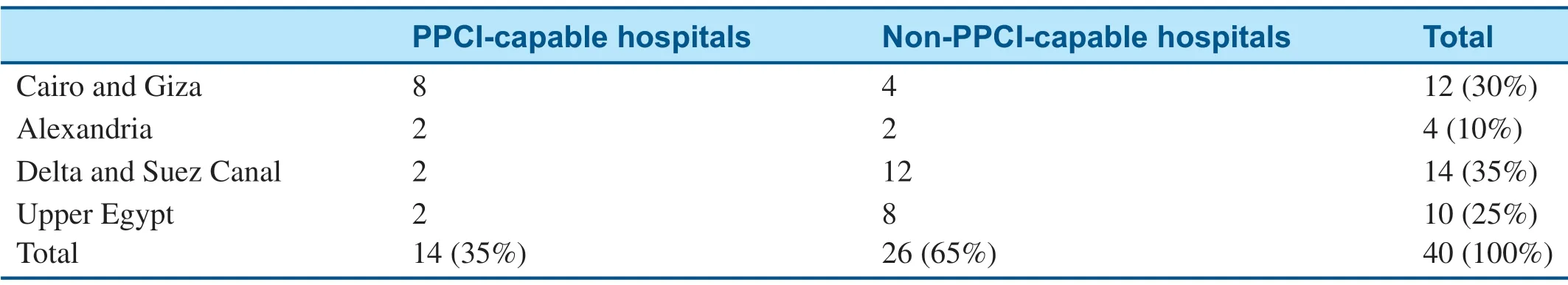
Table 1 Type and Geographical Location of the Participating Hospitals.
Results
Patient Presentation
STEMI patients presenting to PPCI-capable hospitals either arrived directly (71%) or were referred from another hospital (29%).The type of reperfusion did not differ significantly between the two groups: PPCI in 34% of the direct group versus 31% among the referred patients (P not significant).In non-PPCI centers, only 22% of patients arrived by ambulance, while 78% were self-transported.Only 29% of patients arrived at the hospital within 2 h of chest pain onset.
Interhospital Transfer
In PPCI centers, 96% of admitted STEMI patients were not transferred to another hospital for recovery or further management.In non-PPCI hospitals, only 38% were transferred to a PCI center and, when transferred, 81% were self-transported.Regarding the level of expertise required by the hospital policy to transfer a STEMI patient,81% of the transferred patients for primary PCI responded that only an emergency medical service (EMS) paramedic is required and not a nurse or physician.
Written Protocols
Only 21% of PPCI centers reported having written STEMI management protocols in place; the proportion is even less (8%) among non-PPCI hospitals.None of the PPCI centers had a regional STEMInetwork program.The reperfusion strategy is left to the discretion of the referring hospitals.None of the PPCI centers had written repatriation agreements with the non-PPCI centers in the region.
Quality Control Indicators
In PPCI centers, quality control indicators for STEMI diagnosis and management are variably monitored: door-to-balloon time in 79%, door-to-ECG time in 71%, door to catheterization laboratory activation time in 71%, and chest pain to device time and door-to-thrombolysis time in only 7%.Quality control indicators are less monitored in non-PPCI hospitals; 85% report in-hospital mortality, 50% report in-hospital morbidity, 23%report readmission rate, 15% report 30-day mortality, 73% report patients arriving within 2 h of chest pain onset, 50% report patients arriving at hospital by EMS, and 19% report door-to-needle time.
Hospital Resources and Coverage of Expenses
There is a cardiology department in 85% of the surveyed hospitals, there is an ICU/CCU in 96%,physicians are available 24/7 in the emergency department in 96%, ECG is available in the emergency department in 92%, a defibrillator is available in 88%, echocardiography is available in 73%, and troponin/creatine kinase estimation is available in only 42%.In PPCI centers, 87% of patients were covered by the Ministry of Health(MOH) and 6% were covered by the governmental Health Insurance Organization; in non-PPCI centers, 61% of patients were covered by the Ministry of Health, 2% were covered by the Health Insurance Organization, and 28% had to make outof-pocket payments.
STEMI Outcomes and Secondary Prevention
STEMI outcomes were perceived as less complicated by respondents in non-PPCI hospitals than by respondents in PPCI hospitals: STEMI patients fully recovered in 87% versus 75% of cases, in-hospital mortality was 2% versus 3%, in-hospital morbidity was 5% versus 13%, the readmission rate was 5%versus 6%, and 30-day mortality was 1% versus 3%.Secondary prevention strategies were applied less often in non-PPCI centers than in PPCI centers:acetylsalicylic acid was prescribed on discharge in 88% versus 93%, antiplatelets were prescribed in 88% versus 100%, statins were prescribed in 88%versus 93%, renin-angiotensin system blockers were prescribed in 81% versus 86%, patients were educated on risk modification in 73% versus 93%,and patients were referred for cardiac rehabilitation in 27% versus 64% (see Figure 1).

Figure 1 Management Outcomes of Patients with ST-Segment Elevation Myocardial Infarction in the Present Study.
Prehospital Delay
Prehospital delay is the main obstacle to timely reperfusion because of patients’ reluctance to seek medical advice, heavy traffic, searching for an available bed in a PPCI hospital, lack of EMS role, and the absence of regional networks (Figure 2 ).Only an estimated 29% of the patients presenting with STEMI to non-PPCI hospitals arrive at the hospital within 2 h of chest pain onset; for PPCI centers the proportion is 24%.Also, 71% arrive directly at the hospital, while 29% are transferred from other hospitals (Figure 3).EMS were used by only 35%of patients arriving at PPCI-capable centers and by 51% of patients presenting to non-PPCI capable centers.

Figure 2 Delays in the Journey of Patients with ST-Segment Elevation Myocardial Infarction (STEMI) in Egypt.ED, emergency department; EMS, emergency medical service; PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention.
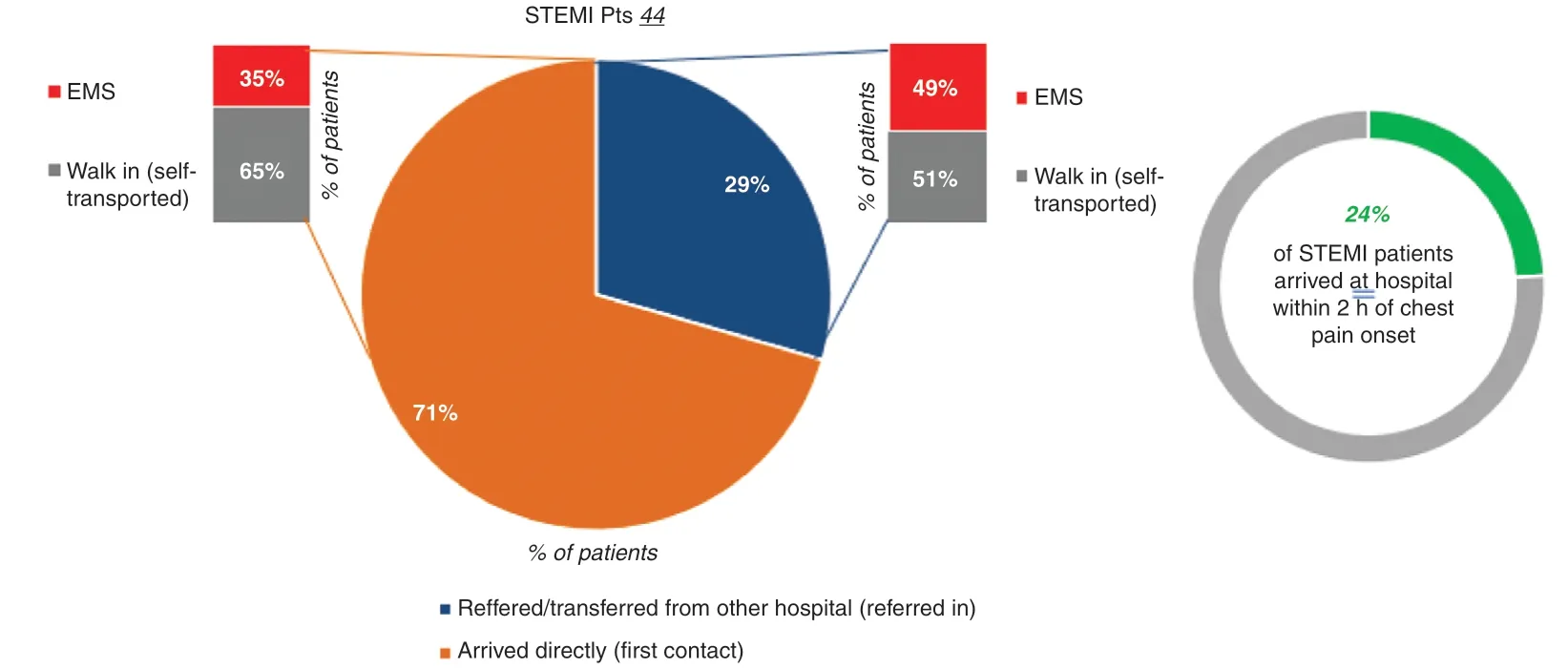
Figure 3 Proportions of Patients Presenting at the Emergency Department with ST-Segment Elevation Myocardial Infarction(STEMI).EMS, emergency medical services; Pts, patients.
Emergency Department Delay
A delay is also observed in the emergency department because of high patient numbers.According to the surveyed non-PPCI centers, as many as 13%of patients presenting to the emergency department have STEMI.On the other hand, 5% of patients presenting to the emergency department of PPCIcapable centers have STEMI.Among non-PPCI hospitals, only 42% of STEMI patients are transferred to PPCI centers.The barriers are as follows(see Figure 4): long estimated time for patient transfer, and limited availability of EMS, an accompanying physician, and vacant CCU beds at the PPCI hospital.The transfer of patients to the CCU before the procedure rather than to the catheterization laboratory directly also adds more delay in STEMI management.
Figure 4 Barriers in Transferring Patients From Non-Percutaneous Coronary Intervention (PCI)-Capable Centers to PCI-Capable Centers.EMS, emergency medical services; HIO, Health Insurance Organization; STEMI, ST-segment elevation myocardial infarction.
Catheterization Laboratory Delay
Most non-PPCI hospitals have a catheterization laboratory but it operates for less than 12 h in 84%of the non-PPCI hospitals, and 36% of patients arrive after the operating hours.This highlights the underutilization of the limited yet available resources.Even during catheterization laboratory operating hours, only 23% of the questionnaire respondents will perform PPCI.This may point to other obstacles, such as unavailability of essential equipment or lack of expertise for PPCI.Moreover, the time for catheterization laboratory activation and the time until the catheter team arrives may add more delay to the process (Figure 5).In 79% of cases, the catheterization laboratory is activated by the cardiologist and not the emergency department physician.Some essential PPCI equipment may not be available, and patients may pay for some items.Thus, 24% of patients presenting directly to PPCI-capable centers may end up receiving thrombolytic therapy(Figure 6).

Figure 5 Catheterization Laboratory Activation Process.ED, emergency department; PPCI, primary percutaneous coronary intervention.

Figure 6 Management of Patients with ST-Segment Elevation Myocardial Infarction (STEMI).PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; Pts.patients.
Postprocedural Barriers
Among PPCI hospitals, the most common place for immediate recovery after PPCI is the CCU/ICU in 93% of hospitals.Unavailability of CCU/ICU beds after the procedure and the absence of a repatriation policy are barriers to PPCI implementation in some cases.In this study, 64% of respondents do not use early discharge for STEMI patients after the procedure.
Summary
The barriers for providing the best medical service for patients presenting with STEMI in Egypt are summarized in Figures 7 and 8 for PPCI-capable centers and non-PPCI-capable centers, respectively.Limited resources, lack of trained interventional cardiologists, insufficient numbers of CCU beds,lack of regional STEMI networks, and lack of hospital policies are among the main barriers in the management of STEMI patients in Egypt.
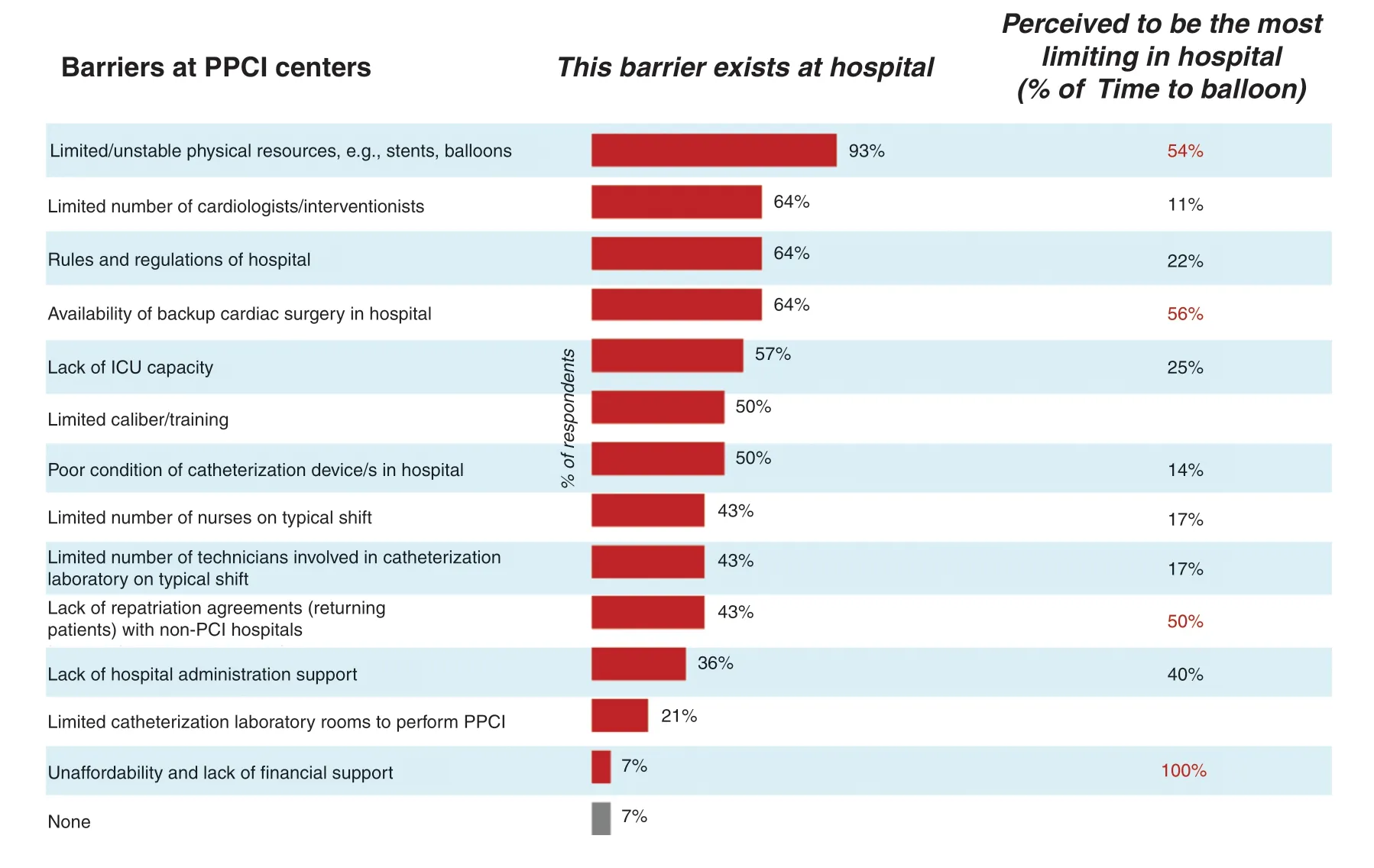
Figure 7 Barriers in Primary Percutaneous Coronary Intervention (PPCI)-Capable Centers.PCI, percutaneous coronary intervention.
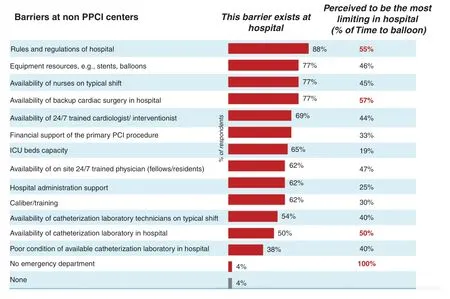
Figure 8 Barriers in Non- Primary Percutaneous Coronary Intervention (PPCI)-Capable Centers.PCI, percutaneous coronary intervention.
Discussion
Rapid myocardial reperfusion is the cornerstone of treatment for patients with STEMI.For every 30-min delay in the treatment of patients with STEMI, the risk of death increases by 7.5%; therefore, minimizing delay is crucial [4].
In the present study, according to the questionnaire respondents, only 22% of patients arrive in an ambulance, while 78% walk in (self-transported).Only 29% of patients arrive at the hospital within 2 h of chest pain onset and only 38% of patients admitted to non-PCI hospitals are transferred to a PCI center.
Shaheen et al.[3] evaluated data from 19 Egyptian centers (with and without PCI facilities) with 1356 patients, who were compared with 7420 patients from other European Society of Cardiology (ESC) countries to describe the characteristics of patients with STEMI, to assess STEMI management patterns, to evaluate the organization of STEMI networks across Egypt, to evaluate in-hospital patient outcomes, and to compare Egyptian patients with patients from other ESC countries.Compared with patients from other ESC countries, Egyptian patients had longer median pain to first medical contact time, 120 min(range 60- 240 min) versus 100 min (range 50-240 min), P < 0.001.This is due to both patient delay and system delay.Self-presentation rather than EMS presentation was the mode of admission in 86.06%of patients in Egypt versus 25.83% in EU countries(P < 0.001).The initial reperfusion therapy rates were 49.12%, 43.07%, and 7.26% for PPCI, thrombolytic therapy, and no reperfusion, respectively, in Egypt versus 85.42%, 7.26%, and 7.82%, respectively, for EU countries.Thrombolytic therapy is still the most common reperfusion strategy in patients with STEMI in Egypt.They stated that there is an urgent need for public awareness and patient education campaigns to instruct patients with chest pain to seek medical advice as early as possible together with improving the EMS performance in Egypt to become a dependable and efficient mode of STEMI patient transfer.Moreover, the number of PPCIs per million population is very small because of the limited number of PPCI centers also not connected to the non-primary PCI capable centers.A pharmaco- invasive approach might be a practical way of treating STEMI patients as a temporary solution until the development of a STEMI referral network.
The China STEMI Care Project was started in 2011 to evaluate the problems of insufficient reperfusion and delay in treating patients with STEMI in China.A total of 4,191 patients with STEMI with symptom onset within 12 h or between 12 h and 36 h were enrolled from 53 tertiary PCI hospitals in 14 provinces in China.Among them, 49% were self-transported, 26.5% were transported by calling the EMS directly, and 24.5% were transferred from other hospitals.About 83.2% of patients received PPCI, 5.9% received thrombolysis, and 10.9%received conservative treatment.The median doorto-balloon time was 115 min (range 85- 170 min)and the median door-to-needle time for in-hospital thrombolysis was 80 min (range 50- 135 min).It was concluded that although a long treatment delay and a high proportion of patients transporting themselves to the hospital were observed, the trends were positive, with greater adoption of PPCI and lower in-hospital mortality in tertiary hospitals in China.Therefore, these results provide important information for the need for future integrated STEMI network construction in China [5].
Yin et al.[6] conducted a study to understand the current STEMI treatment process in Guangdong province in China to provide recommendations for improvement.Data were collected by face-to-face interviews from 32 participants, including patients with STEMI, cardiologists and nurses from hospitals, emergency department physicians, primary health care providers, local health governors, and coordinators at the EMS.The patients’ barriers are unawareness of STEMI symptoms and self-transfer rather than calling the EMS.The main system barriers are the limited capacity of health professionals in hospitals and lack of coordination between hospitals They made five important recommendations to improve STEMI care in Guangdong province:(1) public education; (2) strengthening the primary health care workforce; (3) increasing EMS capacity; (4) establishing an integrated care model; and(5) harnessing the government’ s responsibilities.
In the present study, only 21% of PCI centers reported having STEMI management protocols in place; the proportion was even less (8%) among non-PCI hospitals.None of the PCI centers had a regional STEMI network program.None of the PCI centers had written repatriation agreements with the non-PCI centers in the region.One of the reasons cited by participants for nondelivery of PPCI is that there was no medical code for the procedure after thrombolytic therapy.This prevented the participating centers from seeking reimbursement, which translated into underutilization of postthrombolytic PPCI.Logistical issues were cited as another reason for the underimplementation of PPCI, such as the lack of written protocols for EMS interhospital transfer.Operational gaps exist, and a multidisciplinary approach to the continuum of care between the EMS and hospitals remains a major challenge in Egypt.The absence of prehospital ECG recording and interpretation in EMS vehicles adds to the problem of diagnosis delay.Furthermore, EMS paramedics are not trained to perform, interpret, or send ECGs to receiving centers.Other obstacles include insufficient numbers of trained interventional cardiologists, nurses, and/or technicians to provide a 24/7 PPCI service and the unsustained flow of availability of consumable equipment such as stents, guide wires, balloons, and contrast agents.These limitations are especially apparent outside Cairo.
Dakota et al.[7] evaluated the door-in to doorout (DIDO) delays as a routine performance measure of a metropolitan STEMI network.Data from 1,076 patients with acute STEMI who were transferred by ground ambulance to a PPCI center demonstrated that the median DIDO time was 180 min(range 120- 252 min) and that in turn led to a significant increase in the total ischemia time (r= 0.4,P < 0.001).The median door-to-device time was 70 min (range 58- 88 min).They concluded that to improve the overall performance of PPCI in the region, interventions aimed at reducing the DIDO time at the initial hospitals are the best efforts in reducing the total ischemia time.
Although most efforts have been made to reduce in-hospital delays, prehospital delays are a major factor in the total delay in STEMI reperfusion.Patient education, especially symptom awareness programs, is the most important step in delay reduction.It is mandatory to educate the public about ischemic symptoms and the importance to immediately contact the EMS once they have any symptoms suspicious of myocardial ischemia.In the present study,the prehospital phase delay was the main obstacle to timely reperfusion because of patients’ reluctance to seek medical help, heavy traffic, searching for a hospital ready to offer PPCI, lack of EMS role, and lack of regional networks.A long time for patient transfer, and limited availability of EMS, an accompanying physician, and CCU beds at the PPCI center are the major obstacles to patient transfer from non-PCI-capable centers to PCI-capable centers.
The American Heart Association recommends the PreAct STEMI algorithm be applied to patients with ischemic symptoms and/or EMS suspicion of STEMI.It recommends three modes of prehospital ECG interpretation: paramedic interpretation,computerized algorithm diagnosis, and ECG transmission for remote interpretation.Patients who fulfill the STEMI criteria should be directly transported to the nearest PPCI-capable center, while those who do not fulfill the criteria should be transported to the emergency department for further management.Prehospital identification of STEMI has been successfully implemented in many regions by training EMS personnel to make STEMI-focused interpretations of 12-lead ECGs and by funding to train and equip EMS personnel to acquire, interpret, and transmit the prehospital ECG [8].
Hoedemaker et al.[9] evaluated the transfer time by ambulance to PPCI centers in the Netherlands and the impact of expansion of off-site PCI centers (PCI centers without surgical backup).They used data from EMS records to estimate the ambulance driving time from each postal code on each route.There were 14 off-site and 16 on-site PCI centers.The median time to on-site PCI centers was 18.8 min (range 12.2- 26.3 min) compared with 14.9 min (range 8.9- 20.9 min) to any PCI center (P < 0.001).In areas that were impacted by the initiation of off-site PCI, the median driving time significantly decreased from 25.4 min (range 18.2- 33.1 min) to 14.7 min(8.9- 20.9 min) (P < 0.001).On the basis of a computational model, timely ambulance transfer to a PCI center within 120 min is available for all postal codes in the Netherlands.Expansion of off-site PCI has significantly reduced the driving time to PCI centers.
The Health Professions Council of South Africa approved the use of prehospital thrombolysis for emergency care practitioners in 2009 [10].However,since its approval, prehospital thrombolysis has failed to reach a level of systematic uptake indicative of successful implementation.Lynch et al.[10]studied the barriers to prehospital thrombolysis in South Africa.They demonstrated that the cost,logistics, interprofessional collaboration, leadership engagement, and beliefs or skepticism associated with prehospital treatment are the most important barriers in preventing delay in STEMI management.They concluded that a lack of strategic implementation has resulted in the poor introduction of evidenced-based prehospital cardiac care, affecting vulnerable populations who may have otherwise benefited from receiving this level of care.
In the present study, a delay in performing revascularization in STEMI patients was observed in the emergency department because of high patient flow.A recent study using the Korean PCI registry demonstrated a median pain-to-door time of 94 min and a median door to balloon time of 62 min [11].Lee et al.[12] evaluated 4,874 patients with STEMI from the Korean acute myocardial infarction registry.They found that older age, female sex, and avoiding use of the EMS were associated with a longer pain-to-door time.
In the present study, the transfer of patients to the CCU before the procedure rather than the catheterization laboratory directly also added more delay in STEMI management.The time for catheterization laboratory activation and the time until the catheter team arrive may add more delay to the process.A recent study found that using a smartphone led to a significant decrease in total ischemia time in patients with STEMI because of rapid communication that led to a decrease in the time needed for transfer from non-PPCI-capable centers to PPCIcapable centers.Patients using a smartphone had a shorter first medical contact to device time than other patients (102.5 min versus 129.5 min, P = 0.031).Prehospital triage via telemedicine led to effective reduction of the pain-to-reperfusion time [13].
The STEMI-India Task Force Writing Committee for Management of STEMI in Low- and Middle-Income Countries recently published the essential components of an effective STEMI care program.This includes five important items: (1) developing a personalized care strategy that targets therapies in a uniquely specific manner that includes rapid mobilization to a reperfusion center or a pharmaco- invasive strategy when PCI is not available; (2) creating a STEMI system of care involving the governments;(3) introducing performance measures for STEMI care that should be educational; (4) creating an easily accessible system of paying for care at any approved STEMI care facility, both public and private- this should eliminate upfront out-of-pocket payments;(5) having a strong component of program evaluation, performance measures, and outcomes [14].
A limitation of this study is that only governmental hospitals were included in the questionnaire.Private hospitals might have different obstacles and limitations as regards PPCI implementation among STEMI patients.However, most of the obstacles discussed in this study are common among most health care sectors in Egypt.Further research is warranted to further explore the obstacles and whether there has been any improvement in the health care system in this regard.
Recommendations
The following actions are needed to optimize STEMI management in Egypt: public awareness campaigns and patient education; improving the EMS in terms of the number of vehicles, call centers, trained personal, and equipment on board;increasing the number of PPCI-capable centers,starting from those centers that already have catheterization laboratories that provide only elective nonemergency services; building regional STEMI networks with written protocols for interhospital transfer; extending reimbursement for PPCI to the first 24 h after thrombolytic therapy; and endorsing training courses for interventional cardiologists and other health care professionals for better diagnosis and management of STEMI.
Conclusion
Limited resources and health care system inadequacies in Egypt have led to insufficient implementation of PPCI.The potential barriers include lack of trained interventional cardiologists, insufficient numbers of CCU beds, and lack of regional STEMI networks and hospital policies.Governmental efforts should be directed toward these barriers to ensure the best quality of management for patients presenting with STEMI.
Conflict of Interest
None.
Funding
Limited grant from Sanofi Egypt.
Acknowledgments
We thank Raghda Fekry and Ahmed Fawzy for their active participation in conducting the survey.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Comparison of a 5 F Microtube-Irrigated Ablation Catheter and a General Ablation Catheter in the Treatment of Resistant Hypertension with Renal Denervation
- Main Renal Artery Plus Branch Ablation in the Treatment of Resistant Hypertension with Renal Denervation
- Clinical Significance of Angiographically Detectable Neovascularity in Patients with Cardiac Myxoma
- ST-Segment Depression in Leads I and aVL:Artifactual or Pathophysiological Findings?
- A Case Report of Radiofrequency Ablation of Typical Atrial Flutter Combined with Atrial Tachycardia