The prognosis and survival of integrated traditional Chinese and western medicine on glioma:a meta-analysis
2021-04-14BoYuShuZhenLiangMingHu
Bo Yu,Shu-Zhen Liang,Ming Hu*
1Special Medicine, School of Basic Medicine, Qingdao University, Qingdao, China.2Department of Oncology, Qingdao Municipal Hospital,Qingdao,China.
Abstract Objective: To systematically access the effects of integrated traditional Chinese and western medicine treatment versus western medicine treatment alone in glioma. Methods: Published randomized controlled trials were included from electronic databases (Cochrane Library, Pubmed, Embase, Chinese National Knowledge Infrastructure, Wanfang database, Chinese Scientific Journal Database, Chinese Biomedical Literature Database.Deadline on January 30, 2020).The Cochrane handbook was referred to evaluate the methodological quality.Curative efficacy, gastrointestinal side effects, bone marrow suppression, survival time and quality of life(Karnofsky) were compared between the two groups.Meta-analysis was conducted using Reveman 5.3 and Stata 14.0 software. Results:Twelve randomized controlled trials involved 886 cases were selected,including 446 cases in the trial group and 440 cases in the control group.The meta-analysis indicated that the overall efficacy of integrated traditional Chinese and western medicine showed significant improvement compared with western medicine alone.The effects included reduced tumor size (RR = 1.32, 95% CI (1.18, 1.49), P <0.05),gastrointestinal adverse reactions (RR = 0.42, 95% CI (0.30, 0.60), P <0.05), bone marrow suppression (RR =0.437, 95% CI (0.282, 0.677), P <0.05), and improved KPS score (SMD = 0.632, 95% CI (0.312,0.952), P <0.05). Conclusion: For patients with glioma, integrated traditional Chinese and western medicine treatment can be one of the options for a better treatment.
Key words: Glioma, Integrated traditional Chinese and western medicine, Gastrointestinal reactions, Suppressing bone marrow,Meta-analysis
Background
In the clinic,glioma is one of the common malignant brain tumors and accounts for more than 30% of all primary brain tumors [1].In recent years, the incidence of malignant gliomas has significantly increased, especially in the elderly.Studies have found that ionizing radiation, passive smoking, and long-term exposure to organic compounds such as petrochemicals are risk factors for gliomas [2-4].The main treatments for glioma include surgical resection,chemotherapy and radiation[5,6].
Drugs such as lomustine, carmustine, and temozolomide are used in chemotherapy on glioma,however,these drugs may have side effects that bring suffering to patients.It has been the common pursuit to improve the tolerance of postoperative radiotherapy and chemotherapy and enhance the quality of life and long-term prognosis of glioma patients.
Traditional Chinese medicine has been used to cure glioma for years and practitioners have accumulated rich experience in the treatment of cerebral glioma.Integrated Chinese and western medicine (ITCWM) treatment for glioma has drawn researchers’ attention.However, due to the small sample size, the evaluation of clinical efficacy is not consistent.This study conducted a meta-analysis of all the clinical effects of ITCWM in the treatment of cerebral glioma, hoping to provide evidence for the clinical treatment of cerebral glioma with ITCWM.
Methods
Literature search
Search databases: Cochrane Library, Pubmed,Embase, Chinese National Knowledge Infrastructure,Wanfang database, Chinese Scientific Journal Database, Chinese Biomedical Literature Database.All databases were searched from setup to January 30, 2020.The search terms were: "cerebral glioma","cerebral glioma", "glioma", "combination of Chinese and western", "the integrative medicine","integrated traditional Chinese and western medicine", "RCT".Search terms were used individually or jointly according to different databases.Retrieval strategies were attached in Supplemented file.
Inclusion criteria
The articles need to meet the following criteria: (1)clinical randomized controlled trial (RCT).(2)Patients are diagnosed with glioma based on the glioma diagnosis guide[7].(3)Patients in the control group received western medicine, and the trial group accept Chinese medicine combined with western medicine treatment.(4) Karnofsky (KPS) score is greater than or equal to 60.(5) Outcome indicators① Efficacy: according to the WHO evaluation criteria [7], complete remission (CR) means that the lesion disappears and remains for more than four weeks; partial remission (PR) means that the lesion volume is reduced by ≥30%; stable disease (SD)lesion volume is reduced by <30%or increased by <20% lesions progress disease (PD) means that the lesion volume increases by 25% or new lesions appear.CR + PR is effective for treatment.②Adverse effects, including leukocytes,gastrointestinal reactions, etc.③ Survival time:One, two and three-year, etc.④ KPS score before and after treatment.Researches included should meet at least one of the four items.
Exclusion criteria
(1) Repeatedly published literature; (2) non-clinical therapeutic RCT experiments; (3) literature on other treatment methods in the trial group and control group; (4) expected survival period <three months;(5) patients with other malignant tumors; (6) women who are breast-feeding or pregnant.(7) Data records are unknown or data statistics are in error.
Study selection and data extraction
Two evaluators conducted both, independently.If there are disagreements, the third evaluator will be consulted and the result is reached through discussion.For the methodological quality evaluation,Cochrane Handbook "Systematic Review Intervention Version 5.1.0" which was used, with high quality indicated by"yes", low quality indicated by "no", and fuzzy information indicated by "unclear".
Statistical analysis
Meta-analysis was performed using RevMan5.3 and STATA14.0 software [8].Data (clinical efficacy)were analyzed using odds ratios(OR),risk ratio(RR)and 95% confidence interval (CI) as the effect size;measurement data KPS used standardized mean difference (SMD) and 95% CI as results.If the heterogeneity test wasI2 <50% andQ-statistic testP >0.1, use the fixed-effects model for meta-analysis; otherwise, a random-effects model was used for combining analysis or performing a sensitivity analysis, Finally, a funnel chart was used to test the publication bias.If the Begg testP>0.05 and (or) Egger testP>0.05, there is no obvious publication bias; otherwise, there is a potential publication bias.
Results
Article identification and selection
76 articles were retrieved through literature search.After screening (review, animal experiment,statistical method error, no relevant statistics, etc.),twelve articles were finally selected for meta-analysis[9-20].The total number of cases was 886,including 446 in the trial group, and 440 in the control group,including the patient's name, age, gender, treatment method, treatment dose, treatment time, etc.(Figure 1,Table 1).
Articles of quality evaluation
As shown in figure 2a, only three articles use the random number table method [11, 12] and the remained nine articles only mention randomness but not describe specific random methods [12-20].ITCWM treatment method is more expensive than using western medicine alone.In order to obtain the patient’s consent, double-blind experiments cannot be performed.Hence,none of the articles used in this paper conducted double-blindness and allocation concealment.In addition, nine articles reported adverse reactions [9-17].One article records the withdrawal and shedding conditions, but it does not have a statistical effect on the experimental results(Figure 2A and Figure 2B)[11].

Figure 1 Articles screening flow chart

Table 1 The basic information of included studies
Results of meta-analysis
Meta-analysis of effective treatment.Treatment effects of eight articles including 528 patients [10-15,17, 18]were detected (I2= 0%,P= 0.89), suggesting that there was no heterogeneity;therefore,fixed-effects model was selected for meta-analysis.The results showed that Z = 4.73,P<0.00001.(RR = 1.32, 95%CI (1.18, 1.49),P<0.05) (Figure 3).That means in terms of efficacy,compared with the control group,the effect of ITCWM is better.
Meta-analysis of tumor size (CR/PR/SD/PD).Five articles including 270 patients have detailed data records[11,14,15,17,18],I2=0%,andP=0.911,no heterogeneity (Figure 4).To ensure the studies’accuracy and stability, the sensitivity analysis was continued, suggesting that none of the results caused significant interference to this study.The fixed-effects model was selected for meta-analysis, the results show thatZ= 3.05,P<0.005, (OR = 2.011, 95% CI (1.28,3.15),P <0.05).The included articles do not have potential publication biases.The outcome indicated that in terms of specific tumor efficacy, the effect of ITCWM was better compared with the control group.

Figure 3 Meta-analysis of the efficacy of eight studies
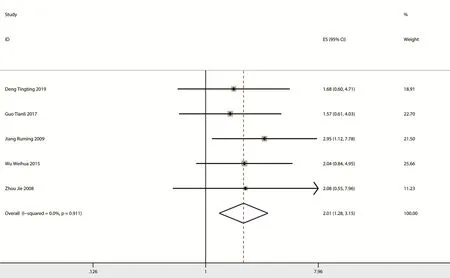
Figure 4 Meta-analysis of complete remission/partial remission/stable disease/progress disease of included studies
Meta-analysis of bone marrow suppression.Seven studies have bone marrow suppression data with 465 patients [10-15, 17].There was heterogeneity as theI2= 63%,P= 0.01 (Figure S5).A sensitivity analysis revealed that Jie Zhou's study [11] had a significant impact on heterogeneity (Figure 5).After removing this study, the results showed no significant heterogeneity (I2= 7%,P= 0.37) (Figure 5), then choose fixed-effects model for meta-analysis.The results showed thatZ=3.71,P<0.00001,(RR=0.44,95% CI (0.28, 0.68),P< 0.05), and there is no potential publication bias in the included articles.The results indicated that in terms of bone marrow suppression,ITCWM had better effects compared with the control group.
Meta-analysis of gastrointestinal adverse reactions.Seven articles including 465 patients [10-15, 17] all have gastrointestinal adverse reactions data in the two treatment methods, due to theI2= 66%,P= 0.007(Figure S6), suggesting heterogeneity and soon a sensitivity analysis found that Jie Zhou's study [11]had a significant impact on heterogeneity.After removing this study, the results showed no heterogeneity (I2= 0%,P= 0.455).Choose fixed-effects for meta-analysis.Showed thatZ= 4.87,P<0.00001, (RR = 0.42, 95% CI (0.30, 0.60),P<0.05) (Figure 6).There is no potential publication bias in the included literature.The results indicate that in terms of gastrointestinal adverse reactions, compared with the control group,the effect of ITCWM is better.
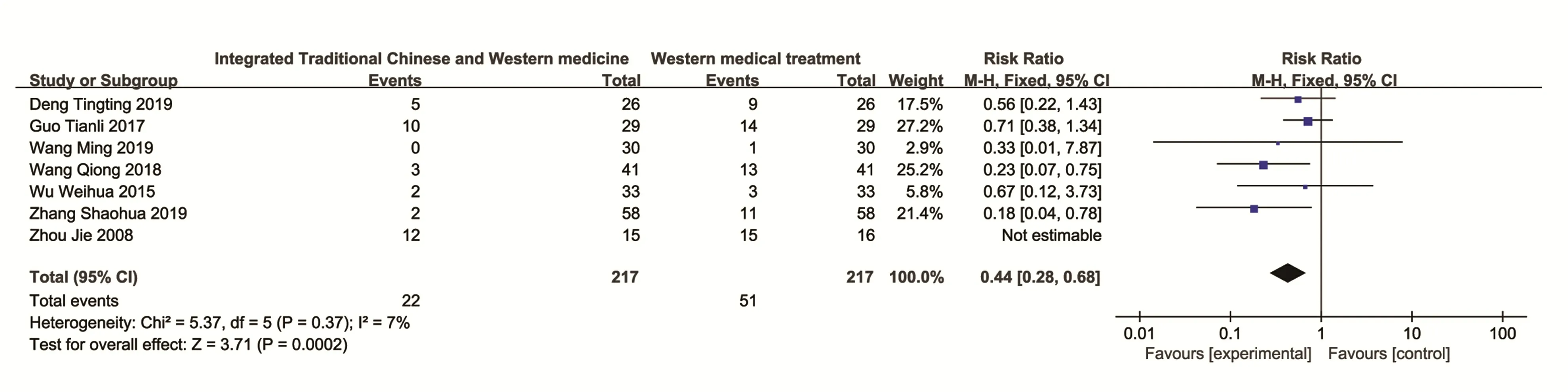
Figure 5 Meta-analysis of bone marrow suppression in seven included studies

Figure 6 A meta-analysis of gastrointestinal adverse reactions data in two groups
Meta-analysis of survival time.Five articles including 337 patients [12, 15, 16, 19, 20] compared the survival time of one-year, two-year, and three-year during the two treatments separately, and the results were meta-analyzed separately.
One-year survival time analysis, becauseI2= 86%,P= 0.00001 (Figure S7A), suggesting that there is significant heterogeneity.Through sensitivity analysis found that Shao-Hua Zhang's[12]and Yan Wang's[15]researches had a greater impact on heterogeneity.After removing them,it showed no obvious heterogeneity(I2= 42%,P= 0.18), Choose fixed-effects model for meta-analysis, showed thatZ= 1.43,P= 0.15, (RR =1.08, 95% CI (0.97, 1.21),P<0.05) (Figure 7A).There is no potential publication bias in the included articles.The results show that the one-year survival time of ITCWM is higher than control group.
Two-year survival time analysis[15,16,19,20],due toI2= 46.8%,P= 0.131, there is no heterogeneity;fixed-effects model was selected for meta-analysis.Showed thatZ= 6.51,P<0.005, (RR = 1.74, 95% CI(1.47, 2.05),P< 0.05) (Figure 7B), there is no potential publication bias in the included articles.The results show that the 2-year survival time of ITCWM is higher than the control group.
Three-year survival time analysis [15, 16, 20], due toI2= 89%,P= 0.0001 (Figure S7B), there is highly heterogeneity.Sensitivity analysis found that Tian-Li Guo's [15] had a significant impact on heterogeneity After removing this study, there was no obvious heterogeneity (I2= 43%,P= 0.19), and the fixed-effects model for meta-analysis shows thatZ=3.65,P=0.0003,(RR=20.33,95%CI(4.03,102.59),P< 0.05) (Figure 7C), and there is no obvious publication bias in the included articles.However, due to the small number of samples included, the results are not reliable, and further statistical studies are needed.

Figure 7 A meta-analysis of different survival times.
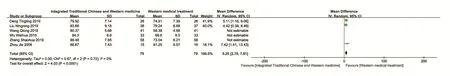
Figure 8 Meta-analysis of Karnofsky scores
Meta-analysis of KPS.KPS scores of Six articles including 422 patients were compared after two treatments [9-12, 14, 17], STATA heterogeneity calculation analysis result (I2= 94.2%,P= 0.0001)suggested there was highly heterogeneity.(Figure S8)Sensitivity analysis found that researches by Shao-Hua Zhang [12], Wei-Hua Wu [17], and Qiong Wang [10] had a greater influence on heterogeneity.After removing them, no significant heterogeneity was found (I2= 0%,P= 0.67), choose fixed-effects model for meta-analysis,and showed thatZ=4.03,P<0.00001, (SMD = 5.25, 95% CI (2.70, 7.81),P<0.05) (Figure 8).Similarly, too many samples are excluded, resulting in insufficient sample size, the result is unreliable,and further research is needed.
Discussion
The morbidity and mortality of brain glioma keep increasing.Surgery combine with radiotherapy and chemotherapy are the main treatments for gliomas[5,6].However,the overall recurrence rate reaches up to 60%~70%, only half of the patients can survive last for more than twelve months [21].Radiotherapy and chemotherapy are accompanied by adverse reactions such as gastrointestinal reactions and bone marrow suppression, which directly affects the quality of life of patients [22,23].Therefore,it is necessary to seek a relatively safe, effective and low-toxicity treatment method.
In recent years, clinical and experimental research on the treatment of brain glioma with Chinese medicine has gradually increased.According to the existing clinical research reports, the clinical effects of traditional Chinese medicine on brain glioma were positive [24-30], which proves that the approach of traditional Chinese medicine to assist treat brain glioma is feasible.
The twelve articles included in this study totaled 886 patients.The results of the meta-analysis showed that the curative effect of ITCWM in reducing tumor volume, gastrointestinal reactions, suppressing bone marrow,and prolonging short-term survival time was better than WM alone.Among them, it was more prominent in reducing tumor volume, gastrointestinal reactions, and suppressing bone marrow.After chemotherapy or radiotherapy, if there was a strong gastrointestinal adverse reaction and (or) bone marrow suppression, we can recommend ITCWM.However, there are many articles with heterogeneity in statistics of long-term survival (>3 years) and improvement of quality of life,and the reason for the greater heterogeneity may be related to the different effects of doctors using different Chinese medicine prescriptions, and this conjecture needs more follow-up cases to prove it.
There are still some limitations and deficiencies in this study: (1) The research articles only come from Chinese and English databases, which may have some publication bias; (2) Some of the included articles did not describe the randomization method and not mention the blind method, allocation and hiding, which would lead to bias and affected the credibility of the research results; (3) The schemes and doses of projects included are not consistent,which may draw impact on research results.(4)Because the prescriptions used are not uniform, there are differences in actual efficacy.
Concisely, according to the results of this meta-analysis, the ITCWM’s clinical efficacy in treating gliomas is better than WM alone, with greater life quality and a lower incidence of adverse reaction.However, in order to prove this conclusion,a larger standard sample project should be conducted.