The role of free tissue transfer in reconstruction of full thickness scalp defects
2021-05-09SaraYangMeganWuAmyPittman
Sara Yang, Megan S. Wu, Amy L. Pittman
1Department of Otolaryngology Head and Neck Surgery, Loyola University Medical Center, Maywood, IL 60153, USA.
2Department of Otolaryngology Head and Neck Surgery, Loyola University Chicago Stritch School of Medicine, Maywood, IL 60153, USA.
Abstract Aim: Describe our institutional experience with different forms of reconstruction, including free tissue transfer vs. other newer techniques such as Integra, an artificial dermis composed of bovine collagen lattice with a layer of an artificial synthetic silicon epidermis.Methods: We performed a retrospective review of patients who underwent full-thickness scalp reconstruction at a single tertiary care institution between January 2016 and March 2021. Patient demographic information, comorbidities, defect depth and size, reconstruction type, American Society of Anesthesiologists (ASA) score, and postoperative complications were collected.Results: Of the total 32 patients collected, 68.7% were male and 31.2% were female with an average age of 57.88 years (range 3-91 years). Malignancy (n = 26, 81.2%) was the most common reason for scalp reconstruction, followed by trauma (n = 5, 12.5%) and non-healing wound/exposed hardware (n = 2, 6.2%). The majority of patients underwent reconstruction with Integra +/- split thickness skin graft (n = 15, 46.8%) followed by tissue expander in combination with local flap (n = 6, 18.7%) and microvascular reconstruction (n = 5, 15.6%). Patients who underwent reconstruction with Integra had more medical comorbidities and a higher ASA score (2.93 ± 0.25) than those who underwent free tissue transfer (2.75 ± 0.96). Large defects (> 6.1 cm) were mostly reconstructed via the Integra/Integra + STSG method (n = 13, 59.1%), and all immunosuppressed patients were reconstructed with Integra (n = 3, 100%). Scalp defects with exposed dura were all reconstructed with free tissue transfer (n = 3, 100%). Four Integra-reconstructed patients required revision surgery due to partial graft failure.Conclusion: Free tissue transfer is widely used to reconstruct large and full-thickness scalp defects. However, Integra can be a viable option in patients with numerous medical comorbidities or extensive scalp defects requiring complex reconstruction.
Keywords: Free tissue transfer, full-thickness scalp defects, Integra, scalp malignancy
INTRODUCTION
Acquired scalp defects can be a result of trauma, burns, tumor resection, chronic non-healing wounds, or radiation necrosis. Defects can vary in size and depth. It can involve hair-bearing and non-hair-bearing skin. Reconstruction is often challenging due to the complex anatomy of the scalp.
Anatomy
Scalp thickness ranges from 8 to 13 mm, often thicker in patients with advanced age, males over females, and increasing levels of body mass index (BMI)[1,2]. The layers of the scalp have been well described in previous literature and remembered by the mnemonic “SCALP”: S - skin, C - connective tissue, A - aponeurotic layer, L - loose connective tissue, and P - periosteum[3-5].
The skin covering the scalp often contains hair follicles and numerous sebaceous glands. The connective tissue layer is where the dense vascular supply of the scalp is located, resulting in the richest blood supply of any area of the skin in the body[5]. Branches of the internal and external carotid arteries contribute, including the supraorbital and supratrochlear vessels (internal carotid artery) and the superficial temporal, posterior auricular, and occipital vessels (external carotid artery)[6]. The aponeurotic layer is also known as the galea and is the source of strength of the scalp. This thick connective tissue layer results in the scalp inelasticity and the convex shape of the skull, making closure with local flaps more difficult[7]. Galeotomies or galeal scoring techniques can be used to relax and reduce tension during closure[8]. In addition, the loose connective tissue accounts for the mobility of the scalp over the underlying skull. Lastly, the periosteum over the skull, also called the pericranium, is responsible for providing nutrition to the bone.
Reconstruction
Reconstruction of scalp defects can range from nothing with healing by secondary intention[9], simple reconstruction such as primary closure, local rotational flaps[10]or advancement flaps[11], skin grafting (partialvs.full-thickness)[12], tissue expansion[13], to more complex procedures such as microvascular free tissue transfer[14].
In recent decades, the Integra Dermal Regeneration Template® has been utilized as an option for the reconstruction of complex scalp defects, even with exposed calvarium. It is an artificial dermis composed of a bovine collagen/glycosaminoglycan polymer lattice covered by a thin synthetic silicone epidermis[19]. This has provided an alternative to defects that otherwise would have been closed with free tissue transfer. Studies have shown similar outcomes in terms of the quality of closure technique and in relation to cost[20]. In addition, Integra has the benefit of spared donor site morbidity, reduced operative time, and reduced inpatient stay compared to free tissue transfer, making it a viable option for patients who have significant comorbidities.
Microvascular techniques are certainly utilized in select scenarios at this academic center, a tertiary care referral center for complex cancer and trauma cases. The purpose of this paper was to evaluate the frequency of free tissue transfervs.other techniques such as reconstruction with Integra for the closure of full-thickness defects of the scalp and associate common factors which led to the reconstructive choice.
METHODS
After obtaining institutional review board approval, a retrospective review was conducted between January 2016 and March 2021. All patients who underwent full-thickness scalp reconstruction at a single tertiary care institution were identified. Information regarding patient demographic, medical co-morbidities, smoking history, prior chemotherapy or radiation history, pre-existing coagulopathy, defect etiology, size, depth, reconstruction type, postoperative complications, and any revision surgery were obtained. Patient’s calculated American Society of Anesthesiologist (ASA) classification score given by the anesthesia service at the time of surgery was also recorded to capture the patient’s risk of peri-operative morbidity and mortality.
Defect size was defined as small (< 3 cm), medium (3.1-6 cm), and large (> 6.1 cm). Defect depth was categorized as full-thickness defects of the scalp and partial or full-thickness defects of the calvarium with dura exposure. Reconstruction was categorized as either skin graft, Integra only, Integra followed by splitthickness skin graft (STSG), local flap, regional flap, tissue expander followed by local flap, or free tissue transfer. Postoperative complications were categorized as acute (occurring during a hospital stay)vs.subacute (occurring after a hospital stay). Acute complications were more related to free tissue transfer complications such as arterial or venous thrombosis, flap death, hematoma, infection, or revision surgery. Subacute complications included skin graft loss, Integra failure, flap necrosis, or infection.
RESULTS
Demographic information
A total of 32 patients with full-thickness scalp and/or partial or full-thickness calvarial defects were identified for qualitative data review. The average age was 57.88 years (range 3-91), with 22 males (68.7%) and 10 females (31.2%). All patients were of Caucasian ethnicity. Common medical co-morbidities included hypertension (n= 15, 46.8%), heart disease, (n= 6, 18.7%), diabetes mellitus (n= 6, 18.7%), chronic kidney disease (n= 4, 12.5%), obesity defined as BMI between 30 and 40 (n= 6, 18.7%), and severe obesity defined as BMI > 40 (n= 2, 6.25%). History of anticoagulation use prior to surgery was identified in 7 patients that underwent reconstruction (21.8%). Three patients (9.4%) were immunosuppressed at the time of treatment, and nine patients had a prior history of radiation therapy.
ASA scores calculated by Anesthesia at the time of surgery were averaged for Integra patients (2.93 ± 0.25)vs.free tissue patients (2.75 ± 0.96), see Figure 1. In addition, medical co-morbidities in Integra patients were compared against free tissue transfer patients in Figure 2.
Reconstruction type
The majority of patients underwent reconstruction with Integra/ Integra + STSG (n= 15, 46.8%) followed by tissue expander with local flap reconstruction (n= 6, 18.7%). Free flap reconstruction was pursued in 5 patients (15.6%) with 2 latissimus dorsi flaps, 2 radial forearm free flaps, and 1 anterolateral thigh flap. STSG only or local flap reconstruction was completed in 3 patients each, respectively (9.4%). The most common reason for scalp reconstruction was malignancy (n= 26, 81.2%) followed by trauma (n= 4, 12.5%), and nonhealing wound/exposed hardware (n= 2, 6.2%), see Figure 3.
The organ played and the children’s voices in the choir sounded soft and lovely. The bright warm sunshine streamed through the window into the pew where Karen sat, and her heart became so filled with it, so filled with peace and joy, that it broke. Her soul flew on the sunbeams to Heaven, and no one was there who asked after the Red Shoes.
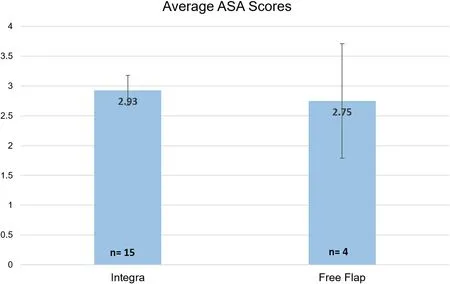
Figure 1. Mean American Society of Anesthesiologist (ASA) classification scores (+/- SD) recorded at the time of surgery for patients with Integra reconstruction (n = 15) vs. free flap reconstruction (n = 4).
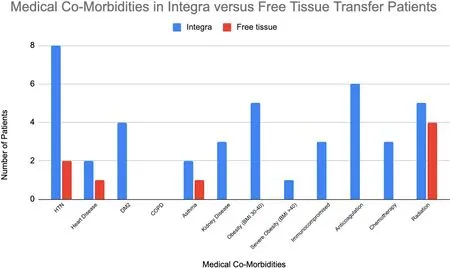
Figure 2. Comparing frequencies of medical co-morbidities among patients with Integra reconstruction vs. free tissue transfer. In this figure, all patients with DM2, kidney disease, obesity, severe obesity, immunosuppression, anticoagulation therapy, or prior chemotherapy underwent Integra reconstruction.
Defect size and depth
The majority of the large defects (n= 22) were reconstructed via the Integra/ Integra + STSG method (59.1%). Breakdown of defect size and type of reconstruction can be seen in Figure 4.
Previously radiated patients were either reconstructed with free tissue transfer (n= 4, 12.5%) or Integra (n= 5, 15.6%). Immunosuppressed patients were all reconstructed with Integra (n= 3, 100%).
All exposed dura defects were reconstructed with free tissue transfer (n= 3, 100%). The majority of the partial bone defects with intact inner calvarium were reconstructed with Integra (n= 12, 63.1%), see Figure 5.
Complications
Four patients reconstructed with Integra were required to return to the operating room for revision surgery. Patient 1 had a persistent area of exposed bone and required coverage with more Integra. Patient 2 had a history of prior kidney transplant with poor wound healing and only had 60% Integra take, requiring another layer to be placed. Patient 3 developed a hematoma under the Integra, preventing any take of the graft. Finally, patient 4 had 85% take with a small area of exposed bone that developed while undergoing radiation treatment.
One patient reconstructed with a local flap required revision surgery due to distal necrosis. Integra was used for coverage of the defect. Patients reconstructed with local flaps, tissue expanders followed by local flaps, or free tissue transfer did not have any post-surgical complications.
DISCUSSION
Reconstruction of large and full-thickness scalp defects has been challenging. However, the advent of microvascular free tissue transfers in 1959 has greatly expanded the options and versatility of reconstruction[21]. It provides consistently vascularized tissue and more robust soft tissue volume, especially important if postoperative radiation is pursued[22]. Thus, it has been established as an efficacious method. Traditionally, the latissimus dorsi flap[23,24]has been the most commonly used, but the anterolateral thigh flap has also emerged in recent years as another frequently used flap[25-27]. The radial forearm flap[28], rectus abdominus flap[29], and free omentum covered by a skin graft[30]are other described forms of reconstruction.
Some proponents for free tissue reconstruction of scalp defects argue that this may be the more conservative option given that other methods of reconstruction such as local flaps or STSG may result in the need for multiple procedures, prolonged wound care, and unsatisfactory aesthetic result[31]. Numerous algorithms have been previously published in literature with recommendations on how to reconstruct large and/or fullthickness scalp defects. Prior literature has suggested free tissue transfer [Figure 6] with defects larger than 100 cm2and previously irradiated scalps[32], defects > 100 cm2wanting single stage reconstruction[33], size > 8 cm[18], and large scalp defects defined as > 90 cm2whether they are partial or full-thickness[34].
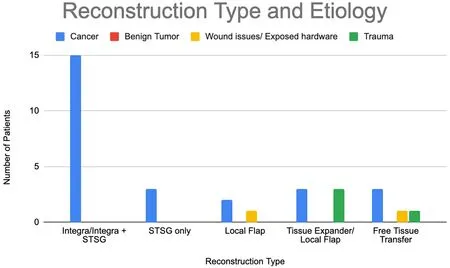
Figure 3. Comparing frequencies of reconstruction type among different scalp defect etiologies (cancer, benign tumor, wound issues/exposed hardware, trauma). Most of the scalp defects following excision of malignancy were reconstructed with Integra (n = 15, 57.7%).
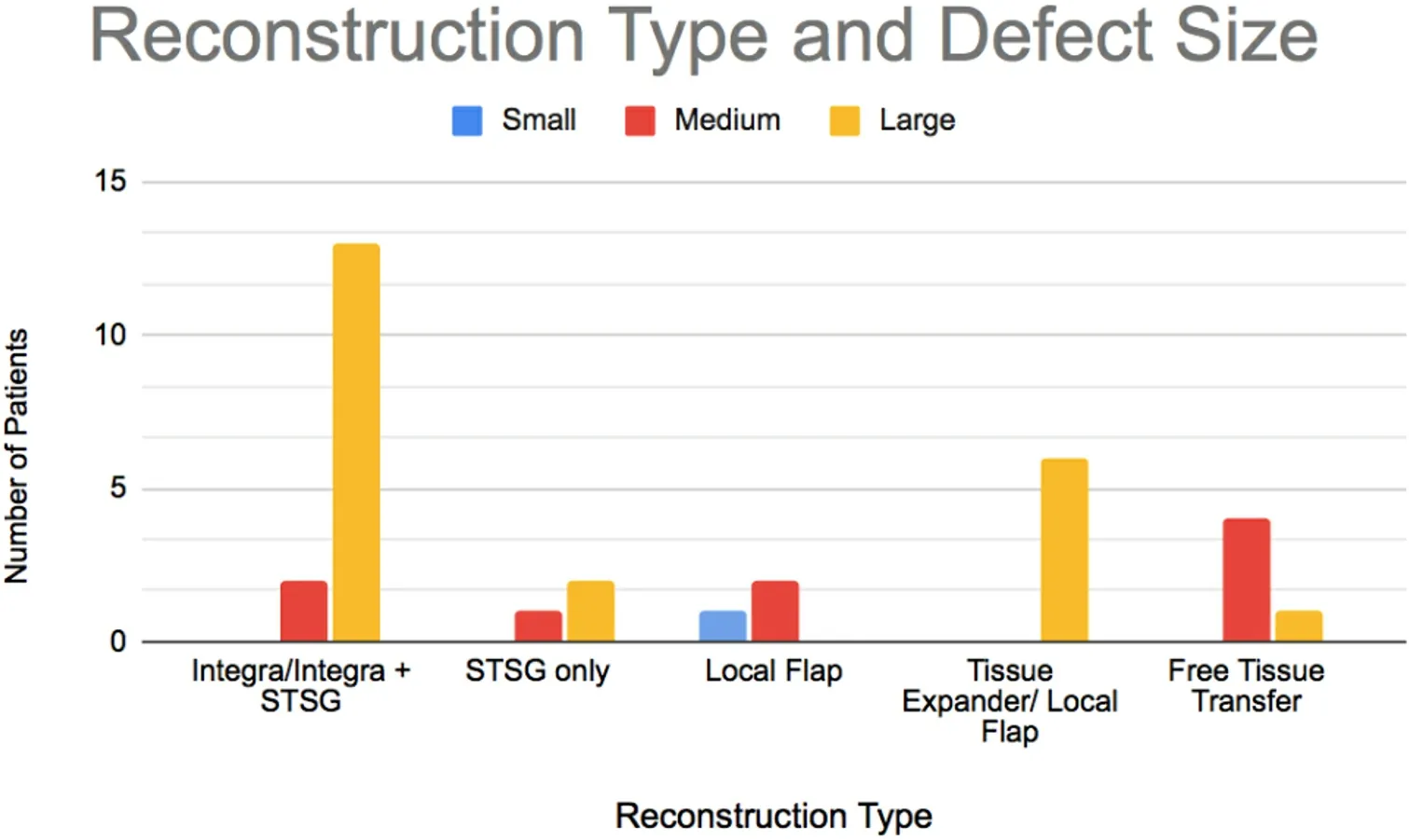
Figure 4. Comparing frequencies of reconstruction type among defect sizes (small < 3 cm, medium 3.1-6 cm, large > 6.1 cm). Large defects were mostly reconstructed using Integra (n = 13, 59.1%).
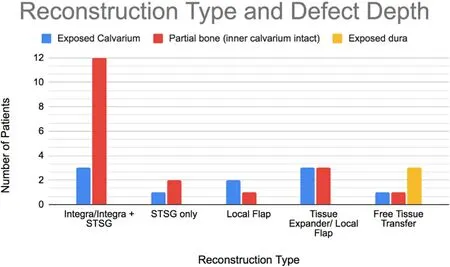
Figure 5. Comparing frequencies of reconstruction type among different defect depths (exposed calvarium, partial bone with intact inner calvarium, exposed dura). Most of the partial bone defects were reconstructed via Integra (n = 12, 63.1%).

Figure 6. (A) Basosquamous carcinoma of the scalp with calvarium invasion. (B) Left frontoparietal craniotomy defect and dura resection with dura patched. (C) Latissimus dorsi free flap with skin graft placement without calvarial reconstruction. (D) Six weeks postoperative visit with a well healed wound.
Free tissue transfer is not without its risks of associated surgical complications such as flap failure and medical complications related to longer operative times and inpatient stays. Older age has been suggested as a possible risk factor for postoperative complications following microvascular procedures, but numerous studies have proven that age alone was not an independent risk factor[35-40]. Rather, frailty and patient comorbidities may provide a more meaningful evaluation of an elderly patient’s candidacy for surgery and ability to tolerate general anesthesia[41]. Frailty can be calculated using the Modified Frailty Index, with higher scores associated with higher complication rates and prolonged recovery[41,42]. In addition, ASA classification is an instrument with a proven predictive value toward complication rates and peri-operative morbidity and mortality. Thus, free tissue transfer is a viable option for reconstruction in patients who have been risked stratified by one of these many metrics.
Integra Dermal Regeneration Template® has recently emerged in the last few years as an option for scalp reconstruction, even for large and full-thickness defects[43]. When there is absent pericranium and exposed calvarium, Integra allows for immediate closure of wounds without significant associated donor site morbidity. The outer table of the calvarium can be burred until there is bleeding bone, like what is typically performed prior to STSG placement[43]. However, prior studies have shown that laying the Integra without any burring of the bone does not affect the percent take of the Integra[44-47]. The Integra is laid directly over the calvarium, and after a delayed period of time to allow for a layer of granulation tissue to form in the wound bed, a skin graft can be placed over but is not necessary [Figure 7]. Integra placement can be performed under sedation, limiting the morbidity with general anesthesia. Figure 1 compares ASA scores of patients who underwent standard of care with microvascular reconstructionvs.a newer method of reconstruction with Integra. It reveals that patients selected for Integra reconstruction often had elevated ASA scores. Although the results are not statistically significant, they demonstrate a selection bias toward pursuing Integra reconstruction in patients with an increased risk of complications with general anesthesia exposure. Integra has also played a role in reconstructing scalp defects following the excision of malignancy and previously has been demonstrated to be successful[48-50]. Overall, prior literature has supported the durability of Integra, reporting 95%-100% graft take even after adjuvant radiation therapy[50,51].
Our institution recently implemented Integra use as a form of reconstruction during the past two years. A review of our patients revealed that an overwhelming majority of our large and full-thickness scalp defects were reconstructed using Integra. These subsets of patients were also found to have a higher ASA score or numerous medical co-morbidities that would increase the risk of postoperative complications with exposure to lengthy general anesthesia. We found success in the percentage of graft take and limited donor site morbidity, especially in patients that had poorer baseline functioning.
The four complications were due to failure for complete graft take with partial exposure of underlying bone. In all these cases, inconsistent and inadequate pressure was applied over certain areas of the Integra reconstruction, allowing serous or sanguineous fluid to collect between the wound bed and the graft [Figure 8]. Like any other skin graft, this prevents attachment and results in graft loss. In patients who required revision surgery due to inadequate Integra takes, usually, a wound vac was placed over the Integra to create a complete and consistent seal. We began implementing wound vac placement over large Integra reconstructions to prevent failure of graft take.

Figure 7. (A) Multiple full-thickness scalp defects after excision of squamous cell carcinoma. Underlying calvarium drilled until bleeding bone was exposed. (B) Three weeks after Integra graft placement. The wound demonstrates a bed of healthy granulation tissue. (C) Three months postoperative visit. The wound healed without skin graft placement.

Figure 8. (A) Large full-thickness scalp defect after dermatofibrosarcoma excision reconstructed with Integra. Silicone sheet removal 3 weeks after Integra placement. (B) Area of exposed bone with incomplete coverage with granulation tissue. (C) Close examination of the area reveals neovascularization of the bone. (D) The second layer of Integra placed. (E) Three weeks after second Integra placement, wound bed covered with a meshed skin graft. (F) Four months post-reconstruction.
Integra was also noted to be useful for patients in whom hair-bearing reconstruction is desired. It provides for immediate and reliable wound closure, with no additional donor site. Tissue expander placement can then be applied six weeks later to achieve the hair-bearing closure. Free tissue transfer could be used in this circumstance as well but has the additional donor site morbidity and operative time that is unnecessary.
Integra also allowed for the reconstruction of multiple different simultaneous scalp defects. This was especially useful in patients with an extensive history of cutaneous head and neck cancers from prior sun exposure or the immunosuppressed patient with a history of prior transplant surgery. Multiple defects could be addressed at the same time[50], reducing the need for multiple procedures. It was also a useful tool in cases where there was high suspicion for recurrence[44], and free tissue transfer could be saved for use later on.
Reconstruction with Integra would not be an ideal long-term reconstruction in a patient with full-thickness scalp and full calvarium defect with exposure of the underlying dura. Abbas Khanet al.[51]described reconstruction of a large full-thickness scalp and calvarial defect that developed due to postoperative ischemia following an aneurysm clipping. Integra reconstruction appeared to be more of a temporizing measure rather than a functional or viable restoration. In addition, Integra cannot be used for a patient where cranioplasty with prosthetic material is planned for calvarial reconstruction[20]. Free tissue transfer must be employed in these cases if there is a co-existing scalp defect.
A limitation in our study and prior institutional studies is the retrospective nature and the lack of a large cohort of patients. In addition, due to the low number of patients in the study, statistical analysis cannot be performed. Therefore, the data should be interpreted as merely an institutional experience and for algorithmic guidance. The data also fails to capture the discussions with patients and families regarding reconstruction options with the final decision made based on individual patient presentation and decision.
Free tissue transfer remains the ideal form of scalp reconstruction, but in patients that have been identified as having higher morbidity associated with a complex reconstruction, Integra can be an alternative reconstructive tool. Success with Integra reconstruction largely lies in the appropriate patient selection.
DECLARATIONS
Authors’ contributions
Data collection, analysis, writing of manuscript, editing: Yang S
Data collection, analysis, editing: Wu MS
Design, analysis, writing of manuscript, editing: Pittman AL
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Consent was obtained from patients for publication of Figures 6-8.
Copyright
© The Author(s) 2021.