Ocular biometric measurements and central corneal thickness in African pediatric population
2021-04-12MichaelineAsuquoIsawumi1BolanleVictoriaOlomolaAdedolapoOlaopa
Michaeline Asuquo Isawumi1, Bolanle Victoria Olomola, Adedolapo Olaopa
Abstract
INTRODUCTION
The cornea is one of the important refractive media in the eye and has a refractive index of -1.3765±0.0005[1]. It helps in refraction of light rays so as to focus images on retina. It is made up of about 2/3rdrefractive power of the eye with 43 dioptres. The thickness of cornea is known to vary between the center and towards the periphery. It also thins out at the periphery with age over 50 years[2]. However, the cornea also has some other clinically related changes whereby its thickness in the central part has been known to vary in various diseased conditions such as refractive error, glaucoma and also in age and race[3]. The thickness and measurement of the cornea is therefore very important in diseased conditions. This measurement is particularly important in recent times when relating to the diagnosis of glaucoma. For example, a thinner measurement of the central cornea is known to be a predictor of high risk for developing glaucoma[4]. While glaucoma patients have also been found to have thinner central cornea thickness[5]. High risk of glaucoma has been associated with thinner cornea of 555 μm and below which is associated with high intraocular pressure usually seen among African Americans. On the other hand, thicker cornea of greater than 588 μm is usually associated with low intraocular pressure which is usually found among Caucasians and Hispanics[6-7]. Some studies have found increased thickness in certain diseased cornea state or dystrophies[8]while others also found various thickness of cornea relating to different types refractive errors and wear of contact lenses[9]. Several studies have been carried out among adult Nigerians. For example, Iyamuetal[10]found that central corneal thickness(CCT) was thicker among normotensive subjects (551.6±44.5) μm, thinner among glaucomatous individuals (508.4±33.8) μm and thickest among the ocular hypertensives (604.5±14.4) μm while Babalolaetal[11]also reported that the mean CCT among Nigerians was (537.9 μm). This was of a higher value than in the African-Americans (521 μm) and lower than in the Caucasians (550.4 μm)[12]. The range of values for the CCT has not yet been known in the pediatric African population. This study was designed to find out the base line measurement of CCT in the pediatric African population as well as the relationship with other ocular biometric measurements. This will also allow for a reference data base and comparison with other populations across the world.
SUBJECTS AND METHODS
EthicalApprovalInformed consent was obtained from parents and guardians. Ethical approval was obtained from the Health Research and Ethical Committee of the College of Health Sciences, Osun State University.
StudySettingThe study was carried out in the State Specialist Hospital in Osogbo. Osogbo is the capital of Osun State which lies in the south western part of Nigeria. The people are of the Yoruba tribe and are mainly made up of agrarian communities. This was an observational clinic-based study of a cross-section of children aged 3 years and above seen consecutively between November 2017 and January 2018.
SampleSizeandSamplingA purposive sampling technique was used in which the participants were enrolled consecutively. All patients seen between this period of study were included in the study. However, children less than 3 years, those with congenital glaucoma, any diseased cornea with opacity or dystrophy, micro corneas, and children with lens opacities and any other ocular pathology were excluded from the study. Patients’ age and gender were obtained from the parents or guardians. Visual acuity (VA) was assessed with LogMAR charts and Lea charts according to age group. Examination under anesthesia (EUA) using oral chloral hydrate was carried out in the clinic for uncooperative children who were eight years and below. Anterior segments were examined using pen light. Heine hand-held slit lamp was used to examine children who would not cooperate with the table-top slit lamp under anaesthesia. The posterior segments were examined using Heine binocular indirect ophthalmoscope through dilated pupils. Pupils were dilated using Apamide plus eye drops (contains Phenylepherine and Tropicamide made by Appassamy and Associates, India). Corneal diameters (CD) were measured using calipers after lid retraction gently by hand. Results were recorded in millimeters. Any corneal diameter with measurements less than 10 mm was considered small while any measurement greater than 12 mm was considered to be a large cornea. Any associated cases of abnormality except refractive error were not included in the study. CCT was measured using the ultrasonic pachymeter, Pacchette 3 model. The cornea was anaesthesised topically with 2% xylocaine before applying the probe within the central 3 mm of the cornea. The units of measurements were recorded in micro meter (μm). The CCT values were then recorded 2 times and the average value was taken. The axial length measurement was also recorded likewise from the pachette 3 pachymeter. Intraocular pressures were measured among the cooperative patients and under anaesthesia among uncooperative patients using Perkins hand held tonometer. Note that the intraocular pressure is usually close to normal with the use of oral chloral hydrate[13]. The measurements were recorded in millimeters of mercury (mmHg). The normal intraocular pressure is usually taken to be between 10-21 mmHg. Cycloplegic refraction under anaesthesia was carried out on uncooperative children 8 years and below using Keeler’s streak retinoscope from a distance of 66 cm. For cooperative children, refraction was carried out without anaesthesia. The subjective results were then determined and juxtaposed using the principles of guidelines of prescribing glasses according to the American Academy of Ophthalmology which also describes refractive error according to age and degree of error. This was used to classify whether refractive errors were normal for age or not and if significant or not.
StatisticalAnalysisData were entered into and analyzed using Statistical Package for Social Science (SPSS Inc., Chicago, IL) software version 17.0 to generate results through descriptive statistics. Frequencies, means, standard deviation and cross tabulations of variables were done.Pvalue ≤0.05 was considered significant. Correlation analysis was done to compare associations of CCT with other variables using minimum of 0 and maximum of 1 and grouped into 0-0.25 as poor correlation, 0.25-0.49 as weak correlation, 0.5-0.749 as fair correlation and 0.75-1 and strong correlation. Independent samplet-test was done to compare means between males and females with a significant level ofP≤0.05. Analysis of variance (Anova) was also done for comparison of CCT among different age groups.
RESULTS
Sixty-six children and 132 eyes were seen. Male with female ratio was 1∶1.7. Their ages ranged between 3-16 (mean 9.13±3.70) years. The modal age range was 6-10±0.7 years (42.4%). Most of them were primary school students 36 (54.5%). The predominant parents’ occupation were traders 34 (51.6%) and civil servants (30.3%). The mean right VA was 0.45±0.46 and left VA 0.45±0.44 (Table 1).
The mean right and left horizontal CD (HCD) were 10.5±1.6 mm and 10.37±1.45 mm respectively. The mean right and left vertical CD (VCD) were 9.7±1.2 mm and 9.7±1.3 mm respectively. The mean right and left CCT were (556.71±2.61) μm and (556.47±45.53) μm respectively. Myopia 23 (34.8%), myopic astigmatism 18 (27.3%) and simple astigmatism 16 (24.2%) were the commonest types of refractive error. The mean values of CCT, IOP, and VCD ratios are shown in Table 2.
Bivariate analysis showed no significant associations between the CCT and HCD (P=0.739), CCT and right VA (P=0.058) as well as CCT and refractive error (P=0.199). The mean CCT is 553.27±43.02 μm. Correlation between the age groups and CCT showed, right is 3.032 andP=0.055. The CCT cross tabulated according to the age group shows that the 501-550 μm and 551-600 μm groups have the most frequent distribution (P=0.056) (Table 3). CCT and the types of refractive error showed more children having myopia, astigmatism and myopic astigmatism in the range of 501-600 μm (Table 4).
There was a fair positive correlation (0.989) between the CCT and refractive error and weak positive correlation (0.695) of CCT with horizontal corneal diameter (Table 5). The means of the variables were compared between boys and girls (Table 6). The right eye results were used as reference data.

Table 1 Frequencies of variables (n=66)

Table 2 Statistics showing variables, mean and standard deviation from SPSS Vs.17
DISCUSSION
This study was conducted among 3-16 (mean range: 9.13±3.70) years old school children. This was similarly to the PEDIG study with the mean age of 8.7 years[14]. In a study of corneal profile among Chinese children, the age range was 7-15 years[15]. There was no comparison of the CCT values with parents’ occupation in this study. The mean CCT in this study (556.71 μm) among children was similar to those found in the Afro Americans of 551 micrometers, which was below the values of the White- Hispanic of 573 μm among subjects 12-
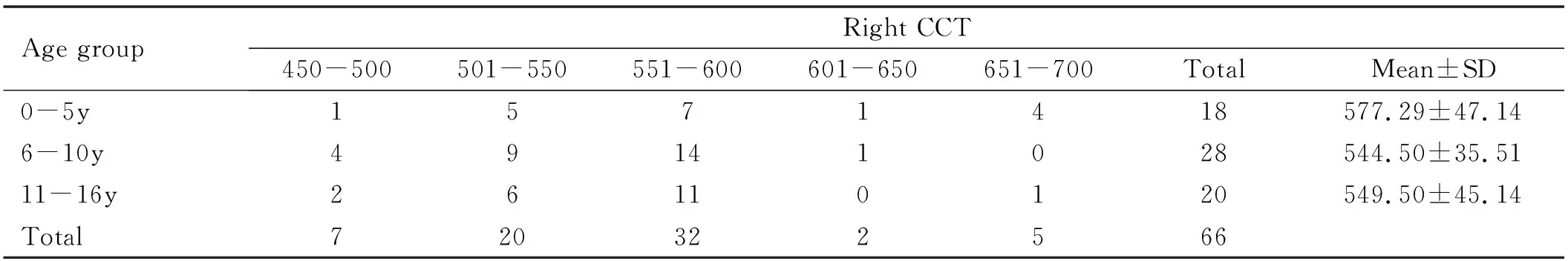
Table 3 Age versus right central corneal thickness and their mean standard deviation

Table 4 Central corneal thickness versus types of refractive error(n, %)

Table 5 Correlations of CCT with right horizontal corneal diameter, visual acuity and refractive error and CCT

Table 6 Group statistics for means of males and females
17 years of age[14]. In another similar hospital based study, in Yuzuncu Yil University, Turkey, 555 μm was seen among 11-12 years, with a mean of 556±3.4 μm[16]. The average CCT found among the Chinese children was 532.70±28.45 μm for left eyes and 532.96±28.33 μm for right eyes[14]. The CCT was seen to slightly increase with age group 6-10 years and later tended to stabilize from 11-16 years. There was a correlation showed between CCT and age in our study (P=0.056) (Table 3). This was similarly noticed where there was a successive increase yearly between ages 1-11 years in the PEDIG study[12]. The CCT was however found to be a bit more stable between ages 12-17 years[12]. Other workers also found similar results in America and Iran[17-18].
The CCT had no significant association with refractive error in this study, similar to findings by Daietal[17]. The Iranian study which was a large population study comparatively found association between the CCT with younger age and female gender and no correlation with anterior chamber depth and corneal curvature[16]. It was also noticed that most children with astigmatism and myopia fell among the category of 500-550 μm and 551-560 μm CCT. The significant association with CCT was however more frequently recorded among the myopic and hyperopic astigmatic Chinese children[19].
The corneal diameter (CD) was not significantly associated with the CCT in this study (P=0.739). However, the mean corneal diameters in this study, [right and left HCD were 10.5±1.6 mm and 10.37+1.45 mm respectively while the mean right & left VCD were 9.7±1.2 mm and 9.7±1.3 mm] were comparatively lower than those found in Saudi Arabia with values of 11.68±0.41 mm using the caliper measurement[20]. In a study carried out by Olatunjietal[21]in Ilorin among new borns, the mean vertical and horizontal corneal diameters were found to be 9.87±0.04 mm for horizontal and 9.62±0.41 mm for vertical respectively. These results appear very similar to our findings especially in relation to the values of the vertical diameters with a little difference of 0.5-0.6 mm for the horizontal axes. This could be because a new born is younger than our study participants that are older in age and so has smaller CD. Corneal diameters are also known to become enlarged in glaucomatous conditions.
The mean IOPs for the right and left eyes were 15.95 mmHg and 14.25 mmHg with no significant association with CCT. This was similar to the mean IOP values of 15.31±2.57 mmHg reported by Weietal[22]. Comparatively, among Palestinian children aged 7-15 years, the mean IOPs for the right and left eyes were of lower values of 12.5±2.2 mmHg and 12.3±2.2 mmHg respectively and no significant differences were observed in relation to age or gender between CCT and IOP[23]. Another comprehensive Meta-analysis carried out among healthy Iranian children showed that the mean IOP in all races was 16.22 mmHg (95%CI: 15.48-16.97) while the highest measurement of 17.38 mmHg (95%CI: 15.77-18.98) was found in black children with Indians recording the lowest IOP of 12.02 mmHg (95%CI: 11.40-12.64)[3]. These probably suggest that intraocular pressure measurement may vary with race, ethnicity and age. A positive correlation of increasing IOP with 100 μm in CCT was also noticed among the Malay children aged 8-16 years[24]. The mean axial length (AL) recorded in this study was 22.10 mm. This was similar to the findings in Turkey where between the age groups 3 to more than 12 years with 2 years interval, the AL (mm) measurements were between 20.49-22.95 (mean range: 22.02) mm which is very close to our findings[16].

Limitations of study: this study had a small sample size which could affect the power of the study. It was also a hospital-based study which means that the result is only a reflection of those that presented to the hospital. The strength of the study lies in the fact that it is a specialized study which can only be carried out in a specialist center and therefore could suggest a true estimate of the values.