Current status and challenges in sentinel node navigation surgery for early gastric cancer
2021-05-19SatoruMatsudaTomoyukiIrinoHirofumiKawakuboHiroyaTakeuchiYukoKitagawa
Satoru Matsuda,Tomoyuki Irino,Hirofumi Kawakubo,Hiroya Takeuchi,Yuko Kitagawa
1Department of Surgery,Keio University School of Medicine,Tokyo 160-8582,Japan;2Department of Surgery,Hamamatsu University School of Medicine,Shizuoka 431-3192,Japan
Abstract As an optimal surgical procedure to accurately evaluate lymph node (LN) metastasis during surgery with minimal surgical resection,we have been developing sentinel node (SN) biopsy for early gastric cancer since the 1990s.Twelve institutions from the Japanese Society of Sentinel Node Navigation Surgery (SNNS),including Keio University Hospital,conducted a multicenter prospective trial to validate the SN concept using the dual-tracer method with blue dye and a radioisotope.According to the results,397 patients were included in the final analysis,and the overall accuracy in detecting LN metastasis using SN biopsy was 99% (383 of 387).Based on the validation study,we are targeting cT1N0 with a primary tumor of ≤4 cm in diameter as an indication for SN biopsy for gastric cancer.We are currently running a multicenter nonrandomized phase III trial to assess the safety and efficacy of SN navigation surgery.The Korean group has reported the result of a multicenter randomized phase III trial.Since meticulous gastric cancer in the remnant stomach was rescued by subsequent gastrectomy,the disease-specific survival was comparable between the two techniques,implying that SN navigation surgery can be an alternative to standard gastrectomy.With the development of SN biopsy procedure and treatment modalities,the application of SN biopsy will be expanded to achieve an individualized minimally invasive surgery.
Keywords:Sentinel node;gastric cancer;minimally invasive surgery
Introduction
Gastrectomy with an adequate range of lymph node (LN)dissection has remained a standard surgical procedure for gastric cancer.The Japan Gastric Cancer Association published gastric cancer guidelines that defined standard gastrectomy and the range of LN dissection (1).In the European Society for Medical Oncology Clinical Practice Guidelines,in Western countries,patients who are medically fit should undergo D2 dissection,while it should be carried out in specialized,high-volume centers (2).To date,although pylorus-preserving and proximal gastrectomy can be alternatives for cT1N0 gastric cancer,the standard surgical procedure has been either total or distal gastrectomy.According to the results,the exact number of patients encountered post-gastrectomy syndrome,including dumping syndrome,loss of body weight,resulting in a decreased quality of the remaining life.Although minimizing the field of lymphadenectomy might decrease the incidence of post-gastrectomy syndrome and improve postoperative patients’ quality of life,since curability is a top priority in cancer surgery,the indication of limited gastrectomy should be carefully evaluated.To appropriately modify the surgical procedure,a pre-or intra-operative diagnosis of LN metastasis is required.
As an optimal surgical procedure to accurately evaluate LN metastasis during surgery with minimal surgical resection,we have been developing sentinel node (SN)biopsy for early gastric cancer since the 1990s (3-5).In this review,we updated the concepts and technique of SN biopsy and report the current phase III trials.
Development of SN biopsy in cancer surgery
LN,one of the secondary lymphoid organs,develops in early embryogenesis (6).Once formed,the number of LNs is conserved,while the intra-nodal constitutions and lymphatic networks can be altered in response to an external stimulus,such as inflammation and infection (7).In the development of cancer,LN can be the first metastatic site.Therefore,once the presence of LN metastasis is accurately detected,the indication,and range of lymphadenectomy can be precisely modified for each patient.SN is a 1st drainage LN and primarily receives tumor cells.Historically,Cabanas proposed SN concept for penile cancer (8),and Morton subsequently reported the clinical study in malignant melanoma (9). With development in breast cancer field,the SN concept has been widely accepted and used in determining whether patients require extensive lymphadenectomy.
Navigation surgery based on SN biopsy for early gastric cancer:History and current status
SN concept and basin theory
To accurately diagnose whether a patient has LN metastasis during surgery and develop individualized surgical treatment for early gastric cancer,we started SN mapping in the 1990s (5,10-12).For combining the radioisotope and blue dye,the dual-tracer method was proposed,and the distribution of SNs was evaluated.Different from malignant melanoma and breast cancer,the lymphatic drainage route from gastric cancer is highly variable.In fact,Leeet al.reviewed 462 pT1 or T2 gastric cancer patients and revealed that there was skip metastasis,having suggested the difficulty in predicting the drainage LNs based on the location of primary tumors (13).Therefore,the pre-or intra-operative detection and evaluation of drainage LNs are critical.To classify the lymphatic route,Kinamiet al.defined five independent lymphatic basins for each feeding artery surrounding the stomach (14).Later on,the efficacy of SN biopsy was investigated based on the lymphatic basins.In other words,even though LN metastasis was detected in non-SN,as long as non-SN with metastasis is included in the same lymphatic basin as SN,LN metastasis can be eradicated in the SN biopsy.Therefore,whether or not metastasic non-SN was included in the same lymphatic basin as SN was a critical aspect in the following studies.Niiharaet al.reviewed 385 patients diagnosed with cT1N0 or cT2N0 gastric cancer and confirmed that the SN concept was secured in cT1 with a tumor diameter of 4 cm or shorter(15).On the other hand,as reported,the lymphatic route was highly variable,as Shimadaet al.reported that the common hepatic artery LN had lymphatic flow not only from the right gastric artery basin but also from the left gastric artery basin or the right gastroepiploic artery basin(16).In patients with middle-third location of cT1N0 gastric cancer,13% of patients had SN in supra-or infrapyloric LNs (17).Subsequent analysis from other groups also reported that tumor location and tumor diameter need to be considered to predict the direction of the lymphatic route (18).In summary,the location of a lymphatic basin can be hardly predicted using preoperative factors,and it is crucial to develop a reliable procedure to detect SN during surgery,which will help to select an appropriate surgical procedure for each patient.
Development and update of procedures detecting SN and diagnostic test of metastasis in SN
As a sensitive method of detecting SN during surgery,we have been developing the dual-tracer method,in which a radioisotope and blue dye are combined (19,20).The day before surgery,a solution of technetium-99m tin colloid is injected in four quadrants of the submucosal layer surrounding the primary cancer lesion using an endoscopic puncture needle.Of various radioactive tracers commonly available,such as Tin,phytic acid,and sulfur nanocolloid,Tin colloid has been preferencially used because of its large particle size,that helps tracers to be retained within the SN for a longer time and potentially lower the false-negative rate (11,21).In the current procedure,indocyanine green(ICG) or isosulfan blue has been used as a blue dye,which is injected through intraoperative endoscopy using the same method used for injection of radioactive colloid.For detecting SNs,a gamma probe was used.In addition to the expected higher sensitivity,the other advantage of using radioisotope was its potential as an auxiliary diagnosis.Kamiyaet al.reported that a high radioisotope count from an SN was correlated with LN metastasis,and radioisotope counting might aid efficient pathological diagnosis (22).In terms of a blue dye,isosulfan blue was initially used.However,as ICG fluorescent tracer was widely accepted,ICG was adapted as an alternative.As reported in the radioisotope,the fluorescence intensity obtained from ICG was associated with metastasis (23).Although there are comparative studies between isosulfan blue and ICG in other malignancies (24),there is no concrete standard for blue dye in gastric cancer at this point in time.While ICG was reported to be more sensitive than isosulfan blue,surgeons need to be aware that ICG potentially visualizes lymphatic trunk or second-and third-echelon nodes.Further validation studies along with the new technology to improve the sensitivity and specificity to detect SN during surgery are desired.As a new method,a fluorescent dye detected under the light-emitting diode curing light was also reported to be feasible for visualizing SN.Given that SN can be detected by visible light,we can visualize SNs and their surrounding structures that might improve safety of the procedure (25).
Detecting SN before surgery would guide the type of gastrectomy preoperatively and will be valuable for patients to select the treatment strategy.Computed tomography(CT) lymphography using peritumoral lipiodol injection was tested (26).Although the detection rate was almost identical between preoperative CT lymphography and intraoperative dual-tracer method,the concordance rate was 87%,indicating that there was a discrepancy in the distribution of SN basin.Therefore,the authors recommended the complemental application of CT lymphography.With regard to the utility of lymphoscintigraphy,we have previously demonstrated its insufficient detection rate of sentinel lymphatic basins before gastrectomy (27).Therefore,the preoperative lymphoscintigraphy is still immature SN mapping in early gastric cancer.
Along with SN detection,an accurate and prompt intraoperative diagnosis of LN metastasis is required.Although intraoperative immediate pathologic assessment should be the gold standard,micrometastasis can be ignored because one section is generally examined for each node.As a more reliable procedure,the clinical significance of real-time polymerase chain reaction (28,29) and one-step nucleic acid amplification (30-33) were suggested.Those methods targeted specific markers such as cytokeratin (CK)19,CK20,and carcinoembryonic antigen that were unique to gastric cancer.However,we cannot ignore the drawback of molecular detection that might lead to false positives,and the heterogeneity of tumor cells might lose typical makers that were targeted in the assay.
Validation studies of SN biopsy for early-stage gastric cancer
To validate the SN concept and dual-tracer method,12 institutions from the Japanese Society of Sentinel Node Navigation Surgery (SNNS),including Keio University Hospital,conducted a multicenter prospective trial.Gastric cancer patients who were diagnosed as cT1N0 or cT2N0 with single primary lesions (≤4 cm) were included.In terms of the SN detection,the dual-tracer method using technetium 99m-labeled tin colloid and 1% isosulfan blue dye were used.The primary endpoint of the study was the sensitivity in detecting metastasis on the basis of SN status.According to the results,of the 397 patients included in the final analysis,SN was detected in 387 (97.5%).LN metastasis was observed in 57 patients.Based on the fact that 4 out of the 57 did not show LN metastasis at SNs,the overall accuracy in detecting LN metastasis using SN biopsy was 99% (383 of 387).In terms of the four patients who experienced false negatives,three were either pT2 or with a primary tumor of >4 cm in diameter.There were no severe adverse events associated with SN biopsy (34).Based on the validation study,we are targeting cT1N0 with a primary tumor of ≤4 cm in diameter as an indication for SN biopsy for gastric cancer.On the other hand,given that preoperative diagnosis remains unsatisfactory (35),the overall safety and efficacy of navigation surgery based on SN biopsy need to be evaluated in the prospective interventional trial where the type of gastrectomy is also modified following SN biopsy.
While the SN concept was successfully validated,we need to recognize the result that the JCOG0302 study,where the utility of SN biopsy for early gastric cancer was tested,reported a relatively high false-negative rate and sent an alert that SN biopsy with histological evaluation of one plane might not be adequate.Although there were several limitations that the single-tracer method using ICG was used and basin resection was not conducted,which might have led to lower sensitivity,this study suggested that the efficacy of SN biopsy might differ,depending on the procedure and learning curve that seemed to be vital (36).
Current trial progress in SN navigation surgery
The ultimate goal of SN biopsy for early gastric cancer is to develop SN-based navigation surgery as an individualized minimally invasive surgery for gastric cancer.We are currently running a multicenter nonrandomized phase III trial (37) (Figure 1).Based on our previous multicenter study (34),previously non-treated gastric cancer in patients diagnosed as T1N0 with a single lesion(≤40 mm) is a major inclusion criterion.SNs are identified by dual-tracers and are subjected to immediate intraoperative pathological assessment. For patients with negative SN metastasis,individualized surgery consisting of local stomach resection and SN basin dissection is performed.A total of 225 patients will be accrued from 13 hospitals from SNNS that have experience in SN mapping.The primary endpoint is the 5-year relapse-free survival.As one of the secondary endpoints,patient-reported outcomes are to be collected and will be used to assess the utility of SN navigation surgery.
The Korean group designed a multicenter randomized phase III trial to investigate the efficacy of SN navigation surgery for gastric cancer (the SENORITA trial) (38).The major inclusion criterion was a cT1N0M0 gastric adenocarcinoma,with a diameter of 3 cm or less.A total of 290 patients per group were randomized to either laparoscopic stomach-preserving surgery with SN biopsy or standard surgery.The primary endpoint was 3-year disease-free survival (DFS).Overall,527 patients underwent surgery.In the SN navigation surgery group,an SN basin was detected in 97% of patients.In terms of the type of gastrectomy,stomach-preserving surgery that comprised endoscopic submucosal dissection (ESD),endoscopic full-thickness resection,laparoscopic wedge resection,or laparoscopic segmental resection was carried out in 81% of patients in the SN navigation surgery group.There was no significant difference in the rate of postoperative complications between the groups (39).A primary survival analysis was reported in 2020,showing that 3-year DFS was 95.5% in the standard gastrectomy group and 91.8% in the SN navigation surgery group[hazard ratio (HR)=1.901,95% confidence interval (95%CI),0.911-3.967].However,since meticulous gastric cancer in the remnant stomach was rescued by gastrectomy,the 3-year disease-specific survival was comparable,implying that SN navigation surgery could be an alternative to standard gastrectomy (40).
When comparing these two pivotal studies,we need to be aware that the definition of the lymphatic basin,which refers to“to what extent lymphatics flows from the primary tumor”,might not be identical.In the Korean trial,the lymphatic basin that should be dissected refers to a limited area comprising of SNs,whereas in the Japanese trial,the lymphatic basin was defined as five distinct lymphatic areas based on their location along the five main arteries to the stomach (14).Therefore,careful consideration would be necessary when interpreting the result of the two studies.
Fused surgical procedure using local stomach resection and SN biopsies
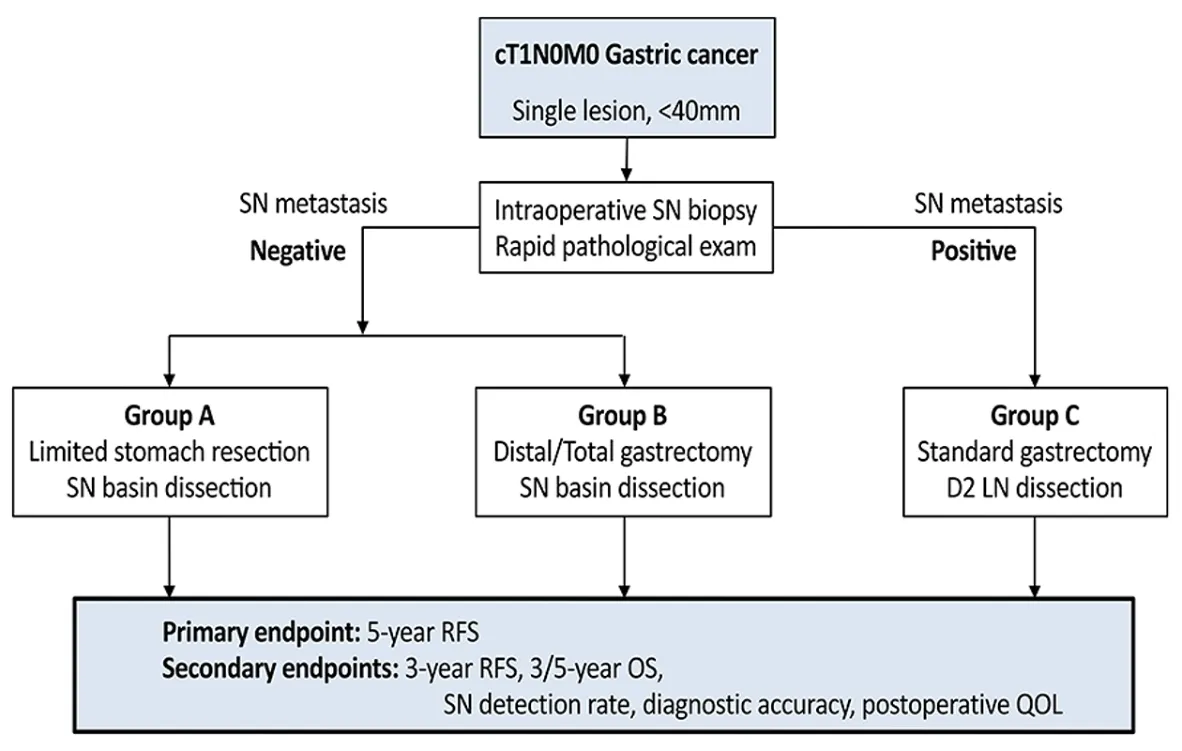
Figure 1 A multicenter non-randomized phase III trial from the Japanese Society of Sentinel Node Navigation Surgery (Reproduced with permission from Ref.37,Oxford University Press).SN,sentinel node;RFS,relapse-free survival;OS,overall survival;QOL,quality of life.
Given that local resection for gastric cancer could be safely performed with the help of SN biopsy,various patterns of local resection can be considered.In fact,Aoyamaet al.investigated the probabilities of local resection with SN biopsy.They revealed that 53% of all the study participants were considered eligible for local resection based on the distribution of SNs,particularly those with tumors in the upper third of the stomach (41).There is another retrospective study showing the potential of local resection and SN basin resection in proximal gastric cancer (42).When local resection is indicated in gastric cancer,fullthickness resection without exposing tumor cells to the abdominal cavity is required.Furthermore,the resection margin needs to be carefully evaluated to achieve a curative resection with minimal size.As a novel surgical procedure for full-thickness resection,full-layer resection for gastric cancer with the non-exposure technique (CLEAN-NET)was reported in 2012 (43).CLEAN-NET was beneficial since the stomach wall was not perforated with resection and achieved local resection.Combining local resection with SN biopsy,the post-gastrectomy symptoms were reported to be improved (44).Combining local resection using laparoscopy and endoscopic submucosal dissection,non-exposed endoscopic wall-inversion surgery (NEWS)was developed by Gotoet al(45).In NEWS,after marking the primary lesion,circumferential sero-muscular incisions were made and sero-muscular continuous suturing was performed,with the lesion inverted toward the inside of the stomach.Finally,a circumferential mucosal incision was made with the endoscopic submucosal dissection technique,and the lesion,as well as the sheet,was transorally retrieved.The combined procedure with SN biopsy was already reported for gastric cancer (46,47).As a minimally invasive procedure to achieve full-thickness resection without transluminal access,NEWS is expected to be a promising surgery (48).
Expanding indication of SN biopsy for upper gastrointestinal malignancies
The era of SN navigation surgery will come to light and will become one of the standard procedures for early gastric cancer.To date,ESD has been widely indicated for early-stage gastric cancer.With the improvement of the technique and safety profile,the indication of ESD is expanding. According to the results,patients who underwent ESD and did not achieve curative resection would be candidates for SN navigation surgery.On the other hand,ESD and the healing process of gastric mucosa might affect the lymphatic network.Using a porcine model,Noharaet al.investigated the distribution of lymphatic flows between pre- and post-ESD.Consequently,the distribution of flows remained unchanged in 83% of all lesions,implying that lymphatic flows remained unchanged in most parts of the stomach after ESD (49).In a clinical data review,Mayanagiet al.conducted a retrospective data analysis from Keio University Hospital and proved that SN basin was not greatly affected by endoscopic resection (50).In line with the report,Arigamiet al.reported the result of a retrospective analysis from a single institution and showed that metastatic LNs were contained in SN in patients who previously received endoscopic resection with a noncurative intent.To validate the accuracy of SN concept after endoscopic resection,SNNS conducted a retrospective multicenter study.The individual data of 132 patients who underwent SN mapping after endoscopic resection were collected from 8 institutions.The SN basin distribution was compared between gastric cancer patients with (n=132) or without (n=275) endoscopic resection.According to the results,SNs were not identified in two cases,both of which underwent the single-tracer method in SN biopsy,indicating that the SN detection rate was 98.5%.Of nine cases (6.8%) that had LN metastasis,eight had a metastatic LN within the SNs,and one had a non-SN metastasis while within the SN basin.There was no significant difference in diagnostic sensitivity of SN biopsy between groups (88.9% in the post-endoscopic resection group and 95.7% in the non-endoscopic resection group;P=0.490).The accuracy in diagnosing LN metastasis in SN biopsy was 99.2% and 99.6% (P=0.539),respectively.Consequently,these findings clarified the feasibility of SN concept in patients with gastric cancer who previously underwent endoscopic resection and others (51,52).Since the Korean trial (SENORITA 2) has been targeting post-ESD patients (53),SN navigation surgery might be used in those patients in the near future.
Esophageal or gastroesophageal junction (GEJ) cancer requires highly invasive surgical treatment with high mortality and morbidity,which has dramatically improved in recent years (54,55).Given that esophagectomy would negatively impact the nutritional status,an appropriate modification of the surgical approach can be beneficial for patients.Recently,the mediastinal LN metastasis was shown to be predicted based on the esophageal invasion in GEJ cancer (56).However,there is a remaining difficulty in the preoperative diagnosis of the distance of esophageal invasion.Given that LN metastasis is accurately diagnosed by SN biopsy during surgery,we will be able to modify the surgical approach appropriately.When SN mapping was applied to GEJ cancer,SNs were identified in all the patients (57).Notably,for Siewert type II tumor in particular,the SNs were not detected in the lower mediastinum by intraoperative evaluation,indicating that SN biopsy can be performed without using the transthoracic approach.On the other hand,as previously reported,the distribution of identified SNs was widely spread from the cervical to the abdominal area in thoracic esophageal cancer (58,59).While a validation using an expanded cohort study is required,SN biopsy might provide further insights to predict the distribution of lymphatic flow in GEJ cancer patients.With the development of the transmediastinal approach using robotic surgical systems (60,61),the mediastinal SN biopsy might help to determine the indication of transthoracic esophagectomy and appropriate field of LN dissection(62,63).
Conclusions
More than 20 years have passed since SN biopsy was introduced in gastric cancer.We believe that the current phase III trials from Japan and Korea will prove the safety and efficacy of SN navigation surgery for early gastric cancer patients.With the development of SN biopsy procedure and treatment modalities,the application of SN biopsy will be expanded to achieve an individualized minimally invasive surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Recent updates and current issues of sentinel node navigation surgery for early gastric cancer
- Screening for gastric cancer in China:Advances,challenges and visions
- Current status and future perspectives on neoadjuvant therapy in gastric cancer
- Current status of lymph node dissection in gastric cancer
- Clinical challenges in neoadjuvant immunotherapy for non-small cell lung cancer
- Laparoscopic surgery for gastric cancer:Current status and future direction