Heart failure in the elderly
2021-04-30PabloezVillanuevasarJimnezndezFernandoAlfonso
Pablo Díez-Villanueva, César Jiménez-Méndez, Fernando Alfonso✉
Cardiology Department, Hospital Universitario La Princesa, Universidad Autónoma de Madrid, CIBER-CV, Madrid,Spain
ABSTRACT Heart failure (HF) is a clinical syndrome caused by structural and/or functional cardiac abnormalities, resulting in a reduced cardiac output and/or elevated intracardiac filling pressures at rest or during stress. HF is a major public health problem with high prevalence and incidence, involving both high morbidity and mortality, but also high economic costs. The incidence of HF progressively increases with age, reaching around 20% among people over 75 years old. Indeed, HF represents the leading cause of hospitalization in patients older than 65 years in Western countries. Hence, some authors even consider HF a geriatric syndrome, entailing worse prognosis and high residual disability, and often associating some complex comorbidities,common in older population, that may further complicate the course of the disease. On the other hand, however, clinical course and prognosis may be often difficult to predict. In this article, main pathophysiological issues related to the aging heart are addressed, together with key aspects related to both diagnosis and prognosis in elderly patients with HF. Besides, main geriatric conditions, common in the elderly population, are reviewed, highlighting the importance of a comprehensive and multidisciplinary approach.
Heart failure (HF) is a clinical syndrome caused by structural and/or functional cardiac abnormalities, resulting in a reduced cardiac output and/or elevated intracardiac filling pressures at rest or during stress.[1]HF is a major public health problem with high prevalence and incidence, involving both high morbidity and mortality, but also high economic costs. The incidence of HF progressively increases with age,[2]reaching around 20% among people over 75 years old.[3]Indeed, HF represents the leading cause of hospitalization in patients older than 65 years in Western countries.[4,5]Hence, some authors even consider HF a geriatric syndrome, entailing worse prognosis and high residual disability, often associating some complex comorbidities, common in older population, that may further complicate the course of the disease.[3,6]However, clinical course and prognosis may be often difficult to predict.[7,8]
In this article, main pathophysiological issues related to the aging heart are addressed, together with key aspects related to both diagnosis and prognosis in elderly patients with HF. Besides, main geriatric conditions, common in the elderly population, are reviewed, highlighting the importance of a comprehensive and multidisciplinary approach.
THE AGING HEART
HF globally represents an altered signalling syndrome, not only paracrine but systemic. Pulmonary hypertension, inadequate skeletal muscle vasodilation or inability to excrete a sodium load, are some consequences of this syndrome that may lead to poor functional capacity and quality of life, as well as high mortality, even in the short-term.[9]Many of these processes have peculiarities in the elderly population and might be individually targeted by specific interventions, though just a few have proved to improve outcomes in these patients.[10]
The main physiological changes in the heart and cardiovascular system related with aging are summarised in Table 1.[11]Some of the main mechanisms involved in cardiovascular aging include: (1) oxidative stress due to mitochondrial dysfunction;[12](2) chronic inflammation (also defined as “inflammaging”), especially in obese patients, together with changes in microbiota and immune dysfunction;[13]and (3) low renewal rate of cardiomyocytes, closely related to limited cardiac regeneration capacity.[14]
HEART FAILURE AETIOLOGY AND DIAGNOSIS
The aetiology of HF is diverse and many causes can potentially overlap, especially in the elderly.Table 2 summarizes most of these entities, including ischemic heart disease, which also represents a highly prevalent cause of HF in elderly population.[15]

Table 1 Physiopathological changes in the heart and cardiovascular system with aging.
HF is diagnosed in the presence of suggestive symptoms and signs, increase in natriuretic peptides and echocardiographic findings (Table 3). HF signs and symptoms may develop acutely or progressively over time, leading in both cases to clinical deterioration and death. They also have low sensitivity and specificity in clinical diagnosis in this population. Typical signs and symptoms are known to be less common in the elderly population, due to the presence of other comorbidities, together with atypical manifestations like confusion, somnolence,anorexia, and reduced level of activity.[16]Dyspnoea is the primary symptom of HF, clinical expression of elevated lung pressures. On the other hand, fatigue, which is also a prevalent symptom,may be related to skeletal muscle hypoperfusion.Thus, the complaint of fatigue should not be considered a trivial symptom. Fine rales at lung bases may constitute a common finding in the elderly due to prolonged bed rest and physical inactivity.
Levels of natriuretic peptides increase with age and may vary in the presence of comorbidities such as obesity, renal impairment or atrial fibrillation.[17]Accordingly, they should be interpreted together with clinical and echocardiographic findings.[18]Nevertheless, the utility of natriuretic peptides in the elderly population is controversial: the BED(BNP Usefulness In Elderly Dyspnoeic Patients)study showed that BNP was not useful for discriminating cardiac vs. respiratory origin of acute dyspnoea in patients ≥ 60 years.[19]On the other hand,data from the TIME-CHF study showed that NTproBNP guided therapy is safe in elderly and highly co-morbid HF patients.[20]
Regarding left ventricular ejection fraction(LVEF), HF can be classified into three categories:(1) HF with preserved ejection fraction (HFpEF); (2) HF with intermediate ejection fraction (HFmEF) or (3) HF with reduced ejection fraction (HFrEF). Management and treatment of these subclassifications significantly differ, although prognosis is somewhat poor. On average, older HF patient are more likely to be female and have HFpEF.[21]Because of the heterogeneity in the presentation of HFpEF, different scales such as H2FPEF score or HFA-PEFF score have been proposed to ease the diagnosis.[22,23]Once the diagnosis of HF has been made, functional status is graded using the New York Heart Association (NYHA) classification (Table 4). The American College of Cardiology (ACC) and American Heart Association (AHA) classification is based on the evolution and progression of the disease in four stages (Table 5). Last, but not least, numerous prognostic markers of HF hospitalization and/or death have been identified in patients with HF, with age also being associated with worse prognosis.[24,25]Specific geriatric conditions, such as frailty, sarcopenia or malnutrition may also associate poorer prognosis, and will be addressed later on this review.
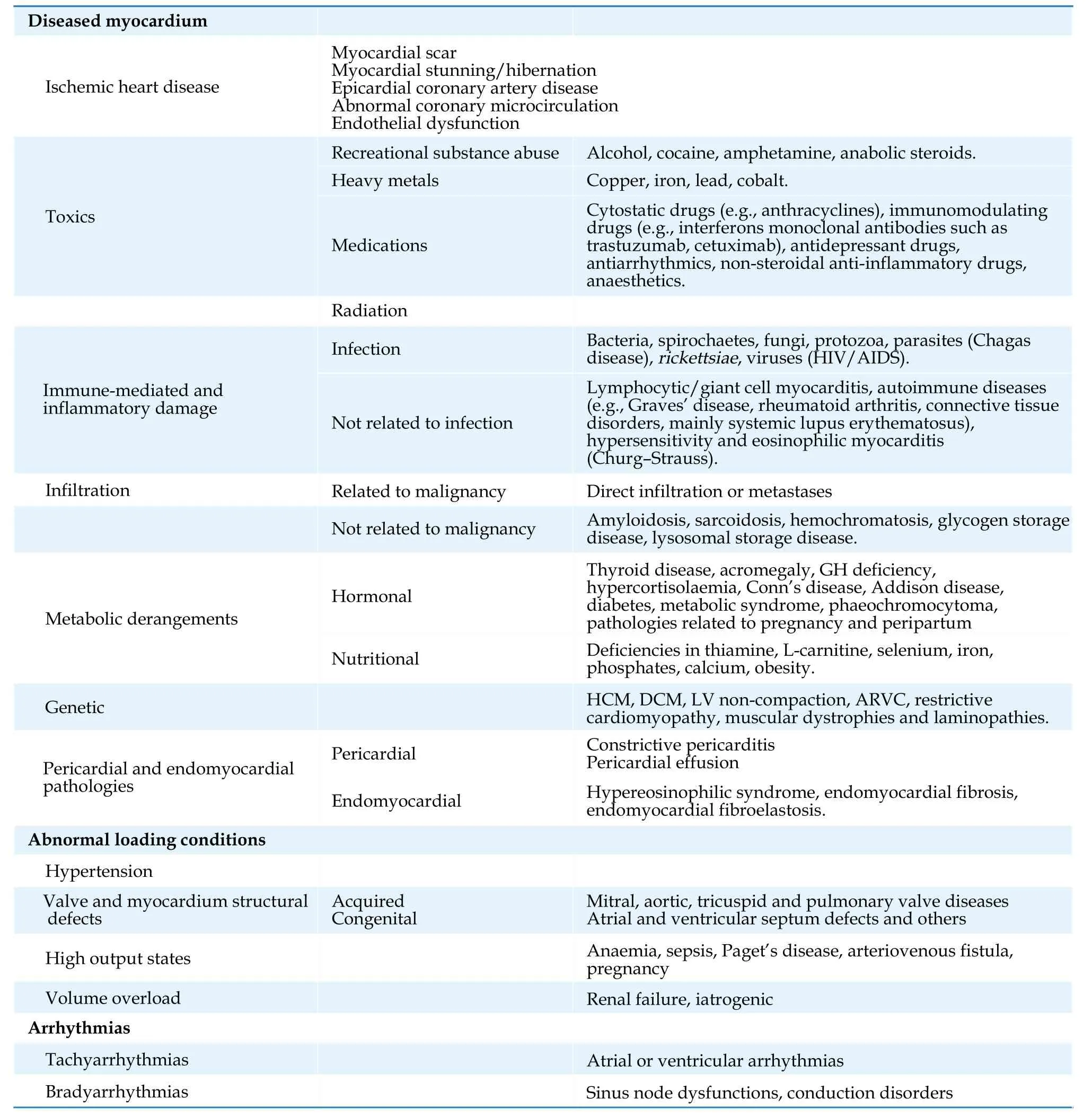
Table 2 Heart failure aetiology*.
Due to its importance and high prevalence in the elderly HFpEF population (estimated to be as high as 17% in this group), cardiac amyloidosis (CA)merits special attention.[26]CA is a severe, progressive, infiltrative cardiomyopathy caused by extracellular deposition of proteins in the myocardium.Transthyretin amyloidosis (ATTR), especially the age-related degenerative form (ATTRwt-wild type),constitutes the leading cause of CA in the elderly.[27]Diagnosis should be suspected in older patients with HFpEF and moderate to severe ventricular wall thickness, then confirmed with bone scintigraphy. Ongoing clinical trials may determine the utility and potential benefits of selected population screening.[28]
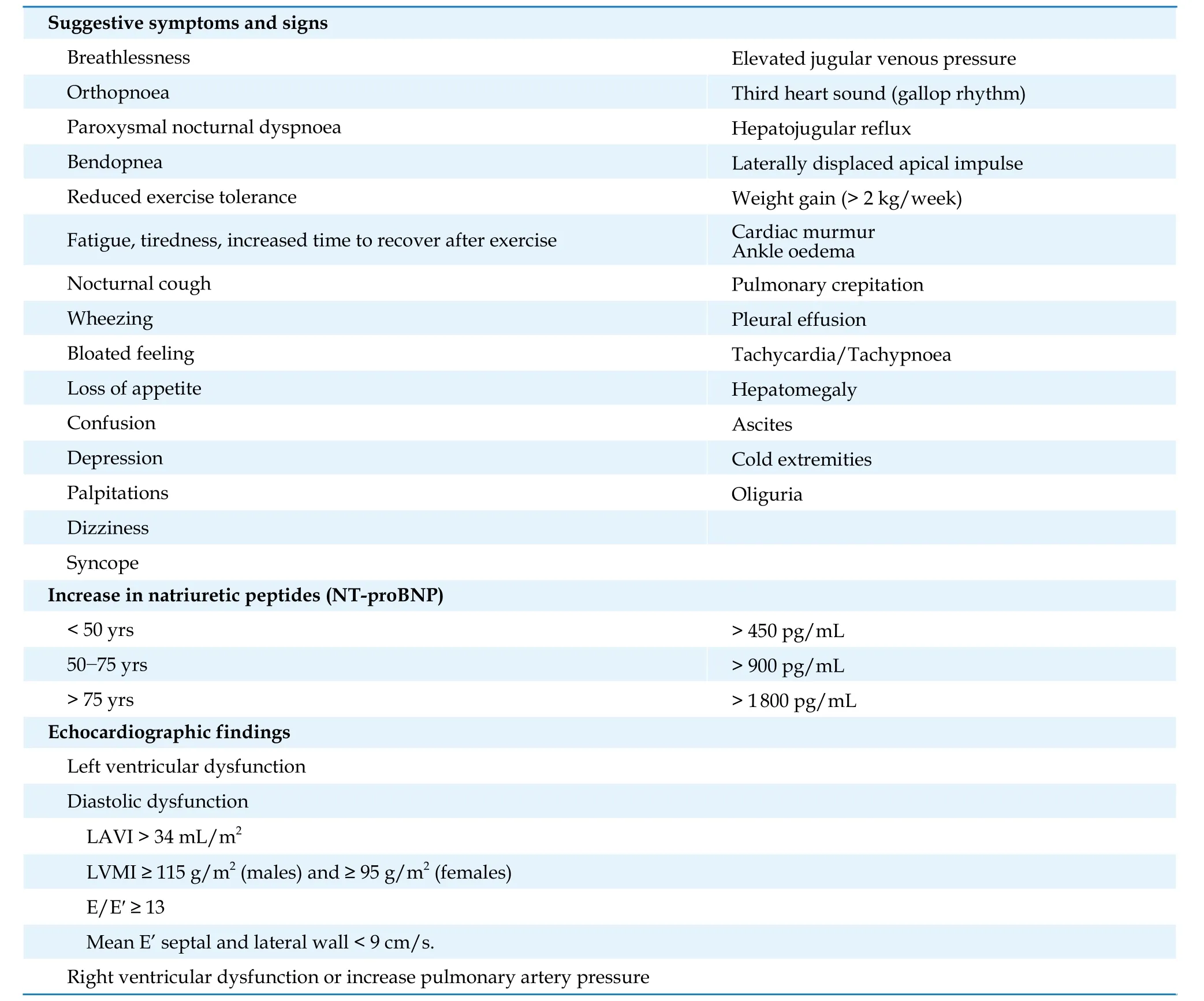
Table 3 Heart failure diagnosis.

Table 4 Heart failure functional NYHA classification.
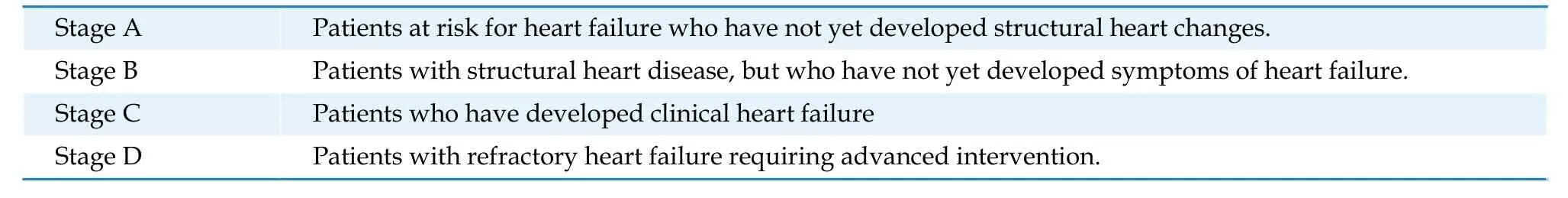
Table 5 Heart failure functional ACC/AHA classification.
HEART FAILURE TREATMENT
Major therapeutic advancements in HF have sprung in the last decades. However, clinical trials usually exclude elderly patients or they may be under-represented, thus raising concern about the external validity of their results.[29]HF treatment consists on both non-pharmacological interventions and pharmacological treatment.
Non-pharmacological Interventions
Non-pharmacological treatment of HF includes appropriate diet with sodium restriction, modest alcohol consumption (less than two units of alcohol a day for men and one unit of alcohol a day for women)and smoking cessation.[1]
Physical activity is highly encouraged. Cardiac rehabilitation programs (CRP) provide a unique tool to achieve good physical condition after HF diagnosis, but also to prevent HF onset. CRP thus constitute a multidimensional therapy with proven major benefits avoiding HF hospitalizations and improving quality of life, significantly in the elderly.[30]Specific CRP, addressing resistance and strength,together with balance training, is associated with better functional capacity in adults ≥ 75 years.[31]As a matter of a fact, selected octogenarians and even nonagenarians can benefit with a similar relative risk reduction but greater absolute risk reductions of events when compared with their younger counterparts.[32]Immunization against influenza and pneumococcus is also highly recommended in patients ≥ 65 years old.[33]
Pharmacological Therapy
Guideline recommendations do not differ by age groups. Of note, different approaches are recommended depending on HF classification according to LVEF. Importantly, and as previously mentioned, comorbidities and polypharmacy are common in the elderly, and so, drugs side effects and interactions.
HFrEF
There are four main pharmacological groups that have demonstrated to improve survival in patients with HFrEF (Figure 1), thus constituting the cornerstone for the treatment of HF with reduced LVEF.[1,34](A) Angiotensin receptor neprilysin inhibitors(ARNi)

Figure 1 Pharmacological treatment in HFrEF. ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor neprilysin inhibitor;HFrEF: heart failure with reduced left ventricular ejection fraction; MRA: mineralocorticoid receptor antagonist; SGLT2i: sodium-glucose cotransporter 2 inhibitor.
The PARADIGM-HF (Prospective Comparison of ARNI [Angiotensin Receptor-Neprilysin Inhibitor]with ACEI [Angiotensin-Converting-Enzyme Inhibitor] to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial) study prospectively compared Sacubitril/Valsartan with Enalapril in HFrEF patients, half ≥ 65 years. The study was prematurely stopped due to significant reduction in cardiovascular and all-cause mortality in patients receiving Sacubitril/Valsartan.[35]A substudy from PARADIGM-HF showed similar beneficial effect from ARNi in older patients despite the fact that they were usually in a more advanced functional status (NYHA III-IV). Of note, hypotension tended to be more prevalent in older patients (those over 75 years), but with no statistical differences when compared with younger patients.[36]A recent observational study showed sacubitril/valsartan is well tolerated in elderly patients, although they often receive lower mean doses.[37]In such study, interestingly, drug withdrawal was more frequent in younger patients and was associated with worse outcomes.[37]Also, sacubitril/valsartan has been found to be associated with LVEF improvement in elderly patients.[38]
Angiotensin-converting enzyme inhibitors(ACEIs)/Angiotensin receptor blockers (ARBs)Concerning ACEIs, perindopril was the first drug that showed a trend to reduce the primary endpoint of HF hospitalization or all-cause death in the PEPCHF (Perindopril for Elderly People With Chronic Heart Failure) trial (HR=0.69, 95% CI: 0.47-1.01;P=0.055).[39]In the CONSENSUS (Cooperative North Scandinavian Enalapril Survival Study) trial,enalapril showed a reduction in mortality and improvement of symptoms in HFrEF patients.[40]Moreover, some studies have demonstrated the higher the dose of ACEIs in the elderly patient, the lesser HF related mortality.[41]
ARBs have associated similar results. The CHARM(Candesartan in Heart Failure—Assessment of Mortality and Morbidity) trial included 7,599 HF patients (3,169 aged ≥ 70 years) that were randomized to candesartan or placebo. The relative risk reduction of the primary outcome (HF hospitalization or cardiovascular death) was similar irrespective of age, while the absolute benefit was greater in older patients.[42]Valsartan was also superior to placebo in the VAL-HeFT trial, showing no differences on outcomes between patients aged < 65 or ≥ 65 years(47% of the trial population).[43]
(B) Betablockers (BB)
Elderly patients with HFrEF in sinus rhythm should receive BB to reduce the risk of death and admission to hospital.[44]
Nebivolol was specifically studied in a prospective clinical trial including 2 128 HF patients aged ≥70 years (35% with LVEF > 35%; 68% with prior history of coronary artery disease) showing a reduction in all-cause mortality or cardiovascular hospitalization.[45]In a sub-analysis of the SENIORS trial,nebivolol also reduced the incidence of ischaemic events.[46]
Age is considered an independent predictor of lower tolerability and side effect of beta-blockers(asthenia, sleep disturbance, symptomatic bradycardia or atrioventricular block). Remarkably, when health education is provided, these agents remain tolerated in > 75% of patient aged ≥ 80 years.
(C) Mineralocorticoid receptor antagonists (MRA)
Previous studies showed MRA were associated with lower hospitalizations in elderly patients with HFrEF.[47]A recent meta-analysis addressing the effect of MRA in patients ≥ 75 years old also showed a reduction in cardiovascular death and all-cause mortality.[48]Worsening renal function was found to be more frequent in elderly patients taking MRAs when compared with those < 75 years, but no hyperkalaemia.[48]MRA should be used with caution especially if renal impairment is present.
(D) Sodium-glucose cotransporter 2 inhibitors(SLGT2i)
SGLT2i such as empagliflozin, canagliflozin and dapagliflozin initially demonstrated to reduce heart failure hospitalizations in diabetic patients.[49]Of note, this pharmacological group does not associate hypoglycaemia unless taken with other hypoglycaemic drugs. Recently, dapagliflozin and empagliflozin have both demonstrated to significantly reduce the composite endpoint of mortality and heart failure hospitalizations in patients with HFrEF irrespective of their glycaemic status,[50]while dapagliflozin has demonstrated to also significantly reduce mortality.Remarkably, DAPA-HF (Dapagliflozin and Prevention of Adverse-Outcomes in Heart Failure) included 60.4% patients ≥ 65 years (24.2% ≥ 75 years),and clinical benefits were also observed irrespective of age.[51]In this study, dapagliflozin was also associated with symptoms improvement without more adverse events.
As previously mentioned, older patients with HFrEF particularly benefit from optimized pharmacological therapy according to current guidelines.[17]This is specially so regarding the quadruple therapy, which would associate the highest benefit in terms of survival and HF hospitalizations, also in very elderly patients.[52]However, different studies and registries show that elderly with HFrEF patients receive less frequently neuro-hormonal blockade.[53,54]Such finding could be potentially explained by different reasons, since this population is less frequently derived to a cardiologist and comorbidities are very prevalent, especially chronic kidney disease, thus hindering proper initiation and titration of prognostic drugs.[55]
Other Drugs
(A) Diuretics
Diuretics are essential to avoid signs of congestion of HF, although their effects on morbidity or mortality have not been demonstrated.[1]Elderly patients are prone to adverse reactions (due to the decline of renal glomerular filtration rate or tendency to hyperkalaemia); hence cautious monitoring is recommended, especially when high doses of loop diuretics are used. Diuretics may also aggravate incontinence, which in turn may lead to self-patient down titration or fluid restriction, thus worsening a previously abnormal renal function.
(B) Digoxin
Age had no influence on the effects of digoxin treatment on outcomes, according to the Digitalis Investigation Group. However, caution should be exerted when using digoxin in the elderly population, given its narrow therapeutic window combined with renal dysfunction. Older women with low body mass index were identified as factors related with digoxin toxicity,[56]which has been associated with increased hospitalizations.[57]
(C) Ivabradine
In the SHIFT trial (Systolic Heart failure treatment with If inhibitor ivabradine Trial) ivabradine was associated with a reduction in the composite endpoint of cardiovascular mortality and HF hospitalization regardless of age, without significant differences in terms of adverse effects, either.[58]Thus, current clinical guidelines support ivabradine use in HF patients (class IIb indication).[1]
(D) Antiplatelet and anticoagulant therapy
Antiplatelet therapy is recommended in ischemic cardiomyopathy while there is no proven benefit in prognosis in HF patients without coronary artery disease.[1]
Similarly, evidence is lacking regarding anticoagulant therapy in patients without atrial fibrillation or other concomitant conditions in which anticoagulation is mandatory.[59]Non-vitamin K antagonist oral anticoagulants are usually preferred over vitamin-K antagonists in AF.
(E) Anaemia and iron deficiency
Anaemia is a common comorbidity in HF patients, especially in elderly women and patients with renal impairment.[60]The aetiology is usually a compound of renal dysfunction, iron deficiency and chronic inflammation. Iron deficiency, which is defined as ferritin ≤ 100 μg/L or ferritin ≥ 100 μg/L but ≤ 300 μg/L and transferrin saturation ≤ 20%, is associated with worse prognosis, independently of anaemia.
To date, three main studies have demonstrated benefit derived from intravenous iron replacement:
(1) The FAIR-HF study firstly showed symptomatic benefits (improved NYHA class, 6-minute walking test and quality of life) secondary to intravenous ferric carboxymaltose (FCM) supplementation in ambulatory HFrEF patients (LVEF ≤ 40%and NYHA II-III) independently of the presence of anaemia.[61]
(2) The CONFIRM-HF study showed not only the above benefits but also lower hospitalization rates in HF patients with LVEF ≤ 45%.[62]
(3) Recently, the AFFIRM-AHF (A Randomised,Double-blind Placebo Controlled Trial Comparing the Effect of Intravenous Ferric Carboxymaltose on Hospitalisations and Mortality in Iron Deficient Subjects Admitted for Acute Heart Failure) trial has been published. After an acute HF episode, FCM was safe and associated with reduced risk of re-hospitalization in this scenario.[63]
Also, a recently published meta-analysis reported that FCM reduces both HF and cardiovascular hospitalizations and associates symptomatic benefits with no effects in all-cause mortality in patients with HF.[64]
Advanced Therapies
Advanced HF therapies comprise cardiac resynchronization therapy (CRT), implantable cardioverter defibrillator (ICD) therapy and left ventricular assist devices (LVAD).
CRT has demonstrated to reduce all-cause death and HF hospitalizations and is recommended in patients with LVEF ≤ 35%, wide QRS and NYHA functional class ≥ II.[1]However, there is little evidence of the benefit of this therapy in the elderly population.[65]In this regard, CRT decreased mortality and HF hospitalization during 3-year follow-up in HF NYHA I-II patients over 60 years old, according to MADITCRT trial.[66]In advanced functional status (NYHA III-IV), post hoc analysis of the MIRACLE and MIRACLE-ICD trials showed CRT benefit in functional class and LVEF in patients over 75 years.[67]Prospective data showed that CRT was as effective in improving LVEF in HF patients ≥ 75 years as in their younger counterparts. CRT also achieved greater reduction in LV end-systolic volume and a much greater QRS reduction in this population.[68]
On the other hand, ICT therapy is indicated in symptomatic HF patients (NYHA II-III) with LVEF ≤35% despite ≥ 3 months of optimal pharmacological therapy and who are expected to survive for more than one year in good functional status, to reduce the risk of sudden death and all-cause mortality.[1]Benefits of ICD especially as primary prevention are less consistent in elderly patients when compared with younger patients,[69]and have been found to be controversial in non-ischemic HF patients.[70,71]In sum, the potential candidates for CRT and ICD therapy should then be carefully selected,also according to quality of life and expectative of survival.[72]
LVAD can be used as a bridge to transplant,bridge to decision, and bridge to recovery or destination therapy. Destination therapy has grown in the last years, though age is commonly associated with comorbidities that exclude heart transplant or LVAD therapies.[73]Some studies have showed no significant differences in survival rates in HF patients between 65-72 years old when compared with younger patients,[74,75]though an increase rate of LVAD related complications (especially gastrointestinal bleeding) has been consistently reported.[75,76]On the other hand, INTERMACS “real world” registry reported a significant decline in 2-year survival of LVAD patients over 70 years (71%vs. 63%) and age itself was found to be an independent predictor of mortality.[77]We can conclude that although age should not be considered an absolute contraindication, it is advisable to carefully select LVAD candidates with lower preoperative risk together with an optimal timing of implantation.[73]
HFpEF
HFpEF represents the most common form of HF in the elderly population, though diagnosis is still challenging, and may require invasive testing in doubtful cases. So far, no drug has improved survival in patients with HFpEF.[22,78]
In the TOPCAT trial, spironolactone showed a decrease in HF hospitalization rates compared to placebo group, although the primary outcome, that also included death from cardiovascular causes,was not achieved.[79]Nevertheless, when restricting the analysis to patients enrolled in the Americas,spironolactone showed a reduction in such composite primary outcome. According to this evidence,ACC guidelines recommend spironolactone (class IIb indication) in HF patients who share the same inclusion criteria than those enrolled in TOPCAT trial (age ≥ 50 years, LVEF ≥ 45%, controlled blood pressure and a serum potassium level ≤ 5 mmol/L).[80]
In PARAGON trial, sacubitril-valsartan showed an improvement in NYHA functional class compared to valsartan, but no differences in HF hospitalizations nor cardiovascular death were found. Exploratory analysis suggests a potential beneficial in patients with LVEF ≤ 55% and early enrolment after a HF hospitalization.[81]
Finally, decongestion with diuretics has also shown to reduce hospitalizations rates.[82]Some other general principles are also important: control of the heart rate if atrial fibrillation is present, optimize blood pressure control and lifestyle interventions as exercise training to improve functional capacity and quality of life. Ongoing studies will evaluate the utility of an individualized approach according to HFpEF phenotypes.[22]
SPECIFIC AGING CONDITIONS
In addition to a higher prevalence of comorbidities, elderly patients with HF present with different and inherent clinical conditions that require adequate recognition and management.
Frailty
Frailty is defined as an age-associated clinical syndrome characterized by a decrease in physiological reserve in situations of stress, constituting a state of vulnerability that entails a higher risk of adverse events.[83]Frailty is common in older adults with HF, even higher than 70% of patients ≥ 70 years of age admitted with acute HF.[84]HF and frailty may share common signs, symptoms, and manifestations. Frailty has been associated with an overall increased hazard risk of 1.5 for hospitalization and mortality in chronic HF,[85]also associating higher 30-day mortality in the acute setting.[86]
It is then essential to recognize and characterize frailty status in patients with HF in order to properly address it. As previously mentioned, CPR plays a key role in frailty approach and treatment.[30]Early multidisciplinary guided plan benefits are currently being evaluated in the ongoing clinical trial DEED FRAIL-AHF, which may demonstrate if a comprehensive care transfer is effective preventing HF hospitalizations in frail acute HF patients discharged home from emergency department without admission.[87]
Ongoing studies including elderly ambulatory HF patients, like the FRAGIC (Impacto de la FRAgilidad y otros síndromes Geriátricos en el manejo clínico y pronóstico del paciente anciano ambulatorio con Insuficiencia Cardiaca (FRAGIC). Estudio prospectivo y multicéntrico) registry may provide further information about the impact of frailty and other geriatric syndromes in a cardiologist-only followed-up population.[88]
Malnutrition
Chronic HF may lead to loss of appetite, malabsorption, and a catabolic state, thus leading to malnutrition, which has been reported to be as high as two thirds in some HF population,[89]and is strongly related to 1-year mortality.[90]Malnutrition is commonly associated with frailty, thus entailing poor outcomes.[91]
Multi-dimensional scores have been developed to diagnose malnutrition, though they are all complex and time consuming. Simple screening tools such as geriatric nutritional risk index (GNRI), controlling nutritional status (CONUT) score, prognostic nutritional index (PNI) and Mini Nutritional Assessment-Short Form (MNA-SF) have been validated in HF patients.[90,92]Screening patients with HF for malnutrition might identify patients at higher risk of adverse outcomes who might benefit from tailored treatments or interventions.
Sarcopenia and Cachexia
Sarcopenia is defined as a progressive and generalised skeletal muscle disorder that involves the accelerated loss of muscle mass and function.[93]It has been defined as the biological substrate of physical frailty.[94]Sarcopenia is increasingly recognised not only as an age-related problem, but also one associated with a range of long-term conditions.[93]The term cachexia identifies situations in which muscles, fat and bone tissue are also affected. Cachexia is characterized by an abnormal catabolic/anabolic balance and is frequently seen in different chronic diseases including chronic HF.[95,96]The most effective strategies to prevent or treat sarcopenia include exercise, nutrition and physical rehabilitation.[97]
Depression
Depression is a common comorbidity that is associated with worse prognosis and clinical status.[98]Routine screening using validated questionnaires(as Yesavage scale or geriatric depression scale(GDS)) is recommended, especially in the elderly population. However, recommendation still lack in most HF guidelines concerning the management of cognitive decline, dementia or depression, beyond interdisciplinary approaches and preventive care.
Self-care
Self-care is defined as a process of maintaining health through health promoting and preventive practices. It is a concept formed of three main aspects: (1) self-care maintenance; 2) self-care monitoring (observing one-self for changes in signs and symptoms); and (3) self-care management (response to those changes when they occur).[99]This matter is of great importance, as some physical or neurological conditions, common in the elderly,greatly impact on quality of life. So, HF patients are frequently unable to perform essential tasks needed for HF self-care, and self-perception of care has been found to poorly correlate with real ability.[100]In this regard, poor self-care ability involves lack of adherence to treatment, failure to identify early signs of congestion, and failure to implement appropriated therapeutic measures, thus associating higher HF readmissions and one-year mortality.[100,101]
Gerotechnology
The rapid global adoption of technologies applicable to health care is occurring concurrently with the growing population of older adults with HF.These technologies allow telehealth, telemedicine and remote monitoring. However, technology progresses have traditionally been limited in the elderly due to insufficient dexterity, visual impairment, cognitive dysfunction or strong personal preferences. So maybe, it's time to change this paradigm. On the other hand, the number of new devices available should also be accompanied by further research on its efficacy, safety, and cost-effectiveness.[102]
Telemedicine is been widely used in the complex times we are living, at the time this review is written, due to coronavirus pandemic disease.[103]In the elderly, there are specifically concerns that should be taken into account in order to provide the best practices that can be simplified following the 5M rule (medications, mental status, mobility, morbidity and most important asking the patient about objectives).[104]
END OF LIFE
Palliative care including symptoms management,psychological, emotional and spiritual support should be properly offered to patients and relatives/caregivers throughout the disease, not only in advanced stages.[8]This approach should be early initiated in patients with HF, thus addressing patients' needs and wishes, who should also participate in decision-making.[7,105]It is recommended to consider turn-off ICD therapies in those patients with frequent readmissions due to end-stage HF.
CONCLUSIONS
HF is a prevalent and complex disease that predominantly affects the elderly. A precise diagnosis is required to provide the treatment that may associate the greatest benefits in terms of both survival and quality of life. It is also important to identify and address specific and frequent aging particularities as frailty and other geriatric conditions. Besides, therapeutic goals should be modulated and adapted to functional status and vital prognosis.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Journal of Geriatric Cardiology
- Hybrid coronary revascularization vs. percutaneous coronary interventions for multivessel coronary artery disease
- Effects of the total physical activity and its changes on incidence, progression, and remission of hypertension
- Association of changes in waist circumference with cardiovascular disease and all-cause mortality among the elderly Chinese population: a retrospective cohort study
- Factors associated with change in frailty scores and long-term outcomes in older adults with coronary artery disease
- Associations between low-density lipoprotein cholesterol and haemorrhagic stroke
