Comparison of outcomes for percutaneous coronary intervention in men and women with unprotected left main disease
2021-04-30ShengWenLIUChangDongGUANFengHuanHUJueCHENKeFeiDOUWeiXianYANGYongJianWUYueJinYANGBoXUShuBinQIAO
Sheng-Wen LIU, Chang-Dong GUAN, Feng-Huan HU, Jue CHEN, Ke-Fei DOU,Wei-Xian YANG, Yong-Jian WU, Yue-Jin YANG, Bo XU, Shu-Bin QIAO,✉
1. Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences, Beijing, China; 2. Catheterization Laboratories, Fuwai Hospital, National Center for Cardiovascular Diseases,Chinese Academy of Medical Sciences, Beijing, China
ABSTRACT BACKGROUND Percutaneous coronary intervention (PCI) in patients with unprotected left main coronary artery disease (ULMCAD) is increasing strategy in coronary artery patients. However, there is a lack of knowledge on the impact of sex on outcomes of patients undergoing ULMCAD PCI. METHODS From January 2004 to December 2015, there were 3,960 patients undergoing ULMCAD PCI at our institution, including 3,121 (78.8%) men and 839 (21.2%) women. The clinical outcome included the incidence of major adverse cardiac events(MACE) (the composite of all-cause death, myocardial infarction (MI), and revascularization), all-cause death, MI, revascularization at three years follow-up. RESULTS Compared with men, women had not significantly different MACE (14.7% vs. 14.6%, P=0.89, all-cause death (3.5%vs. 3.7%, P=0.76), MI (5.0% vs. 4.3%, P=0.38), revascularization (9.1% vs. 8.9%, P=0.86), respectively. After adjustment, rates of MACE (HR=1.49; 95% CI: 1.24-1.81; P<0.000 1) and all-cause death (HR=1.65; 95% CI: 1.09-2.48; P=0.017) occurred more frequently in male patients, as well as revascularization (HR=1.46; 95% CI: 1.16-1.85; P=0.001). CONCLUSION In this analysis, compared to men, women undergoing ULMCAD PCI have better outcomes of MACE, allcause death, and revascularization.
Coronary artery bypass graft surgery(CABG) has long been the standard strategy for unprotected left main coronary artery disease (ULMCAD). However, over the last two decades, there are marked advances in percutaneous coronary intervention (PCI), involving drug-eluting stents (DES), adjunctive antithrombotic drugs, periprocedural management, many studies reported favorable outcomes of PCI of ULMCAD in carefully selected patients.[1-4]
Compared with men, women have additional pathophysiological processes in addition to traditional cardiovascular risk factors. Such areas of ambiguity include the effects of reproductive hormones on inflammatory markers, fat distribution, and atherosclerotic burden as well as a clearer understanding of mental stress-induced and vascular dysfunction-induced ischemia, which is believed to occur more commonly in women than in men.[5-7]
Previous studies have shown differences in outcomes between women and men undergoing PCI.[8,9]However, existing data is limited by smaller sample sizes which makes it challenging to draw robust conclusions regarding efficacy and safety of PCI in women with ULMCAD.[10-12]Despite the guidelines, women are less likely than men to undergo revascularization with CAD. Causes include inherent gender bias and underestimation of patient risk, atypical symptoms on presentation, conflicting data from post-hoc analysis of trials regarding revascularization benefit, and higher vascular complications from the procedure.[13,14]The objective of the present analysis was to investigate the comparative safety and efficacy of PCI between women and men who underwent left main (LM) revascularization.
METHODS
Between January 2004 and December 2015, 3,960 consecutive patients with ULMCAD who underwent PCI in patients at Fu-Wai Hospital in Beijing,China were enrolled. Patients who underwent percutaneous transluminal coronary angioplasty(PTCA) alone or were treated with bare metal stents(BMS) were excluded. The decision for LM PCI was based on consultation with both patients and surgeons in instances of patient refusal for surgery or comorbidity that posed excessive surgical risk.
Interventional strategy and device use including type of stent were left to the discretion of the attending physicians. The patients were pretreated with oral antiplatelet medication consisting of aspirin 300 mg or 100 mg daily and clopidogrel 75 mg daily for at least 5 days, followed by aspirin 300 mg or 100 mg/day indefinitely, and clopidogrel 75 mg/day for at least one year after successful procedure. All patients were evaluated by clinic visit or by phone at 1, 3, 6, and 12 months and annually thereafter. Patients were advised to return for coronary angiography if clinically indicated by symptoms or documentation of myocardial ischemia.Two independent, experienced staff members analyzed all baseline and follow-up angiographic results.
Definitions and Follow-up
The clinical endpoint included the occurrence of major adverse cardiac events (MACE, composed of all-cause death, myocardial infarction (MI) and revascularization), all-cause death, MI, and revascularization. MI was diagnosed by local cardiologists at the hospital of admission according to standard criteria (rise in the creatine kinase level to more than two times of the upper limit of normal with an increased creatine kinase-MB (CK-MB) and newly developed Q waves). Target vessel revascularization (TVR) was defined as revascularization (coronary artery bypass graft (CABG) or PCI) driven by any lesion located in the same epicardial vessel.Target lesion revascularization (TLR) was defined as any revascularization procedure, either percutaneous or surgical, involving the target lesion. The target lesion was defined as the treated segment from 5 mm proximal to the stent to 5 mm distal to the stent. The protocol of our study did not include routine angiography for any subgroup of patients;therefore, virtually all revascularization can be considered clinically driven. Stent thrombosis was defined according to a standardized definition proposed by the Academic Research Consortium(ARC). Follow-up was obtained directly and independently through analysis of the hospital discharge records by clinic visitor by telephone interview. All endpoints were adjudicated centrally by two independent cardiologists and disagreement was resolved by consensus.
Statistical Analysis
Discrete variables were reported as numbers and percentages and continuous variables as means ±SD. Categorical variables were compared with the chi-squared test, while continuous variables were compared using the Student'st-test. For outcomes with < 5 expected values in each category, Fisher's exact test was used. Three-year cumulative incidences were estimated by the Kaplan-Meier method,and differences were assessed with the log-rank test. To reduce the treatment selection bias and potential confounding factors in this study, we performed rigorous adjustment for baseline characteristics by using the weighted Cox proportional hazards regression models with the trimmed inverseprobability-of-treatment weighting (IPW). Results are reported as HR with associated 95% confidence interval (CI) andPvalues. ThePvalue < 0.05 was considered significant. All statistical analysis was performed with SAS software version 9.4 (SAS Institute, Inc, Cary, NC).
RESULTS
Baseline Characteristics
Between January 2005 and December 2015, 3,960 patients with ULMCAD were underdone PCI at our institution, including 3,121 male and 839 female.Complete three-year follow-up was obtained in 96.3% of the male cohort and 95.3% of the female cohort. Baseline clinical characteristics of these patients are listed in Table 1. In general, the two groups were similar regarding hyperlipidemia, peripheral vascular disease, chronic obstructive pulmonary disease, family history of coronary artery disease,prior stroke, left ventricular ejection fraction and clinical presentation. Female cohort was more likely to have higher age and rates of hypertension, diabetes mellitus. However, female cohort has lower rates of prior PCI, prior MI, current smoker, and have lower number of creatinine and body mass index (BMI).
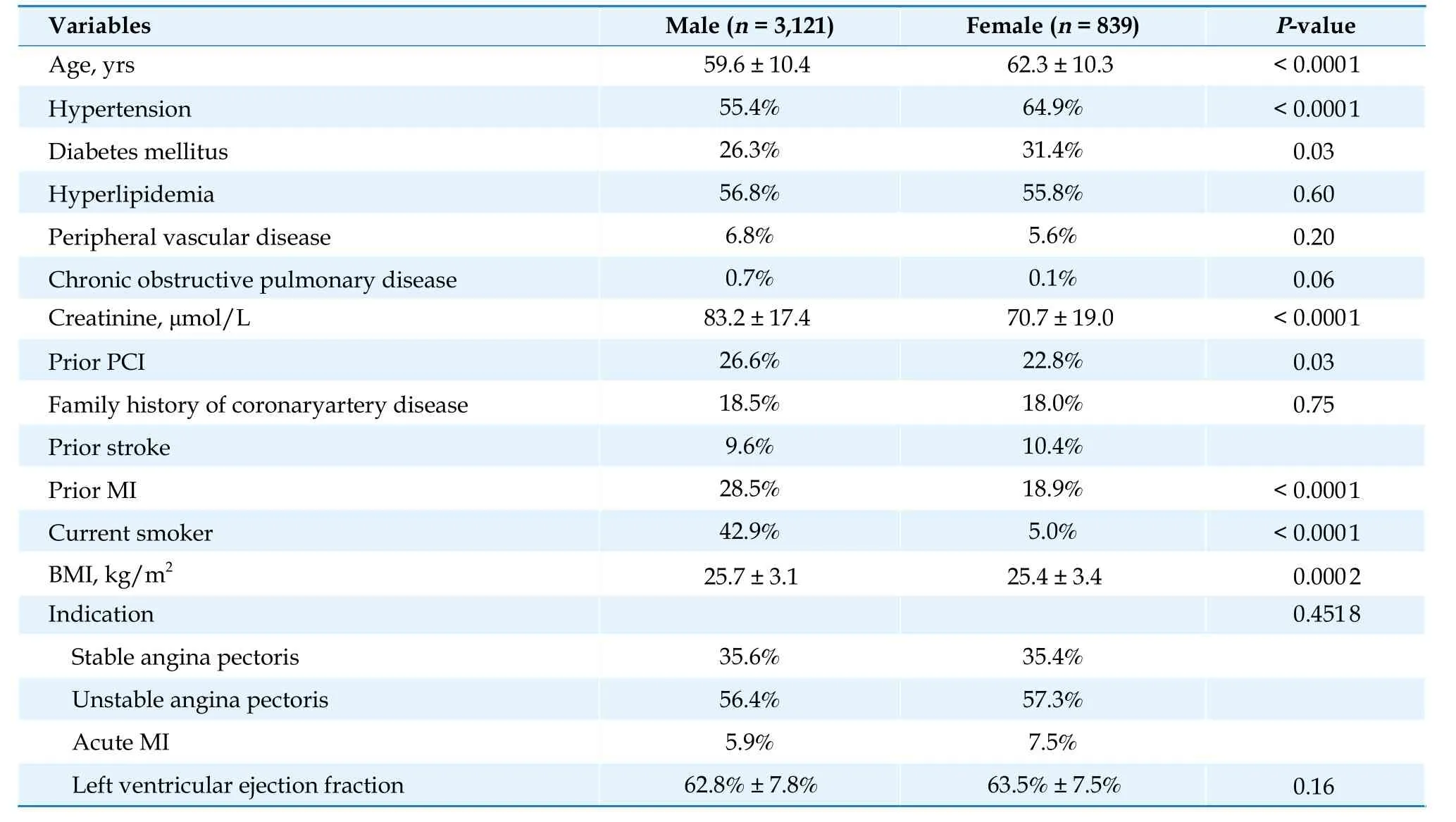
Table 1 Baseline clinical characteristics of patients.
PCI details have been listed in Table 2. Both groups had some similar angiographic and procedural characteristics, including restenotic lesions, calcified lesions, intra-aortic balloon pump use, transradial approach, procedural complications and procedural success. The male cohort had higher rates of LM distal lesion (73.5%vs. 68.5%,P<0.000 1), LM plus 3-vessel disease (39.4%vs. 32.9%,P<0.000 1),bifurcated lesion (82.9%vs. 77.0%,P<0.000 1),IVUS use (9.9%vs. 6.4%,P<0.000 1) and post-dilation (72.9%vs. 68.2%,P=0.006 6). The male cohort also had a higher SYNTAX Score (23.2vs. 22.2,P<0.000 1), as well as longer mean stent length (32.4 mmvs. 31.5 mm,P=0.05).
Clinical Outcomes
The 3-year cumulative incidence of MACE (composed of all-cause death, MI, and revascularization)(14.6%vs. 14.7%,P=0.89) were not significantly different between male and female cohort, as well as all-cause death (3.8%vs. 3.3%,P=0.78), MI (4.5%vs. 5.1%,P=0.39), revascularization (9.0%vs. 9.1%,P=0.87. Overall, the 3-year unadjusted rates of TVR (4.1%vs. 3.3%,P=0.42) and TLR (3.0%vs.3.3%,P=0.40) were also similar in two groups.
After adjusted by IPW model analysis, there were significant higher risks in terms of 3-year MACE(HR=1.49; 95% CI: 1.24-1.81;P<0.000 1) and allcause death (HR=1.65; 95% CI: 1.09-2.48;P=0.017), as well as revascularization (HR=1.46; 95%CI: 1.16-1.85;P=0.005 6) in male group than female group. However, risks of TVR (HR=1.39; 95%CI: 0.97-2.01;P=0.07) and TLR (HR=1.03; 95% CI:0.70-1.51;P=0.87) were similar between two cohorts even after adjustment, as well as MI (HR =1.08; 95% CI: 0.79-1.49;P=0.63) (Table 3 and Figure 1).
DISCUSSION
The major finding of this study is that, for patients with ULMCAD underdone PCI, the cumulative incidence of three years MACE (the composite of all-cause death, MI, and revascularization), allcause death, MI, as well as revascularization are not different in male group and female group. However,after adjustment, rates of MACE, all-cause death and revascularization occurred more frequently in male patients. In addition, male patients with UPLMCAD had an overall worse baseline clinical risk profile than female patients, therefore, male patients had overall more anatomic complexity than women, with higher SYNTAX scores, more left main bifurcation lesions and concomitant multivessel disease.

Table 2 Angiographic lesion characteristics and procedural details.
Evidence from randomized controlled trials proved that PCI is a noninferior revascularization strategy in LM patients compared to CABG. The EXCEL trail found PCI with everolimus-eluting stents was noninferior to CABG with respect to the rate of the composite end point of death, stroke, or MI at three years.[15]The NOBLE study also demonstrated five years mortality was similar after PCI and CABG but patients treated with PCI had higher rates of non-procedural MI and repeat revascularization.[16]The SYNTAX Extended Survival (SYNTAXES) study reported the rates of all-cause death in patients with ULMCAD after PCI was not different from CABG (27%vs. 28%, HR=0.92, 95% CI:[0.69-1.22],P=0.023) at 10-year follow-up.[17]

Table 3 Three-years unadjusted and adjusted cumulative incidence of primary clinical outcomes.

Figure 1 Adjusted Kaplan-Meier curves for male vs. females cohort. MI: myocardial infarction.
In the EXCEL trial, Serruys,et al.[18]analyzed the relative treatment effect of CABGvs. PCI on ULMCAD in men and women paients as pre-specified subgroups. By multivariate analysis, sex was not independently associated with either the primary endpoint (the composite of all-cause death, myocardial infarction, or stroke) (HR=1.10; 95% CI: 0.82-1.48;P=0.53) or all-cause death (HR=1.39; 95% CI:0.92-2.10;P=0.12) at three years. The women treated with PCI had a trend toward worse outcomes (19.7%vs.13.8%,P=0.06), which differences were driven by higher periprocedural rates of myocardial infarction in women.[18]However, SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) trial, in which 1800 patients with multivessel disease (including 705 patients with UPLMCAD) were randomized to PCI versus CABG, women undergoing PCI had a higher adjusted 4-year risk for mortality than men (HR=1.60; 95% CI: 1.01-2.56;P=0.048),whereas CABG outcomes were comparable between the sexes (HR=0.59; 95% CI: 0.32-1.10).[8]MITO Registry also confirmed women had greater comorbidity and more complex lesions, resulting in an increased risk of clinical events. However, after propensity matching, there was no difference in the occurrence of MACE but cardiac death showed a trend to being higher in women compared to men(HR=2.70; 95% CI: 0.98-7.49;P=0.056).[11]These data have shown worse outcomes after PCI of UPLMD in women compared to men, these findings were related to baseline differences in which women had worse risk factor profile and higher anatomic complexity than men.
These studies have showed a worse clinical outcome in women undergoing LM stenting when compared with men, these results in the following studies proved to be inconsistent, which confirmed the clinical outcome risks following PCI were similar between male.[19,20]IRIS-MAIN registry, which recruited 2 328 patients (545 women; 1 783 men) with unprotected left main CAD, the composite outcome of death from any cause, MI, or stroke was similar between the two groups (10.8%vs. 10.8%, respectively, log-rankP=0.587). The results were similar after adjustment for baseline variables and consistent across major subgroups.
In the present study, women had a lower overall risk factor burden and significantly lower coronary anatomic complexity with lower SYNTAX scores and fewer coronary lesions compared with men,which were in accord with a recent study that reported less overall plaque burden and slightly more favorable plaque composition characteristics in women,[21]therefore consistent with female UPLMCAD patients have better clinical outcomes.
LIMITATION
This study is a retrospective analysis of consecutive and nonrandomized patients, however, it carries important and complementary information derived from real-world practice. The present study was also a single-center experience and lacked systematic angiographic follow-up. Finally, although we performed multivariate analysis which is known to be a valuable approach for taking into account the potential confounding effect attributable to between group imbalances, there may have confounders that were not adjusted for that affected the outcomes.
CONCLUSIONS
Our study showed that women undergoing ULMCAD PCI have better outcomes of MACE, allcause death, and revascularization compared to men. Women had a lower prevalence of clinical risk factors and less coronary anatomic burden and complexity than men. Prospective, randomized,longer-term follow-up data in a larger cohort clinical trial will have value in confirming these initial findings.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Journal of Geriatric Cardiology
- Hybrid coronary revascularization vs. percutaneous coronary interventions for multivessel coronary artery disease
- Effects of the total physical activity and its changes on incidence, progression, and remission of hypertension
- Association of changes in waist circumference with cardiovascular disease and all-cause mortality among the elderly Chinese population: a retrospective cohort study
- Factors associated with change in frailty scores and long-term outcomes in older adults with coronary artery disease
- Associations between low-density lipoprotein cholesterol and haemorrhagic stroke
