Acute syndesmotic injuries in ankle fractures: From diagnosis to treatment and current concepts
2021-05-20FrancescoPogliacomiMassimoDeFilippoDanieleCasaliniAlbertoLonghiFabrizioTacciRoccoPerottaFrancescoPagniniSilvioToccoFrancescoCeccarelli
Francesco Pogliacomi, Massimo De Filippo, Daniele Casalini, Alberto Longhi, Fabrizio Tacci, Rocco Perotta,Francesco Pagnini, Silvio Tocco, Francesco Ceccarelli
Francesco Pogliacomi, Department of Medicine and Surgery, Orthopaedic Clinic, Parma 43126, Italy
Massimo De Filippo, Daniele Casalini, Alberto Longhi, Fabrizio Tacci, Rocco Perotta, Francesco Pagnini, Francesco Ceccarelli, Department of Medicine and Surgery, University of Parma, Parma 43126, Italy
Silvio Tocco, Centro Riabilitativo della Mano e Arto Superiore, Parma 43121, Italy
Abstract A stable and precise articulation of the distal tibiofibular syndesmosis maintains the tibiofibular relationship, and it is essential for normal motion of the ankle joint.The disruption of this joint is frequently accompanied by rotational ankle fracture, such as pronation-external rotation, and rarely occurs without ankle fracture.The diagnosis is not simple, and ideal management of the various presentations of syndesmotic injury remains controversial to this day.Anatomical restoration and stabilization of the disrupted tibiofibular syndesmosis is essential to improve functional outcomes.In such an injury, including inadequately treated, misdiagnosed and correctly diagnosed cases, a chronic pattern characterized by persistent ankle pain, function disability and early osteoarthritis can result.This paper reviews anatomical and biomechanical characteristics of this syndesmosis, the mechanism of its acute injury associated to fractures, radiological and arthroscopic diagnosis and surgical treatment.
Key Words: Ankle; Fracture; Injury; Distal tibiofibular joint; Trauma; Syndesmosis
INTRODUCTION
The distal tibiofibular syndesmosis (DTS) complex is critical for maintaining the congruency of the ankle mortise[1] and is the most important supporter of this joint[2].DTS injuries of sufficient severity can disrupt the normal stability of the ankle and they may occur in many forms, commonly classified into isolated or, more frequently, with an associated malleolar fracture[3].They are consequent to an external rotation force applied to the foot that leads to eversion of the talus within the ankle mortise[4-6].Ankle fractures occur with an incidence of 107-148 per 100000 in the adult population[7-9].About 10% of all are associated to syndesmotic injury, and this percentage is twice as high in patients who require internal fixation[10].Therefore, it is crucial that surgeons adequately diagnose these lesions, which are present in up to 40% of all type B injuries according to Danis-Weber classification and up to 80% of all type C[11].Persistent ankle pain, function disability and early osteoarthritis are potential problems related to misdiagnosed or inadequate treatment[12-14], and for this reason it is necessary to acquire an accurate diagnosis and maintain syndesmotic reduction when treating ankle fractures with concomitant syndesmotic disruption.
Patients with unstable injuries require surgical stabilization[15].Various fixation techniques have been introduced over recent decades (metallic and bioabsorbable screws, staples, polyester bands, syndesmosis hooks, Kirschner wires and suturebutton fixation)[2,16-18].Static fixation (SF) with one or more cortical screws is the reference standard fixation method.However, some significant issues should be considered.Screw loosening, breakage[19], discomfort, pain related to overcompression, the need for a reoperation for screw removal and the risk of late diastasis after early removal are potential drawbacks of this type of fixation[20-24].An alternative dynamic method of fixation (DF) uses an implanted suture-button device; it consists of a nonabsorbable synthetic suture between two metallic buttons implanted across the DTS[25].Recently, this technique has become increasingly popular because it allows a more physiological articular movement, early rehabilitation, satisfactory functional outcomes and no requirement for implant removal[2,25].However, there is no unique consensus on whether DF methods are superior to the static ones in terms of functional outcomes, change in range of motion, complication rates and incidence of reoperation[26,27].The aim of this study is to review anatomical and biomechanical characteristics of DTS, the mechanism of its acute injury associated to fractures, radiological and arthroscopic diagnosis and surgical treatment.
ANATOMY AND BIOMECHANICS
The bony anatomy of the distal tibia and fibula is important for the osseous stability of the tibiofibular joint, which is a syndesmosis formed by the medial rough convex surface of the distal fibula which articulates with the lateral triangular fibular notch of the distal tibia[1,28].The lateral ridge of the distal tibia bifurcates into an anterior and posterior margin, forming a larger anterior (Chaput’s tubercle) and a smaller posterior tubercle (Volkman’s tubercle).These tubercles represent the tibial attachment sites respective of the anterior and posterior syndesmotic ligaments.Posterior tubercle functions as a fulcrum during external rotation injury, and the fibula spins around its longitudinal axis.Between the anterior and posterior margins of the tibia there is a triangular concave notch, named incisura tibialis, where the convex medial margin of the distal fibula rests.In about 75% of ankles, there are cartilage covered facets at the tibiofibular contact zone, forming a true synovial joint[29].This articulation can act as a guide for the alignment of the ankle mortise in ankle fracture fixation or in syndesmosis reconstruction.
The ligamentous structures of the syndesmosis (Figure 1) function in addition to the bony support to provide syndesmotic stability by resisting the axial, rotational and translational forces.The distal syndesmosis complex may be further divided into its four components as follows[30].
The anterior inferior tibiofibular ligament (AITFL) traverses the joint at an oblique 45° angle from the Chaput’s tubercle of the tibia to the Wagstaffe-Le Forte tubercle of the fibula.It is often composed of three bundles forming a trapezoidal shape.Rarely, an accessory anteroinferior tibiofibular ligament (Bassett’s ligament) runs parallel and inferior to the AITFL.AITFL is the weakest of the syndesmotic ligaments and is the first ligament subjected to stress during an external rotation force of the fibula around its longitudinal axis.
The posterior inferior tibiofibular ligament (PITFL) is the strongest portion of the complex, and it lies in the posterior surface of the syndesmosis.From its origin, at the Volkman’s tubercle, it descends posterolaterally to insert in the posterior aspect of the distal fibula.Tear of PITFL can occur in Lauge-Hansen supination-eversion, pronationabduction or pronation-eversion injury.However, in these cases, forces usually result in a posterior malleolar avulsion fracture due to the ligament strength[31].
The interosseous ligament is formed by a thickening of the lowermost end of the interosseous membrane.This ligament functions as a “spring” to accommodate slight separation of the mortise during dorsiflexion of the ankle.The interosseous membrane connects the tibia and fibula throughout their length and plays a minimal role in syndesmotic stability[32].
The transverse tibiofibular ligament extends horizontally from the proximal margin of the fibular malleolar fossa to the dorsodistal rim of the tibia distal to the PITFL; it may protract to as far as the dorsal aspect of the medial malleolus[31].It has a fibrocartilagineous appearance that functions as a labrum to deepen the posteroinferior rim of the tibia.The presence of another ligament, the posterior intermalleolar ligament, is still controversial.Its occurrence varies from 19% in magnetic resonance imaging to 82% in dissected anatomical specimens[33].Although the posterior intermalleolar ligament has been neglected in the anatomy literature, the existence of this ligament has been revealed recently to be a cause of posterior impingement syndrome that brings about posterolateral ankle pain during plantar flexion[34,35].Furthermore, radiological studies have demonstrated that this ligament is an almost invariably present anatomical entity[36,37].However, its anatomical role is still unknown.
In a study based on computed tomography (CT) imaging of 100 normal syndesmosis, Elgafyet al[38] showed variation of the articulation between genders, with variation between the anterior and posterior dimensions within the syndesmosis.This diversity of the articulation poses both diagnostic and operative challenges to the practitioner.
Despite a small amount of motion, DTS has a very important role in ankle joint biomechanics even if only very small rotations and displacements are detected indicating that the fibula is closely attached to the tibia.With the ankle in external rotation, the fibula translates medially (0-2.5 mm) and posteriorly (1.0-3.1 mm) and externally rotates (2°-5°), even though this little displacement cannot be estimated on radiographs[39].While moving from plantar flexion to dorsiflexion, Peteret al[40] reported a 2° external rotation and 1.25 mm lateral translation of the lateral malleolus to accommodate the irregularly shaped talus.
The disruption of ligamentous structures around the ankle modifies this “equilibrium.” Anatomical study suggested the relative importance of any syndesmotic ligament to the overall syndesmotic stability (35% by AITFL, 22% by interosseous ligament, 9% by superficial PITFL and 33% by deep PITFL)[41].Sectioning of the AITFL results in the greatest reduction in resistance to external rotation, although there is a significant decrease in resistance with each sequential ligament sectioned.In contrast, sectioning of the PITFL results in the greatest decrease in resistance to internal rotation[42].Additionally, the deltoid ligament confers secondary stability by resisting lateral shift of the talus[43].Ramseyet al[44] reported that when the deep horizontal part of the deltoid ligament is cut, this diastasis increases to 3.7 mm and described that when the talus moves laterally by 1.0 mm, the contact area in the tibiotalar articulation is decreased by 42%.
Moreover, Burnset al[45] showed that a complete disruption of syndesmosis with a deltoid ligament tear caused a 40% decrease in the tibiotalar contact area and a 36% increase in the tibiotalar contact pressure.Therefore, a precise and stable articulation is required for normal motion of the ankle.

Figure 1 Anatomy of the distal tibiofibular syndesmosis: anterior view, posterior view, lateral view and proximal and distal coronal view.
MECHANISM OF INJURY AND CLASSIFICATION
Although the precise mechanism of injury in the DTS often remains unclear, it has been demonstrated that these lesions occur more frequently with some types of rotational ankle fractures such as in pronation-external rotation and pronationabduction and less frequently in supination-external rotation[34].
The most frequently used ankle fracture classifications are the Danis-Weber, AOMüller, and Lauge-Hansen.The Weber classification (Figure 2) is based on the position of the distal fibular fracture in relation to the syndesmosis.Weber A includes fractures below the level of the syndesmosis, those at the level of the syndesmosis are Weber B, and Weber C includes fractures above the level of the syndesmosis.Type C also includes rotational ankle traumas with high fibular rupture, the so-called “Maissoneuve fractures,” which are usually associated to syndesmotic disruption.The syndesmosis is rarely involved in Weber A fractures, although it is torn in up to 80% of all type C injuries[7,12].In this case, we have disruption of the deltoid ligament caused by external rotation and peroneal fracture above the level of distal syndesmosis.The status of the syndesmosis is unclear in Weber B lesions caused by an external rotation mechanism, but some studies report lesions in up to 40% of cases[7,12].
In the AO/OTA classification, ankle fractures are classified as infrasyndesmotic (correlating to Danis-Weber Type A injuries), trans-syndesmotic (correlating to Danis-Weber Type B injuries) or suprasyndesmotic (correlating to Danis-Weber Type C injuries) with other subsets based on the presence or absence of medial or posterior malleolar injuries[46,47].This contrasts with the Danis-Weber classification that ignores the medial and posterior structures.AO/OTA classification system also includes the fracture patterns described by Lauge-Hansen and Danis-Weber[47].
The Lauge-Hansen classification system instead gives more information about the mechanism of injury and anatomic structures involved, and it divides these fractures in four categories and other subgroups.It includes mechanism (with the position of the foot supinated or pronated), the direction of the force at the moment of the trauma (a force causing abduction, adduction or external rotation) and has multiple stages for each type depending on severity[48].Lauge-Hansen used amputated limbs to divide ankle fractures in which the position of the foot at the time of the traumatic event and to the direction of the forces were crucial points for the injury mechanism knowledge.

Figure 2 Radiographs representing the three types of ankle fractures according to Danis-Weber.
In supination external rotation injuries, the most commonly occurring of Lauge-Hansen’s categories, the lateral structures are under stress, and the medial structures are finally compromised.In Stage 1 the talus rotates laterally and pushes the lateral malleolus posteriorly stressing the AITFL that is injured.In Stage 2 progressive external rotation in supination and lateral rotation of the talus results in an oblique or spiral fracture of the distal fibula.Stage 1 and stage 2 are considered stable injuries or fractures.With more force, in Stage 3, the PITFL is injured, or the posterior malleolus (PM) is fractured.Finally, in Stage 4, the medial malleolus is fractured, or the deltoid ligament is disrupted.
Supination adduction injuries are caused by compression force under the medial ankle structures and traction of the lateral ankle structures.In stage 1 either a transverse fracture of the lateral malleolus below the level of the tibial plafond is produced, or the lateral ligaments of the ankle are avulsed of the distal fibula.In Stage 2, either a vertical medial malleolus fracture or injury to the deltoid ligament occur.
In pronation external rotation lesions the foot is pronated, and the deltoid ligament is stressed; this mechanism produces injury of the medial ankle structures.In addition, the external rotation involves the lateral and posterior ankle structures.This results in fibula and PM fractures.In Stage 1 with either deltoid ligament rupture or avulsion, fractures of the medial malleolus are evident.Injuries of the AITFL occur in Stage 2, oblique or spiral fibula fractures proximal to the level of the tibial plafond are observed in Stage 3, and fractures of the PM or injury to the PITFL occur in Stage 4.
In pronation abduction injuries the abduction of the talus causes traction of the medial ankle structures.Stage 1 injuries involve rupture of the deltoid ligament or transverse fractures of the medial malleolus, whereas Stage 2 injuries are associated with damage to the AITFL.In Stage 3, transverse or comminuted fibula fractures were observed above the level of the tibial plafond[47-49].
In conclusion, ankle fractures that are more frequently associated to DTS injuries are those localized over the syndesmosis.Less frequently, these lesions are present in fractures at the level of the syndesmosis and rarely in those positioned under.Concomitant traumas of the medial structures may influence the correct reduction of the fibula inside the tibia at this level and consequently the prognosis.
CLINICAL AND INSTRUMENTAL EXAMINATION
Patients affected by syndesmotic injuries associated to fractures are characterized by swelling, instability and pain at rest that makes loading impossible and is exacerbated by palpation and compression[50].
Several specific syndesmosis tests have been described.The squeeze test consists of compressing the tibia against the fibula at the mid-point of the calf, thus inducing a movement separating the two bones distally[51].The test is considered positive when it produces a distal pain around the interosseous ligament[52].
The Frick test is performed by applying an external rotation to the foot and ankle with the knee flexed 90°[53].The ankle is dorsiflexed, and the external rotation of the foot replicates the mechanism of the injury.Pain indicates a positive test[54].
In the Cotton test, medial and lateral forces are applied to the talus; the increased pain in medial-lateral plane translation indicates a positive test result[55].
Finally, in the crossed-leg test the patient is in a sitting position, and the mid fibula of the injured leg is placed on the knee of the healthy leg.The knee is then pushed on the injured leg toward the ground; syndesmosis pain demonstrates a positive result[54].
Unfortunately, none of these examinations are directive in the diagnosis, especially if a fracture is present, because induced pain can limit its development.For this reason, the diagnosis should not only be made based on medical history and physical examination but in conjunction with imaging (also helpful for the preoperative planning) and intraoperative evaluation[55].
Generally, anteroposterior (AP), laterolateral and mortise views are used during radiographic examination.The AP view is useful for evaluating the distal epiphyseal portion of the fibula and tibia.The mortise projection is a variant of the AP projection (obtained with the internal rotation of the foot by 10-15°).The lateral view allows a good evaluation of the posterior tibial tuberosity (Figure 3).Three radiographic parameters have been established to evaluate diastasis of the distal tibiofibular joint: tibiofibular clear space (TFCS)[56,57], tibiofibular overlap (TFO)[56,57] and medial clear space (MCS)[58] (Figure 4).
The TFCS is the distance between the lateral border of the posterior tibial malleolus and the medial edge of the distal epiphysis of the fibula, measured about 10 mm above the tibial plafond in both the AP projection and in the mortise view.Most authors believe that TFCS is the most reliable parameter to suspect a syndesmotic lesion and consider a TFCS greater than 6 mm as pathological[51,59].Schoennagelet al[60] have shown that by setting a TFCS cut-off of 5.3 mm and considering values greater than 5.3 mm as indicative of syndesmotic lesions and values lower than 5.3 mm as not indicative of such lesions, is possible to have a diagnostic accuracy with a specificity and sensitivity of 75% and 82%, respectively.
The TFO is the distance between the lateral edge of the anterior tibial tubercle and the medial edge of the distal epiphysis of the fibula.In normal conditions it should be > 6 mm in the AP projection and > 1 mm in the mortise view.It has been demonstrated that the TFO value has a high degree of variability depending on the rotation of the foot at the time of the X-ray acquisition and that the only parameter that does not vary, according to the rotation of the foot, is the TFCS[51,61].

Figure 3 X-ray of the right ankle: standard projections.

Figure 4 Normal values of tibiofibular clear space, tibiofibular overlap and medial clear space in left ankle mortise projection.
The MCS, measured in the projection of the mortise, is the widest distance between the lateral edge of the medial tibial malleolus and the medial edge of the talus.In normal conditions the MCS should be equal to or less than the space between the tibial plafond and the talar dome[51].Like the TFO, the value of the MCS varies depending on the rotation of the foot at the time of acquisition of the radiograph[61].Schoennagelet al[60] demonstrated that using the distance of 2.8 mm as a cut-off is possible to discriminate between patients with syndesmotic lesions and patients without syndesmotic lesions with a specificity and sensitivity of 59% and 73%, respectively, and if both TCFS and MCS values were altered, the specificity increased to 86%.Grathet al[62] affirmed that it may also be useful to compare the MCS of the affected side with the contralateral and that differences greater than 2 mm may be indicative of syndesmotic lesions.
However, due to the interobserver variation, wide anatomic variability in the depth of the peroneal groove and the shape of the tibial tubercles, these measurements are not reliable unless there is significant disruption of the DTS[1].If the measurements obtained by radiography are ambiguous, bilateral CT can be useful (Figure 5).Horizontal slices allow measurement of the intertibiofibular gap.With a threshold of 4 mm, the anterior gap (selectivity, 56.5%; specificity, 91.7%) and medial gap (selectivity, 74.4%; specificity, 78.4%) are reproducible measurements, unlike the posterior gap.AP translation of the fibula and rotation with respect to the tibia, TFCS and TFO can also be assessed, and peroneal groove anatomy can be evaluated[51].
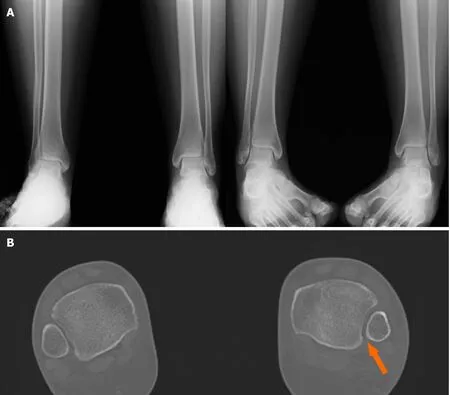
Figure 5 Suspect of a left syndesmotic lesion.
In those cases of DTS injuries associated with fractures, preoperative CT should be useful to better study the morphology of the fracture, determine the correct size and shape of the PM fracture, which will determine if the associated plan is the correct surgical procedure[63,64].In addition, comparative CT can be used in the postoperative evaluation of the correctness of the reduction of the diastasis (Figure 6).The current trend is in favor of stress X-rays and stress CT (external rotation and dorsiflexion) or CT in weight-bearing[51], especially in the detection of chronic disruptions.Magnetic resonance imaging has added benefit to assess the soft tissue condition directly, but it has been found to be useful in both acute and chronic isolated syndesmotic injuries[1,65,66].
Furthermore, the modified Cotton test is largely used during surgery, and it consists in laterally fibula distraction with the use of a bone hook or reduction clamp (Figure 7).An intraoperative fluoroscopic mortise view of the ankle that shows a widening more than 2 mm in the syndesmosis suggests an unstable injury that necessitates fixation[67].Another intraoperative specific test for the deltoid lesion is the external rotational stress test that is performed after lateral fibular fixation.If there is a talar tilting leading to MCS more than or equal to 5 mm, then the test should be considered positive[68].
Finally, ankle arthroscopy also enables diagnosis of syndesmosis instability, and it can be used as a diagnostic and therapeutic tool[51].The syndesmosis is judged unstable as of 2 mm diastasis, which is commonly tested by introducing an arthroscopic palpation hook into the tibiofibular joint line[58,59].If fixation is indicated, then arthroscopy may guide extra-articular stabilization[51].

Figure 6 Postoperative computed tomography scans of a syndesmotic lesion showing a widened tibiofibular space (arrows) indicative of an inadequate reduction.

Figure 7 Intraoperative view.
SURGICAL TREATMENT AND POSTOPERATIVE CARE
All injuries with evident diastasis require surgical stabilization[69,70].The goal of treatment is to restore joint congruency and to maintain the stability of the syndesmosis until the ligaments have healed.The ideal implant should stabilize the joint but also allow its physiological movements and that of the ankle, thus guaranteeing an early mobilization.
Surgery initially involves stabilization and restoration of the fibular length, followed by the fixation of the PM and finally of the tibia.The indications for fixation of the PM remain controversial.Historically, these included fractures involving > 25% to 33% of the joint surface, displacement > 2 mm, ankle instability in association to syndesmotic lesion and persistent posterior subluxation of the talus[71,72].
However, up to now, there has not been any strong clinical evidence for this practice, and the percentage of articular surface of PM has been questioned, as studies have demonstrated the importance of even small posterior malleolar fragments to ankle stability, and surgical indications have expanded.The historic criteria based on size could underestimate the number of fractures that requires operative intervention[73].
In a prospective study of outcomes of syndesmotic injuries with posterior malleolar fractures, Milleret al[74] found that posterior malleolar fixation was equivalent to fixation with syndesmotic screws or combined fixation.The results of these studies would lead to the conclusion that even small posterior malleolar fractures should be repaired in ankle fractures with syndesmotic disruption.Anatomic reduction of the PM additionally recreates the incisura fibularis, the congruity of the articular tibial surface and should minimize the risk of posterior translatory malreduction of the syndesmosis as the PITFL is intact.
Warneret al[75] went so far as to say ligamentous repair of the PITFL is critical in ankle fractures.They studied PITFL injuries in the absence of the PM fracture and found that most lesions occur as a delamination of the ligament from its attachment to the PM.In conclusion, they suggested that repair techniques to fix the PITFL to its footprint on the PM may provide an effective stabilization of the syndesmosis and that this approach could potentially obviate the need for further DTS stabilization.
Different surgical approaches and techniques for internal fixation of PM fractures [percutaneous anterior to posterior screw fixation or open reduction and internal fixation using screws or buttress plates from posterior to anterior] have been reported[76].Indirect reduction and stabilization with AP screws remain the early common method[76,77].The disadvantages of this type of fixation of the PM are that anatomical reduction is more difficult due to the interposition of soft tissues or loose bony fragments, which is hard to assess reduction satisfactorily using an image intensifier, and the fixation of small or comminuted fragments is technically difficult.Furthermore, symptomatic tibial nerve entrapment syndrome has been described[78].
For this reason, several surgeons prefer open and anatomical reduction.The choice of the surgical approach must be guided by the characteristics of the ankle’s fracture thus including the PM.Precise classifications of PM fractures, based on CT examination, are undoubtedly helpful as different studies have shown inadequacy of radiographs in assessing the shape and the size of the PM detached but also the real involvement of the fibular notch and of the medial malleolus[63,79,80].In this context the most utilized classification systems are from Haraguchi[64], who conducted a CT study to clarify the pathologic anatomy of the PM fractures, and from Bartoníček[63].
The posterolateral approach has been described in the literature and has received much attention.Surgery is usually performed in the prone position.Most surgeons prefer an incision between the peroneal and Achilles tendons, but others did perform the incision just medial to the posterior border of the fibula[81].This approach allows a direct visualization and reduction of the posterior fragment, even if addressing the posteromedial malleolar fracture is more difficult.In this case an incision immediately laterally to the Achilles tendon can facilitate fixation of the more medial part of the PM fracture.On the other hand, posterolateral approach has the potential to cause sural nerve injuries and that prone position may render open reduction and internal fixation of the medial malleolus more challenging[76].
Another possible approach is the posteromedial, which allows fixation of the medial and PM through the same incision, even if for a typical posterolateral fragment it would seem suboptimal[82].
In types II and IV fractures according to Bartoníček, which correspond to type I of Haraguchi’s classification, a posterolateral approach with mobilization of the peroneal tendon is used almost exclusively.For fixation of type III lesions, which corresponds to type II of Haraguchi’s classification, a posteromedial approach is preferred.In selected cases, in which the reduction of both posterior fragments is not possible, a combined posteromedial and posterolateral approach have been utilized[83,84].
Definitive osteosynthesis of PM fragments depends on the number and size of the fragments and on quality of the bone.Later, the surgeon must decide the necessity of an additional syndesmotic fixation.This choice depends on DTS stability and must be evaluated manually and fluoroscopically during surgery[21].Various stabilization modalities of DTS have been used[2].They can be divided by SF techniques (metallic or bioabsorbable screws, staples, syndesmosis hooks, Kirschner wires) and DF techniques (suture-button)[2,16-18].
SF with cortical screws is the reference standard fixation method.However, some significant issues should be considered.Screw loosening, breakage (Figures 8 and 9), discomfort, pain related to overcompression, the need for a reoperation for screw removal and the risk of late diastasis after early removal are potential drawbacks of this type of fixation[20-24].Syndesmotic screw is the oldest surgical device utilized, and it was first described by Burwellet al[70] in 1965.In the literature there is a wide debate about the type, size and number of screws to be placed, the optimal distance from the tibial plafond, the optimal number of cortices to cross, the position of the foot during fixation, the timing and real need for screw removal.

Figure 8 Type B ankle fracture.
The screw that is more frequently used is metallic.As mentioned, it stabilizes the joint allowing the injured ligaments to heal.However, this fixation does not completely permit the physiological reciprocal movement between the fibula and tibia.It often requires removal, with the associated increased risk of complications (infections and recurrence of diastasis) and higher costs.For these reasons, bioabsorbable devices have been developed, first produced in polyglycolic acid, subsequently in polylactic acid and currently in polylevolactic acid.These devices gradually reabsorb by hydrolysis, thus allowing a progressive recovery of the syndesmosis function[85].The bioabsorbable screw has shown the same efficacy in maintaining stability, and the incidence of rupture and infection is similar to that of the metal one.The reoperation rate is lower, and in about 13% of cases there is a foreign body reaction that can last for months.In some cases, it can lead to a second intervention[86,87].

Figure 9 Type C ankle fracture and dislocation.
One or two 3.5 mm or 4.5 mm diameter screws can be used, and there are no statistically significant differences in short and long-term outcomes and functionality between these two diameters.Biomechanical studies have shown that the breaking load is higher in 4.5 mm screws and that the presence of two screws ensures greater biomechanical stability.Nevertheless, these differences have no clinical significance because it has been demonstrated that the single 3.5 mm diameter screw is able to maintain adequate stabilityin vivo[88,89].
Tricortical and quadricortical screws have been compared in terms of stability and outcomes.Tricortical fixation is a less rigid system for stabilizing a syndesmosis, and it recreates a more similar syndesmosis biomechanism with less breakage risk.However, quadricortical fixation, with one or two screws, is characterized by less occurrence of syndesmotic widening during the healing period, although it is more rigid.In any case, fixation after reduction should be performed 2-4 cm above and parallel to the joint line and perpendicular to the distal tibiofibular, from posterior to anterior through the fibula and tibia with an inclination of 25°-30°[90,91].
The influence on the short and long-term outcomes of the foot position to be maintained during fixation is still unclear.Olerudet al[92] suggested placement of the syndesmotic screw with the foot in dorsiflexion to avoid limitations of this movement.Other authors instead have recently demonstrated that the most important aspect of fixation is anatomic reduction of the syndesmosis, and dorsiflexion during fixation has less importance.They concluded that foot position does not influence long-term outcomes[93].However, the possibility of excessive compression and, consequently of a limitation of dorsiflexion, is described, but it is observed when the screw is tightened too hard, or it is attributable to the excessive force applied with the reduction clamp at the time of positioning the screw, which does not depend on the foot position[94].
The optimal force that should be applied with a clamp to reduce the syndesmosis is currently unknown.Fluoroscopy is typically used for intraoperative assessment of the reduction of the syndesmosis.However, the use of other intraoperative imaging studies have been evaluated (intraoperative CT).Obtaining intraoperative mortise and perfect lateral fluoroscopic views of the talar dome of both ankle before fixation could help in determining the relationship between the fibula and tibia in the ankle and to reduce the risk of overcompression[93].
The real need for the removal of the intersyndesmotic screw is a topic that has been the subject of debate for years.The authors that suggest to always remove the screw maintain that otherwise the biomechanics of the ankle joint and its dorsiflexion could be hindered, and the load could therefore lead to the breaking or mobilization of the screw[95].Other authors instead have shown that patients with retained or broken devices do not show significant differences in terms of outcomes and complications compared to those with intact ones[96].Furthermore, their removal, especially in patients who present a delayed healing of the surgical wound following the first operation, is subject to a higher rate of infection.For these reasons, the percentage of patients in which the screw has not been removed has passed from 8% in 2004, to 14% in 2008, to over 35% in 2010[97], and as a consequence the routine screw removal is not recommended now.However, this procedure may be indicated in cases of intolerance, poor joint reduction and when it is indicated to remove the synthesis hardware of the associated malleolar fracture[98].In these cases, extraction should be scheduled no earlier than 8 wk (preferably 10-12 wk) as it has been amply demonstrated that removal within the first 8 wk is burdened by a higher incidence of loss of reduction and recurrence of diastasis[99].
In any case, one of the main problems in screw maintenance cases is the management of the patient in the postoperative period.In many cases, the patient struggles to accept the idea of being able to weight bear on a retained screw, and similarly he/she does not accept the idea of maintaining a screw that is broken (although this does not involve any risk)[100].Consequently, if the surgeon decides to maintain the screw, it is therefore necessary to adequately explain to the patient the risk of rupture of the screw and that any breakage does not lead to more complications.
To overcome the excessive joint stiffness and the increased stress on the interosseous membrane that a static stabilizer causes, an alternative system of dynamic stabilization with an implanted suture-button device has been developed.It consists of a nonabsorbable synthetic suture between two metallic buttons implanted across the DTS[4,25], and it is characterized by less risk of hardware pain and recurrent syndesmotic diastasis, quicker return to mobility, maintenance of physiologic movement while retaining reduction, earlier rehabilitation and no need for removal[101,102].It has also been shown that the position of the foot at the time of implant fixation does not affect stability, postoperative range of motion and outcomes[103].Several literature reviews and meta-analyses confirmed these significant clinical advantages, but sometimes a greater residual diastasis is described.Instead, syndesmosis screws provide more rigid assembly but a higher rate of poor reduction (12%-39%), ablation (40%-50%), breakage (up to 30%) and more local discomfort[104].Nevertheless, there is no agreement on whether DF methods are superior to SF methods in terms of long-term functional outcomes, change in range of motion, complication rates and incidence of reoperation[26,27,105].
Equally important is the postoperative treatment.To prevent the equinus of the foot, the ankle is kept at rest with the foot at 90° by means of a plaster splint applied posteriorly.The patient is encouraged to move the toes early.If the wounds are satisfactory, then passive and active mobilization of the ankle under the control of the therapist can begin after 24-48 h.Once active dorsiflexion is achieved, the decision to leave the ankle free or to keep it still with the plaster cast depends on various factors, such as the stability of the internal fixation obtained by the surgeon, the patient's general mobility and the prospects for adhesion to the chosen postoperative regimen.It has been shown that long-term results are similar with both the immobilized and the free ankle, during the first 6 wk after surgery[106].Loading decisions, with or without plaster, also largely depend on the stability of the fixation obtained and the patient’s cooperation.Most authors recommend avoiding weight-bearing for 8-10 wk whether the screw is removed or left in place[15].
AUTHORS PREFERRED SURGICAL METHOD
Patients are positioned with a tourniquet applied, and the surgical procedure is done under fluoroscopic control.In the cases of trimalleolar fractures, we initially stabilize and restore the fibula length and consequently synthesize the PM and finally the tibia.We prefer open reduction of posterior malleolar fragment through a posterolateral approach in types II and IV and a posteromedial approach in type III fractures according to Bartoníček classification.In selected cases, when reduction and fixation of both posterior fragments is difficult to achieve, we have opted for a combined posteromedial and posterolateral approach (Figure 10).
The choice of the fixation devices (screws or plates) depends on the intraoperative characteristics of the fractures and the quality of the bone.The decision to stabilize the DTS depends on the positivity of the modified Cotton test.We prefer the use of reduction clamp instead of bone hook because of its minor aggressiveness towards the soft tissues between tibia and fibula.
We obtain DTS fixation with one tricortical 3.5 mm screw that is positioned approximately 2.5-3.0 cm proximal and parallel to the tibiotalar joint with the foot in dorsiflexion at 90° (Figure 11).
In most cases the simple screwing determines the closure of the DTS.If this does not happen, then we first try to reduce the diastasis with forceps before placing the screw.If despite this maneuver the DTS reduction is not sufficient, then we perform a medial surgical exploration to verify if the deltoid ligament is detected between the malleolus and the talus.
In the immediate postoperative period, a plaster cast with the foot at 90° is applied for 48 h.After this period, if the stability of the fixation obtained is good, the wound healing is positive and the patient is collaborative, then the cast can be replaced by a removable bivalve ankle brace with the aim to begin early active and passive progressive mobilization under the control of the therapist.We recommend avoiding weight-bearing for 8-10 wk whether the screw is removed or left in place.
Until 5 years ago, the authors always removed the screw after 8-10 wk from surgery.Based on recent findings in the literature, they currently rarely remove this device.The patient is informed regarding the possibility of screw rupture and that this occurrence does not compromise the long-term functional result.
Intolerance, pain, poor reduction obtained and necessity to remove malleolar fracture hardware does lead us to consider this second surgery.Screw removal is then performed under local anesthesia and fluoroscopic control.Antibiotic prophylaxis with first generation cephalosporin (cefazoline) is always administered.
CONCLUSION
The stability and correct anatomy of the DTS is essential for normal biomechanics of the ankle.Syndesmosis injuries occur following spraining trauma especially in external rotation, and they can be isolated or, more frequently, associated with malleolar fractures.In the latter case, specific clinical tests for the evaluation of syndesmosis are not reliable due to the important painful symptoms of the fracture.Consequently, preoperative imaging and specific intraoperative tests, performed after completing the synthesis of the associated malleolar fractures, are essential for the definitive diagnosis and indication for stabilization of the DTS.In this context, the Danis-Weber radiological classification and the modified Cotton test are the most used and complete.
Furthermore, especially if the images obtained by radiography are not conclusive, preoperative CT is mandatory in order to better evaluate the size, shape and location of fracture fragments and to assess the stability of the tibiotalar joint through more precise measurements and the integrity of the fibular notch[63,74,76,107].In those cases where after fracture stabilization the DTS remains unstable, the different treatment options include SF and DF techniques.To this day, the intersyndesmosis screw remains the most widely used method of stabilization.
Despite the numerous anatomical, biomechanical and comparative studies performed, there is still a wide debate as to which surgical technique is the best.From the analysis of the literature, it emerged that the type, size and number of screws, the number of cortices to cross, the distance from the tibial plafond and the position of the foot during fixation do not significantly affect the short and long-term results.

Figure 10 Trimalleolar right ankle fracture associated with dislocation.
It will be a choice of the surgeon in accordance with the patient whether to remove or maintain the screw.The removal is indicated in those cases characterized by intolerance, pain, malreduction or if it is necessary to remove the hardware implanted for associated malleolar fractures.In this regard, it is important to emphasize that screw rupture does not negatively influence the clinical results.If removal is performed, then it must be scheduled after at least 8 wk to avoid the risk of recurrence of the diastasis.However, it is well established that in this type of fixation the possibility of screw loosening, breakage, discomfort, the need for a reoperation for screw removal and the risk of late diastasis after early removal should be considered.

Figure 11 Type C ankle fracture.
These drawbacks seem to be canceled by dynamic fixation with the endobutton, which has become increasingly popular as it allows a more physiological articular movement, early rehabilitation, satisfactory functional outcomes and no requirement for implant removal.Nevertheless, there is no unique consensus on whether DF methods are superior to the static ones.
Another frequent complication of DTS stabilization associated with fractures is malreduction.This is the consequence of an inadequate closure of the malleolar forceps, of an abnormal anteriorization or posteriorization of the fibula with respect to the tibia or of a rotational fibular malalignment.For this reason, if the simple screwing does not close the DTS, then the authors suggest trying to reduce the diastasis with forceps before placing the screw, considering that an excessive tension of the forceps can favor the anterior translation of the fibula.If despite this maneuver the DTS reduction is not sufficient, then they perform a medial surgical exploration to verify if the deltoid ligament is detected between the malleolus and the talus.In doubtful cases, a bilateral postoperative CT is helpful for evaluating the correct reduction.
In addition to malreduction, the development of heterotopic ossification and more rarely tibiofibular synostosis is reported.Functional consequences of these complications are questionable and often no special treatments are needed due to real symptoms[108].Alternatively, in rarer cases persistent pain related to heterotopic ossification and synostosis required surgical treatment[67].
Finally, the authors are confident that postoperative care is another important aspect for positive outcomes.They agree with most authors that loading is not recommended until the screw is removed, or if it is not removed, then for 8-10 wk after surgery, depending on the stability of the synthesis obtained and the patient’s characteristics.Active and passive exercises of the ankle are allowed immediately after surgery.
In conclusion, patients with unstable injuries require surgical stabilization [15,95,105,109].The aim of surgical treatment is to restore joint congruency and to maintain the stability of the syndesmosis until the ligaments have healed.Satisfactory results depend on a correct management from diagnosis to treatment.SF and DF systems have similar long-term clinical and radiological outcomes.
杂志排行
World Journal of Orthopedics的其它文章
- Fibula fractures management
- Reducing unnecessary crossmatching for hip fracture patients by accounting for preoperative hemoglobin concentration
- Usefulness of computed tomography based three-dimensional reconstructions to assess the critical shoulder angle
- Potential contribution of pedicle screw design to loosening rate in patients with degenerative diseases of the lumbar spine: An observational study
- Endoscopic fasciotomy for chronic exertional compartment syndrome of the forearm: Systematic review of outcomes and complications
- Rare shear-type fracture of the talar head in a thirteen-year-old child— Is this a transitional fracture: A case report and review of the literature
