Pain and function deteriorate in patients awaiting total joint arthroplasty that has been postponed due to the COVID-19 pandemic
2021-04-02JurekRafalTomaszPietrzakZiaMaharajMagdalenaErasmusNkhodiseniSikhauliJosipNenadCakicLipaloMokete
Jurek Rafal Tomasz Pietrzak,Zia Maharaj,Magdalena Erasmus,Nkhodiseni Sikhauli,Josip Nenad Cakic,Lipalo Mokete
Jurek Rafal Tomasz Pietrzak,Department of Orthopaedics,University of the Witwatersrand,Johannesburg 2193,Gauteng,South Africa
Zia Maharaj,Magdalena Erasmus,Nkhodiseni Sikhauli,Lipalo Mokete,Department of Orthopaedic Surgery,Charlotte Maxeke Johannesburg Academic Hospital,Johannesburg 2193,Gauteng,South Africa
Josip Nenad Cakic,Department of Orthopaedic Surgery,Life Fourways,Johannesburg 2193,Gauteng,South Africa
Abstract BACKGROUND Elective total joint arthroplasty (TJA) procedures have been postponed as part of the coronavirus disease 2019 (COVID-19) response to avert healthcare system collapse.Total hip arthroplasty (THA) and total knee arthroplasty (TKA)procedures comprise the highest volume of elective procedures performed at health care facilities worldwide.AIM To determine the demand for TJA despite the pandemic and the impact of surgery postponement on physical and mental health.METHODS We conducted a prospective cross-sectional telephonic interview-based study on patients awaiting THA and TKA at an academic institution in South Africa.The questionnaire consisted of four sections.The first section recorded baseline demographic data and medical co-morbidities,the length of time spent awaiting TJA,and the patients’ desire to undergo elective surgery despite the COVID-19 pandemic.Section 2 and Section 3 assessed the patients’ current physical and mental health,respectively,as a consequence of deferred surgical intervention.The last section established the patients’ perception of the healthcare system’s response to the COVID-19 pandemic and necessity to postpone elective surgery.Patients received counseling and education on the current state of surgery during the COVID-19 pandemic and associated risks.Thereafter,patients were once again asked about their desire to undergo TJA during the COVID-19 pandemic.RESULTS We included 185 patients (65.95% female;mean age:50.28 years) awaiting TJA for a mean of 26.42 ± 30.1 mo.Overall,88.65% of patients wanted TJA despite the COVID-19 pandemic.Patients awaiting TJA for 1-3 years were 3.3-fold more likely to want surgery than those waiting < 1 year (P < 0.000).Patients with comorbidities were 8.4-fold less likely to want TJA than those with no comorbidities (P = 0.013).After receiving education,the patients wanting TJA decreased to 54.05%.Patients who changed their opinion after education had less insight on the increased morbidity (P = 0.046) and mortality (P = 0.001) associated with COVID-19.Despite awaiting TJA for shorter period (24.7 ± 20.38 mo),patients who continued to demand TJA had greater pain (P < 0.000) and decreased function (P = 0.043) since TJA postponement.CONCLUSION There is deterioration in health for patients,who have had elective procedures postponed during the COVID-19 pandemic.Waiting lists should be prioritized for urgency with the re-initiation of elective surgery.
Key Words:Total hip arthroplasty;Total knee arthroplasty;Elective surgery;COVID-19;Waiting lists;Primary total joint arthroplasty
INTRODUCTION
The infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 virus (coronavirus disease 2019 [COVID-19]) was declared an international pandemic by the World Health Organization in March 2020[1-3].In response,a moratorium was declared on the performance of elective surgery in many countries to avert healthcare system collapse,preserve equipment,and maintain resources and hospital capacity[4-8].Approximately 28 million elective operations were cancelled or postponed worldwide during the peak 12 wk of this global pandemic[7,8].Total hip arthroplasty (THA) and total knee arthroplasty (TKA) procedures comprise the highest volume of elective procedures performed at health care facilities worldwide[4,8].A survey of the European Hip Society and the European Knee Associates from 40 different countries reported a near total shutdown of total joint arthroplasty (TJA) with 92.6% of primary TJA procedures being cancelled[7].The demand for TJA is already high and waiting lists continue to rise with approximately 150000 elective procedures performed per month in the United States cancelled at some time due to the COVID-19 response[3,7,8].The prolonged postponement of elective TJA has had devastating economic implications on the healthcare system.It is estimated that the process of re-initiation of elective procedures following the COVID-19 pandemic in developing countries would result in an approximate loss of $700 billion[9].
In addition to the growing economic burden,patients awaiting surgery for more than 180 d have demonstrated increased risks for poor outcomes after TJA[10,11].Patients with hip and knee osteoarthritis on extended waiting lists for surgery deteriorate with time on the pain and physical function on the Western Ontario McMasters Universities Osteoarthritis index scores and joint-specific Oxford scores[10,11].Poor pre-operative baseline function is also associated with worse pain and functional outcomes up to 24 mo after TJA[10-12].
The aim of this study was to gain insight into patient perceptions in the setting of a waiting list for TJA at an academic institution in the COVID-19 era.Through a questionnaire-based telephone interview,we assessed patient demand for elective TJA and evaluated the impact of the postponement of TJA on function and mental health.Lastly,we assessed the effect of purposeful patient education and counseling about the reasoning behind postponement of elective surgery on patient demand for TJA[13].
MATERIALS AND METHODS
We conducted a prospective cross-sectional telephonic interview-based study of 227 patients awaiting TJA at a single,referral academic institution in Johannesburg,South Africa during the COVID-19.There were 118 patients and 109 patients planned for elective primary TKA and THA respectively,during this time who had their surgery postponed.Patients requiring emergency surgery for hip fractures,periprosthetic fractures,joint dislocation,or periprosthetic joint infections were excluded.Institutional review board ethics approval was obtained (M190528) before commencement of the study.Contact information was obtained for all patients from the institution’s TJA waiting list.This waiting list generally operates on a first-in firstout basis with exceptions for cases that are deemed clinically urgent.The list has been used to capture data of patients who qualify for and consent to TJA.It is used to plan and prepare surgical lists and has been operational since 2004.
Interviews were conducted from 20 June to 10 July 2020,a full 6 wk after all elective surgery in both private and public hospitals in South Africa had been cancelled in response to the global COVID-19 pandemic as mandated by the South African Disaster Management Act.At the time of initiation of patient interviews,our institution had already made the decision to only revisit resumption of elective procedures after the 1stof October 2020,a period of 32 wk.Interviews were all conducted telephonically by two post-graduate orthopedic surgery students,and all interviews were recorded.The interviewers were fluent in all major South African language groups and all patients were,to the extent possible,interviewed in their first language.A single,standardized and structured questionnaire was used for all interviews,and all interviews were recorded.Patients were given the option to provide verbal voluntary consent or refusal to participate in the study after being informed of its purpose.The questionnaire consisted of four sections.
The first section recorded baseline demographic data including age,gender and medical co-morbidities including heart disease,diabetes mellitus and human immunodeficiency virus infection.The time that each patient had spent waiting for elective,primary TJA was calculated from the date the patient was first added to the waiting list until the date of suspension of all elective surgery lists,20 March 2020.Lastly,we ascertained the patients desire to undergo elective TJA procedures despite the COVID-19 pandemic.
Section 2 assessed the patients current disease state as a consequence of the deferred surgical intervention.A 5-point Likert scale was used to determine the degree to which the patient felt the postponement of surgery had affected their pain,numerical rating scale (NRS) pain score,functionality and need for analgesia.Section 3 was an evaluation of mental health.Depressive symptoms including weight gain and loneliness were recorded.A 5-point Likert scale was used to evaluate the patients’anxiety regarding TJA during the COVID-19 pandemic.
Section 4 endeavored to establish the patients’ perception of the healthcare system’s response to the COVID-19 pandemic and necessity to postpone elective surgery.We assessed patients’ knowledge of basic coronavirus transmission prevention measures such as the wearing of face masks,general hand hygiene,and social distancing.We attempted to assess the extent of insight that patients had regarding the response of the healthcare system to the COVID-19 pandemic.This included the patient’s knowledge of infection control procedures that have been implemented to minimize disease spread.Thereafter,patients were counseled regarding the current state of surgery during the COVID-19 pandemic.Patients were educated on the introduction of routine testing for COVID-19 prior to admission and preclusion of visitors during their hospital stay.Patients were then counseled with respect to poor clinical outcomes in COVID-19 infected patients undergoing surgery including the possibility of death and the risk of contracting COVID-19 as an inpatient.Upon conclusion of this patient education patients were once again asked about their desire to undergo TJA during the COVID-19 pandemic.
Results were tabulated with mean and standard deviation calculated for integer variables.Chi-squared testing was used to compare relationships between categorical variables.Patient age and period awaiting TJA were categorized and responses were compared across sub-groups.Additional categorical variables that responses were compared across included comorbidities and demand for TJA despite COVID-19 pandemic both before and after patient education and counseling.Odds ratios (ORs)were calculated using logistics regression for binary outcomes.Statistical significance was set atP< 0.05.The statistical software used for analysis wasR4.0.2 for Windows Copyright (C) 1989,1991 Free Software Foundation,Inc with interfaceRStudio Version 1.3.959.
RESULTS
Sample population and demographic data
There were 185 patients (81.5%) included in the study (Figure 1).The mean age was 50.28 years (range:33-69) with 122 female patients (65.95%).There were 106 (57.3%)patients awaiting surgery for TKA and 79 (42.7%) for THA,respectively.The overall mean length of time for patients awaiting TJA was 26.42 mo (standard deviation [SD]:30.1;range:3-264 mo).The mean length of time for patients awaiting THA was 28.29 mo (SD:34.87;range:3-264 mo) and TKA was 25.03 mo (SD:26.07;range:4-200 mo),respectively.There were 126 patients (68.11%) with one or more comorbidities.Additional demographic details and results for the questionnaire are depicted in Table 1.
Patient demand for TJA
There were 164 patients (88.65%) who wished to undergo TJA and 21 patients (11.35%)that did not want elective TJA,respectively at the earliest opportunity despite the COVID-19 pandemic.Patients awaiting TJA for more than 3 years were 4.3-fold more likely to want surgery compared to those awaiting surgery for less than 1 year (OR > 3 years 6.15;< 1 year 1.41;P= 0.029).Patients awaiting TJA between 1 and 3 years were 3.3-fold more likely to want surgery compared to those awaiting surgery for less than 1 year (OR:1-3 years 4.71;< 1 year 1.41;P< 0.000).Patients with more than one comorbidity were 8.4-fold less likely to want elective surgery during the pandemic compared to those with no comorbid conditions (OR > 1 comorbidity 0.24;no comorbidities 3.38;P= 0.013).
Pain and function since the postponement of surgery
There was increased joint pain experienced by 101 patients (55.49%) since the postponement of their TJA.The responses for pain and function were compared between patients that wanted TJA despite the COVID-19 pandemic to those who did not want surgery at the earliest opportunity (Table 2).Increased joint pain was experienced by 58.28% (n= 95) of patients that wanted TJA despite the COVID-19 pandemic compared to 31.58% (n= 6) of patients that did not want elective surgery at the earliest opportunity (P= 0.037).The mean NRS pain score overall was 7.37 (SD:2.24;range:0-10).
There were 123 patients (67.21%) who felt their functionality due to joint pain had decreased since the postponement of surgery.There were 73 (78.5%) patients between the age of 45 to 60 years who had decreased functionality since the postponement of surgery compared to 25 (46.3%) and 24 (68.6%) patients under 45 years and over 60 years of age,respectively (P= 0.015).There was decreased function for patients that wanted TJA compared to those who did not,demonstrated by significant differences in decreased functionality due to joint pain (70.99%vs38.1%;P= 0.002) and decreased walking distance (50.3%vs28.58%;P= 0.034) respectively.
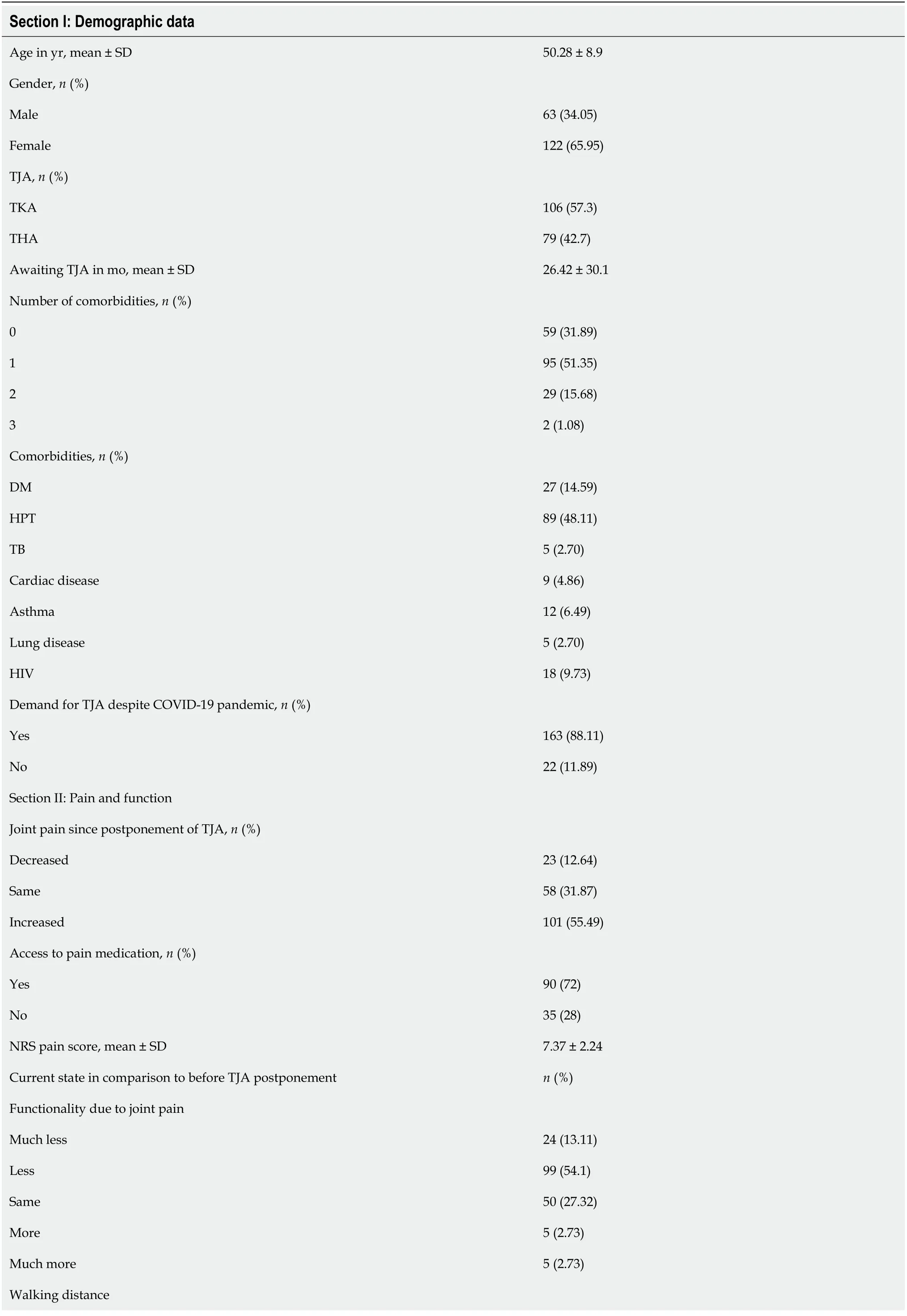
Table 1 Coronavirus disease 2019 arthroplasty waiting list questionnaire response results
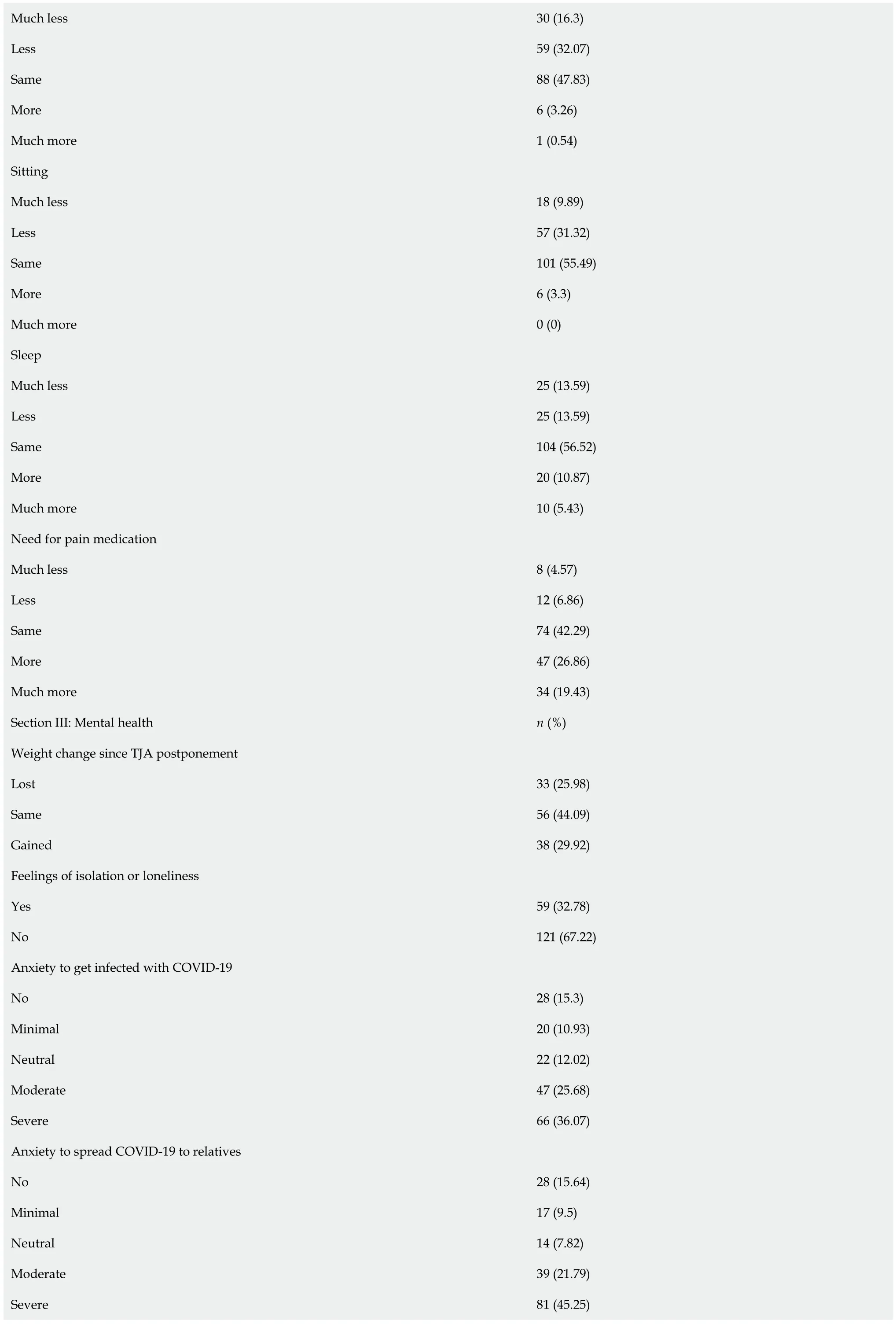
Much less 30 (16.3)Less 59 (32.07)Same 88 (47.83)More 6 (3.26)Much more 1 (0.54)Sitting Much less 18 (9.89)Less 57 (31.32)Same 101 (55.49)More 6 (3.3)Much more 0 (0)Sleep Much less 25 (13.59)Less 25 (13.59)Same 104 (56.52)More 20 (10.87)Much more 10 (5.43)Need for pain medication Much less 8 (4.57)Less 12 (6.86)Same 74 (42.29)More 47 (26.86)Much more 34 (19.43)Section III:Mental health n (%)Weight change since TJA postponement Lost 33 (25.98)Same 56 (44.09)Gained 38 (29.92)Feelings of isolation or loneliness Yes 59 (32.78)No 121 (67.22)Anxiety to get infected with COVID-19 No 28 (15.3)Minimal 20 (10.93)Neutral 22 (12.02)Moderate 47 (25.68)Severe 66 (36.07)Anxiety to spread COVID-19 to relatives No 28 (15.64)Minimal 17 (9.5)Neutral 14 (7.82)Moderate 39 (21.79)Severe 81 (45.25)
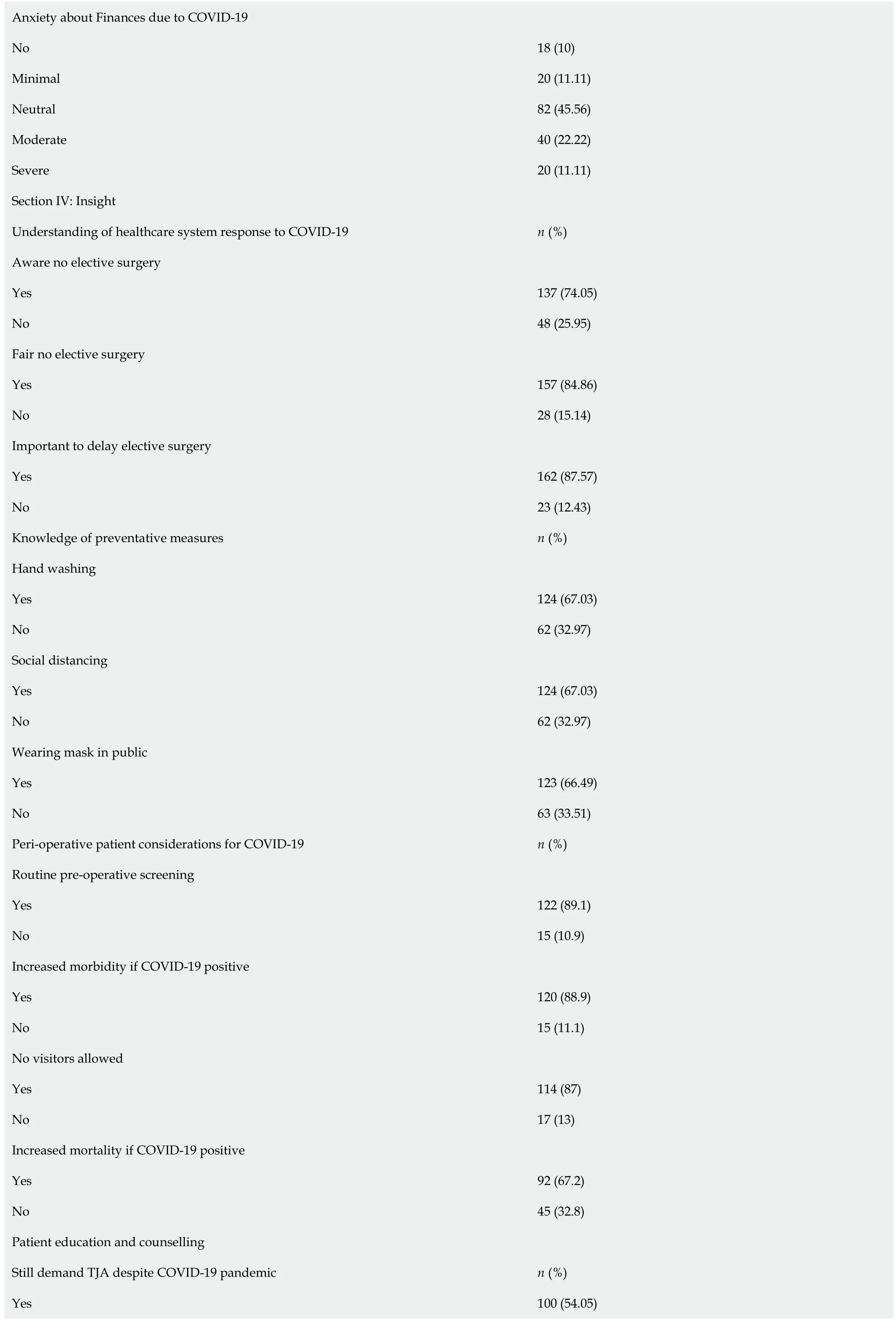
Anxiety about Finances due to COVID-19 No 18 (10)Minimal 20 (11.11)Neutral 82 (45.56)Moderate 40 (22.22)Severe 20 (11.11)Section IV:Insight Understanding of healthcare system response to COVID-19 n (%)Aware no elective surgery Yes 137 (74.05)No 48 (25.95)Fair no elective surgery Yes 157 (84.86)No 28 (15.14)Important to delay elective surgery Yes 162 (87.57)No 23 (12.43)Knowledge of preventative measures n (%)Hand washing Yes 124 (67.03)No 62 (32.97)Social distancing Yes 124 (67.03)No 62 (32.97)Wearing mask in public Yes 123 (66.49)No 63 (33.51)Peri-operative patient considerations for COVID-19 n (%)Routine pre-operative screening Yes 122 (89.1)No 15 (10.9)Increased morbidity if COVID-19 positive Yes 120 (88.9)No 15 (11.1)No visitors allowed Yes 114 (87)No 17 (13)Increased mortality if COVID-19 positive Yes 92 (67.2)No 45 (32.8)Patient education and counselling Still demand TJA despite COVID-19 pandemic n (%)Yes 100 (54.05)
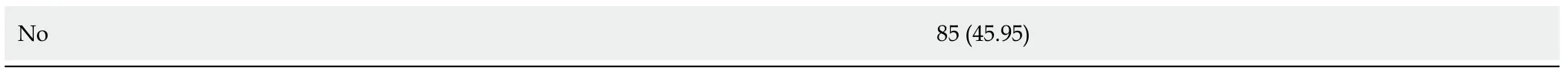
COVID-19:Coronavirus disease 2019;DM:Diabetes mellitus;HIV:Human immunodeficiency virus;HPT:Hypertension;NRS:Numerical rating scale;SD:Standard deviation;TB:Tuberculosis;THA:Total hip arthroplasty;TJA:Total joint arthroplasty;TKA:Total knee arthroplasty.
Mental health during the COVID-19 pandemic
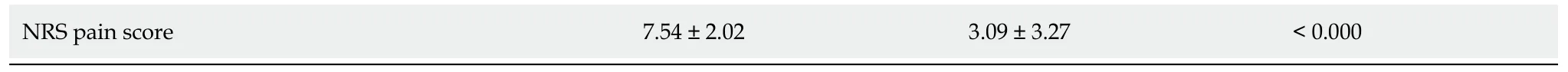
There were 113 patients (61.75%),who experienced increased anxiety about getting infected with COVID-19 should they get their elective TJA during this time.There were 120 patients (67.04%) who experienced increased anxiety about subsequently spreading COVID-19 to relatives.The responses for mental health were compared between patients that wanted TJA despite the COVID-19 pandemic to those who did not want surgery at the earliest opportunity (Table 3).The increased anxiety of getting infected with COVID-19 was found in 64.19% (n= 104) of patients who wanted TJA compared to 42.86% (n= 9) of patients that did not want surgery at the earliest opportunity (P= 0.013).Similarly,there was increased anxiety to spread COVID-19 to relatives for 110 patients (69.62%) that wanted TJA and 10 patients (47.62%) that did not want elective surgery,respectively (P= 0.016).There were no significant differences between patients when compared between age groups and presence of comorbidities.
Patient insight and impact of patient education
There were 162 patients (87.57%) that accepted the reasoning behind the delay of elective surgery in response to the COVID-19 pandemic.The detailed results for the assessment of patient insight are depicted in Table 1.After receiving patient education there were 100 patients (54.05%) that still wanted TJA despite the COVID-19 pandemic and 85 patients (45.95%) that did not want elective surgery at the earliest opportunity(Figure 2).Over half the patients (100 patients/54.05%) wanted TJA despite the COVID-19 pandemic (continued demand group) after counseling.There were 21 patients (11.35%) that opted out of surgery as the earliest opportunity despite COVID-19 (defer group) both before and after patient education.There were 64 patients(34.59%) that changed their opinion after receiving patient education (receptive group).
The receptive group previously wanted TJA despite the COVID-19 pandemic and subsequently opted out of elective surgery after receiving patient education.The results for questions regarding patient insight were compared between the continued demand group,the defer group and the receptive group (Table 3).The importance to delay elective surgery was recognized 81.97% of the receptive group compared to 91.4% and 100% of the continued demand and defer groups,respectively (P< 0.000).Similarly,76.67% of the receptive group were aware of the increased risks associated with COVID-19 if infected peri-operatively,compared to 91.75% and 100% of patients from the continued demand and defer groups,respectively (P= 0.046).There were 44 patients (73.33%) from the receptive group that understood there would be no visitors allowed to see them in hospital after surgery compared to 85 (91.75%) and 20 (95.24%)patients from the continued demand and defer groups,respectively (P= 0.018).Lastly,43.33% of the receptive group were aware of the increased risks for death associated with COVID-19 compared to 77% and 85.71% of patients from the continued demand and defer groups,respectively (P= 0.001).
Continued demand for TJA despite the COVID-19 pandemic
The patient characteristics and perception of pain and function since the postponement of TJA was of interest regarding the continued demand group.The results for questions regarding pain and function were compared between the continued demand group,the defer group and the receptive group (Tables 4 and 5).Patients in the continued demand group were awaiting TJA for a mean period of 24.7 mo (SD:20.38,range:3-132 mo).The mean length of time for patients awaiting TJA in the Defer group was 25.32 mo (SD:40.54,range:4-200 mo) and in the receptive group was 28.91 mo (SD:37.82,range:4-264 mo),respectively.Increased joint pain was experienced by 60.61% of the continued demand group compared to 33.33% and 53.12% of defer and receptive groups,respectively (P= 0.035).The mean NRS pain score for the continued demand group was 7.68 (SD:2.14;range:2-10) compared to 5.9 (SD:3.2;range:0-10)and 7.24 (SD:1.8;range:2-10) for defer and receptive groups,respectively (P< 0.000).There was decreased functionality due to joint pain for 75.51% of the continued demand group since the postponement of surgery compared to 50% and 60.94% of patients in the defer and receptive groups,respectively (P= 0.043).
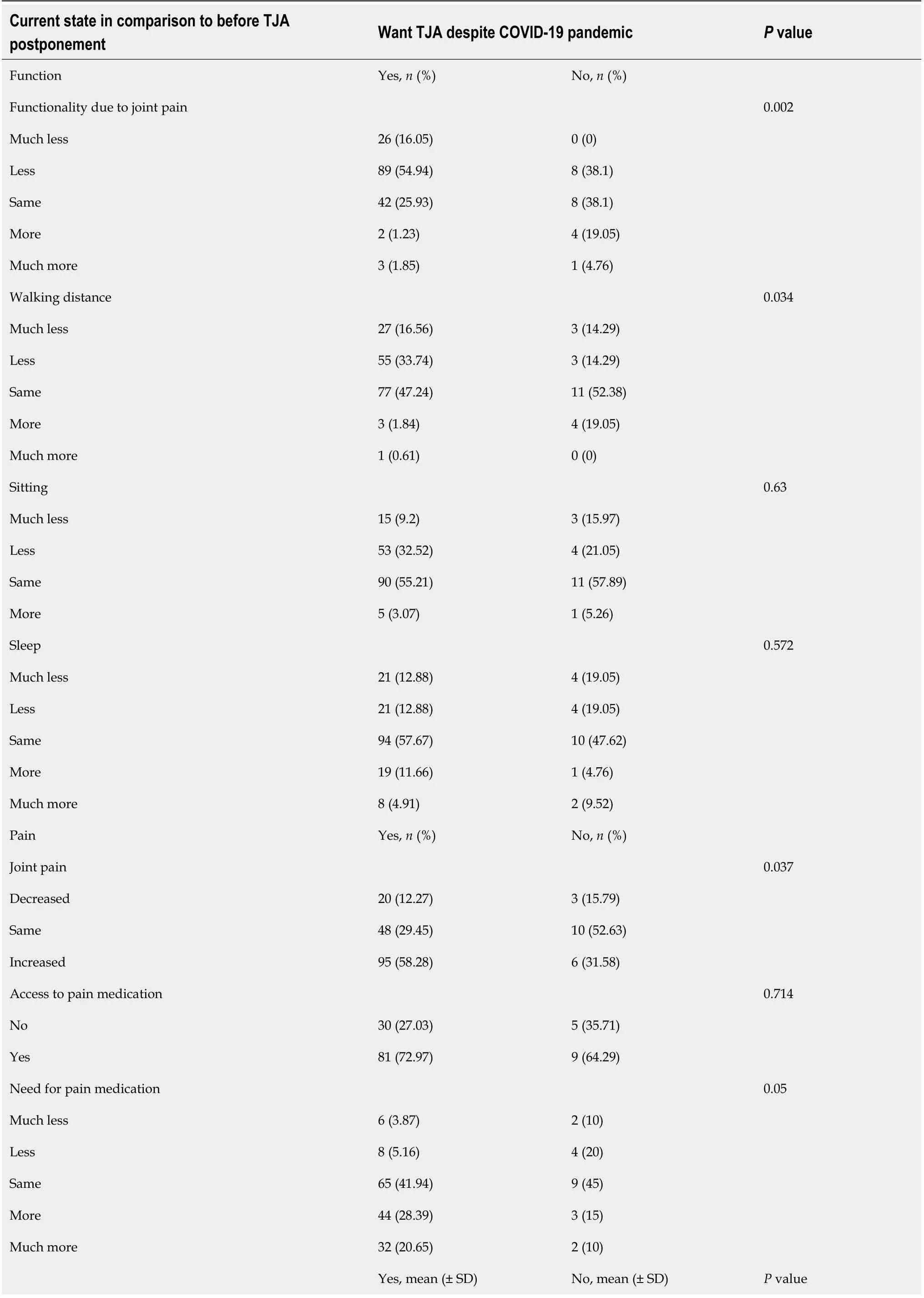
Table 2 Pain and function responses compared between patients that wanted total joint arthroplasty despite the coronavirus disease 2019 pandemic (Yes) to patients that did not want elective surgery as soon as possible (No)1
1Yes (n = 164);No (n = 21).COVID-19:Coronavirus disease 2019;NRS:Numerical rating scale;SD:Standard deviation;TJA:Total joint arthroplasty.
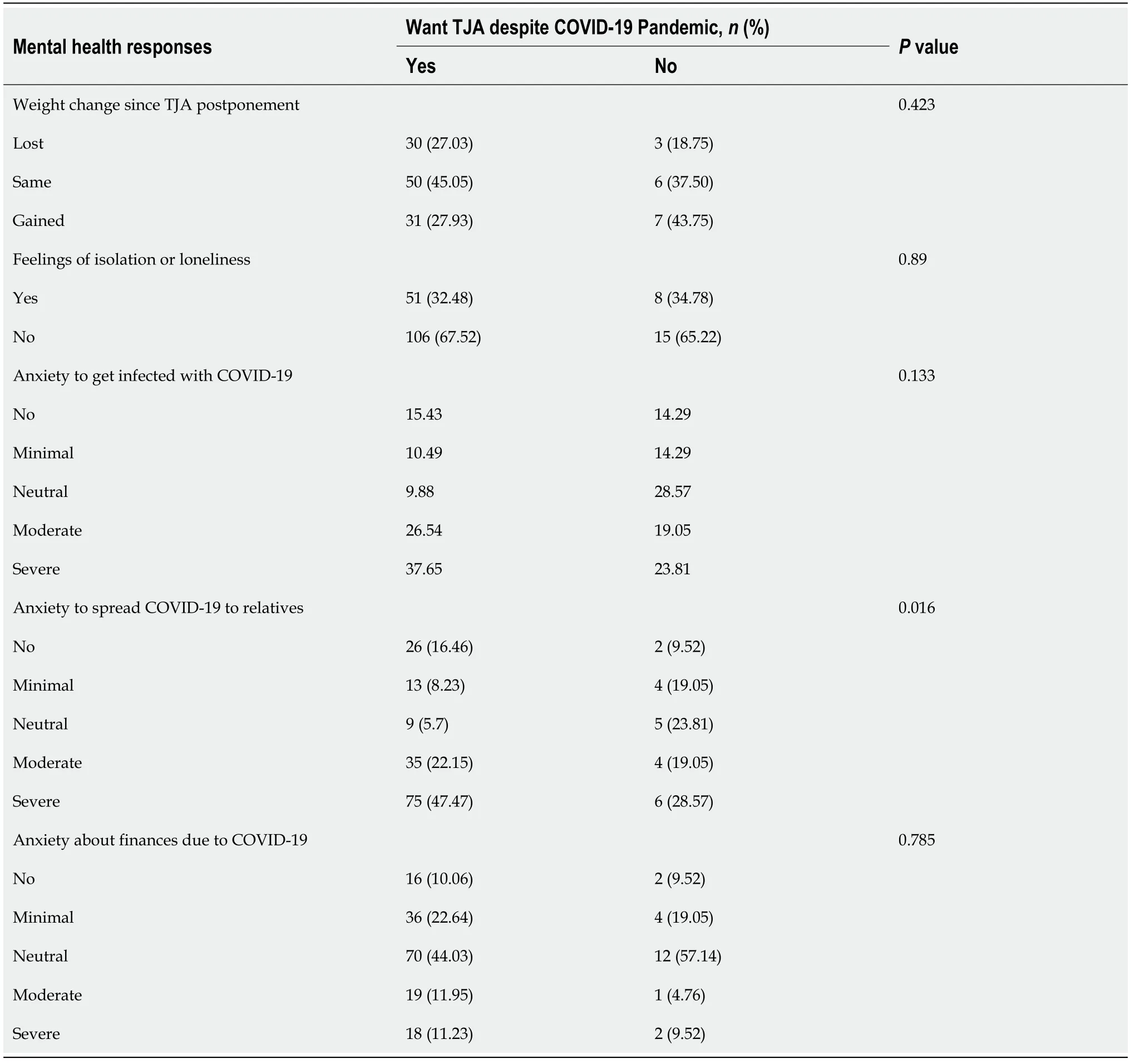
Table 3 Mental health responses compared between patients that wanted total joint arthroplasty despite the coronavirus disease 2019 pandemic (Yes) to patients that did not want elective surgery as soon as possible (No)1
DISCUSSION
In our study,88.65% of patients awaiting TJA wanted elective surgery as soon as possible despite the current COVID-19 pandemic.Similarly,a study by Brownet al[14]in the united states demonstrated that almost 90% of patients wanted to reschedule elective TJA as soon as possible.A study conducted in the United Kingdom found that only 56.8% of patients for TJA wanted their elective surgery as soon as possible[15].Additionally,Brownet al[14]reported that 85% of patients agreed with the decision to cancel elective surgery in response to the COVID-19 pandemic in the united states.This is reflected in our study of a sub-Saharan Africa population with 87.57% of patients accepting the need to delay elective TJA procedures.There is a demonstrated need to postpone elective surgery,particularly in high-risk patients and re-initiation should be careful and gradual.
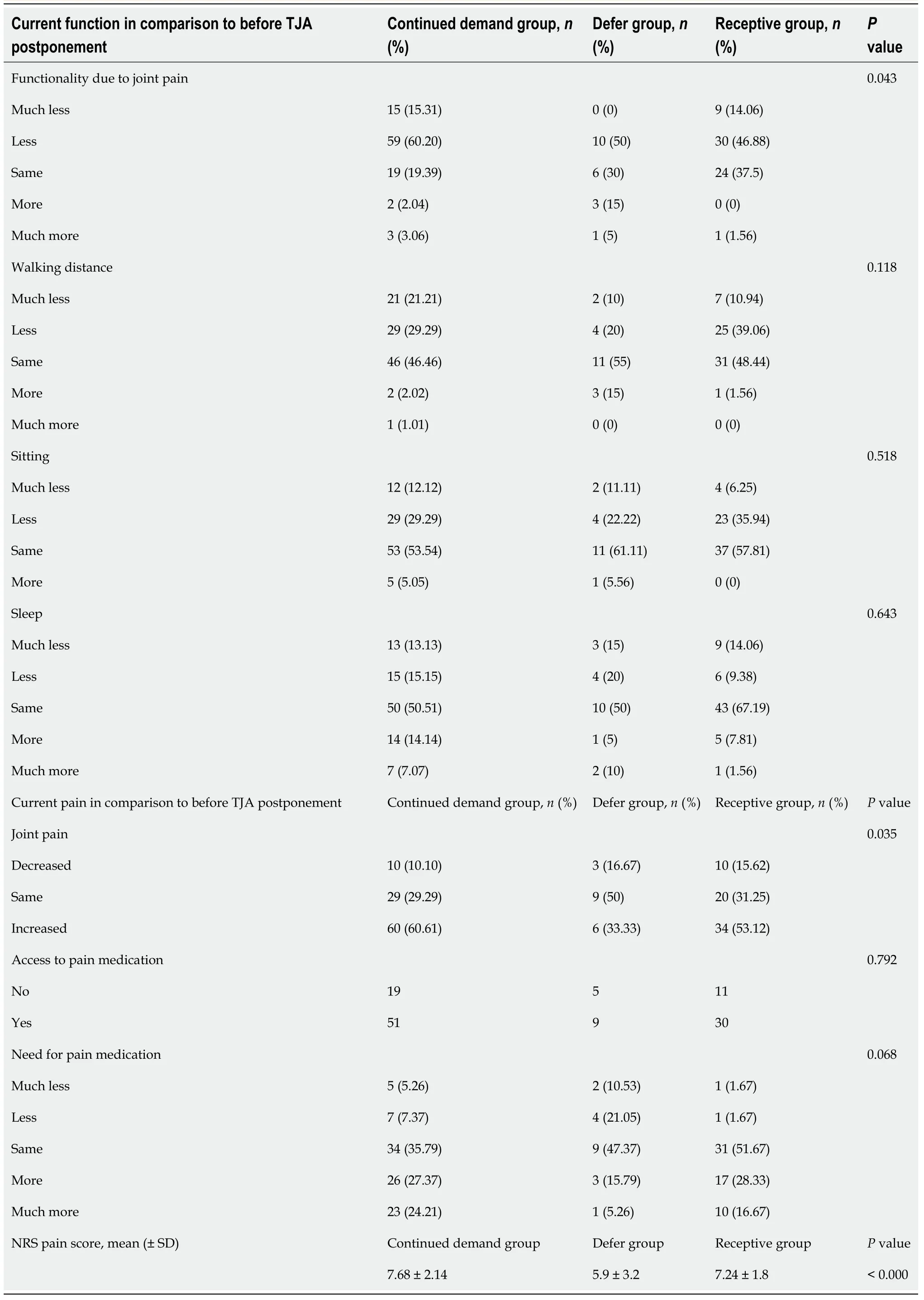
Table 4 Pain and function responses compared between the continued demand group,defer group and receptive group1

Table 5 Responses for Insight Perception Regarding coronavirus disease 2019 compared between the continued demand group,defer group and receptive group1
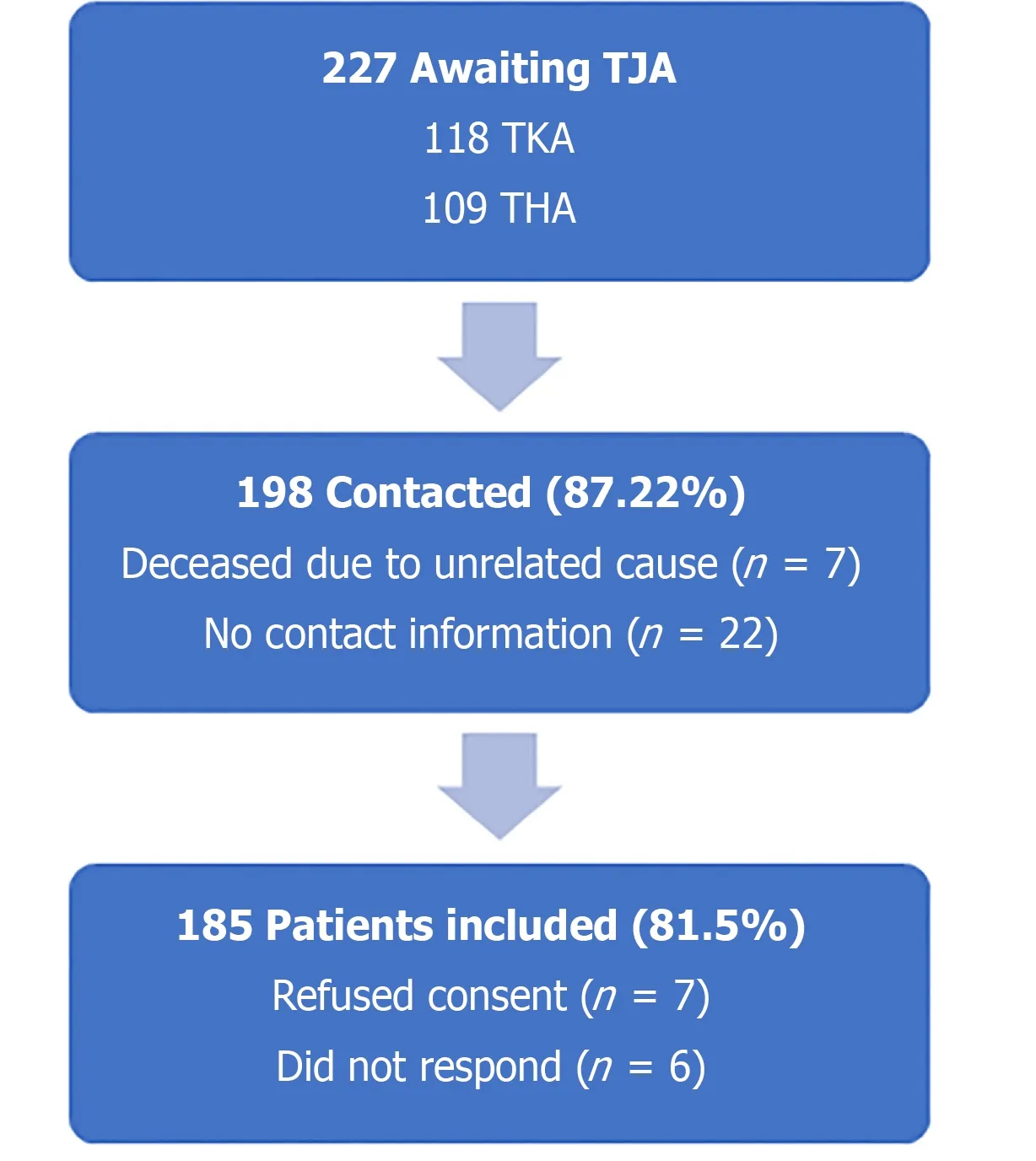
Figure 1 Flowchart of the study cohort.
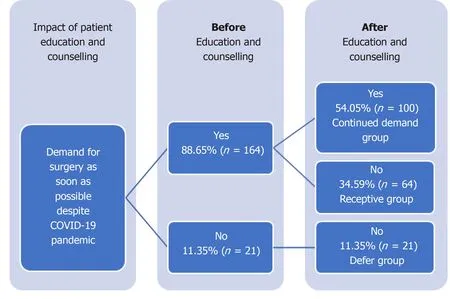
Figure 2 Patient demand for total joint arthroplasty before and after receiving education and counseling.
Patients with comorbidities,particularly those with cardiac diseases,hypertension and diabetes mellitus,have increased risks for morbidity and mortality if infected with COVID-19[16,17].In our study,patients with comorbidities were 8.45-fold less likely to want elective surgery at the earliest opportunity compared to those with no comorbid conditions (P= 0.0128).Similarly,Changet al[15]reported that patients classified ASA I(60.5%) and ASA II (60.0%) were more likely to agree to undergo earlier elective TJA after the COVID-19 pandemic compared to ASA III (44.4%) and ASA IV (0%) patients (P= 0.01).A multicenter study by Kayaniet al[16]assessed the impact of COVID-19 infection on peri-operative outcomes for patients undergoing surgical treatment for hip fractures.COVID-19 positive patients had increased post-operative mortality rates(P< 0.001),increased risk of post-operative complications (P< 0.001) and more critical care unit admissions (P< 0.001) compared to COVID-19 negative patients[16].Furthermore,COVID-19 positive patients with greater than 3 comorbidities had a significantly higher risk for mortality compared to those with no comorbidities (P<0.001)[16].
The waiting period for elective TJA is high in our sub-Saharan setting when compared to other reported rates worldwide.In our study,the mean length of time for patients awaiting THA was 28.29 mo and 25.03 mo for TKA.In 2018,the average median worldwide waiting time for elective THA was 113 d (range:50-282 d) and 189 d (range:45-839 d) for TKA with wide variation,across countries[18].Initially,longer waiting period was associated with increased patient demand for elective surgery at the earliest opportunity despite the COVID-19 pandemic in our study.Patients awaiting TJA for between 1 and 3 years were 3.34-fold more likely to want elective surgery at the earliest possibility compared to those awaiting surgery for less than 1 year (P< 0.000).A systematic review including 15 studies of patients awaiting TJA for osteoarthritis was conducted to assess the impact of wait times on pain and functional status[19].There was a mean waiting period between 42-399 d with strong evidence that pain and WOMAC score did not deteriorate for patients waiting less than 180 d[19].Similarly,a multicenter study with a mean wait time of 5.07 mo by Vergaraet al[20]observed that patients waiting less than 3 mo had a greater likelihood of achieving successful post-operative outcomes on the WOMAC scale and the 36-item short form survey scores.Furthermore,a multicenter study including 7151 patients found that longer waiting periods were significantly associated with a lower Oxford Hip Score at 12-mo follow-up after THA[21].Patients waiting 12 and 24 mo had a post-operative mean difference of 2.6 and 4.2 Oxford Hip Score points,respectively compared to those waiting less than 6 mo[21].
In our study,55.49% of patients had increased joint pain and 67.2% of patients had decreased functionality respectively,since the postponement of their TJA.Patients that wanted TJA despite the COVID-19 pandemic experienced significantly greater decrease in function compared to those who were prepared to wait.This was demonstrated by significant differences in decreased functionality due to joint pain (P= 0.002) and decreased walking distance (P= 0.034) respectively.Additionally,patients between the ages of 45 to 60 years had significantly more decreased functionality due to joint pain compared to patients younger than 45 years of age(78.5%vs46.3%;P= 0.015).Brownet al[14]in their survey of TJA patients in the united states reported that joint pain had increased for 54% of patients and activity levels had decreased for 50% of patients,respectively since their surgery cancellation.This has long-term implications as several studies have demonstrated significantly less improvement in WOMAC and 36-item short form survey scores for patients with lower baseline function compared to those with higher baseline function persisting through 24 mo follow-up after TJA[12,13].A recent study by Scottet al[11]demonstrated that patients with low scores on the Euro Qol five-dimension general health questionnaire achieved significantly worse joint-specific Oxford scores and satisfaction rates 1 year after TJA,compared with those with higher scores pre-operatively (P<0.001).
Patient consent prior to elective surgery during the COVID-19 pandemic must focus on counseling and education,particularly for high-risk patients.Our study found that the percentage of patients who wanted elective surgery at the earliest opportunity decreased from 88.65% to 54.05% after receiving patient education about the COVID-19 pandemic.Patients in our study that were in the receptive group had significantly less insight on the impact of COVID-19 regarding both their individual health and the response of the healthcare system.Patients in the receptive group were less likely to be aware of the increased morbidity (P= 0.046) and mortality (P= 0.001) associated with COVID-19 if infected peri-operatively when compared to non-infected patients.A purposeful patient education program was implemented by the orthopedic department of the New York University Langone Health in response to the COVID-19 pandemic[6].Orthopedic surgeons counseled patients regarding need for the postponement of surgery due to the COVID-19 pandemic and addressed patient concerns and questions which alleviated their anxiety[6].
In our study,the continued demand group had been awaiting surgery for a shorter length of time (24.7 mo) than the defer group (25.32 mo) and the receptive group (28.91 mo).Despite the shorter waiting period,the continued demand group experienced significantly greater pain than other patients.The continued demand group had a higher mean pain score (P< 0.000) and the greatest proportion of patients with increased joint pain (P= 0.035) since the postponement of surgery compared to the other patient groups.
There are unique challenges that must be considered during the re-initiation of elective surgery.Rizkallaet al[22]proposed that the decision to proceed with either primary or revision hip arthroplasty should be assessed for urgency.The urgency to proceed with hip arthroplasty should be based on both the potential harm of delaying surgery and the potential risk of performing surgery in the context of COVID-19[22].In addition to patient outcomes,the economic implications of the postponement of elective surgery place an increasing burden on healthcare systems[23,24].There have been several guidelines developed to facilitate the return of elective surgery in many parts of the world[23,24].The reinstitution of elective surgery must be carefully implemented to ensure patient and staff safety and the responsible management of healthcare resources and equipment[23,24].Waiting lists should no longer operate on a first-in,first-out basis as was previously used in our institution.The effect of TJA postponement on patients should be assessed on an individualized basis and waiting lists should be prioritized for urgency.
One of the weaknesses of our study is that the waiting period was already long in comparison to worldwide rates.An additional limitation is that the interview was done telephonically,however,to mitigate this there were two individuals conducted interviews and all conversations were recorded.
CONCLUSION
Patient education and counseling are essential for those who have had elective procedures postponed during the COVID-19 pandemic.South Africa has longer waiting periods for TJA in comparison to international reports and the further postponement of surgery increases the risk of poor post-operative outcomes.There is deterioration in patients’ physical and mental health whilst awaiting TJA and should be individually reassessed before rescheduling their surgery.Waiting lists should be prioritized for urgency with the re-initiation of elective surgery based on their current overall health status.
ARTICLE HIGHLIGHTS
Research background
The postponement of elective surgery in response to the coronavirus disease 2019(COVID-19) pandemic resulted in a total shutdown of total joint arthroplasty (TJA).The impact of elective surgery postponement has resulted in the cancellation of approximately 92.6% TJAs in Europe.The demand for TJA is already high and waiting lists continue to grow with 150000 procedures per month postponed in the United States.
Research motivation
There is wide variation across countries worldwide;with the average median waiting time of 113 d (range 50-282 d) for total hip arthroplasty and 189 d (range 45-839 d) for total knee arthroplasty respectively.Patients awaiting surgery longer than 6 mo and those with poor pre-operative baseline function have demonstrated increased risks for poor outcomes after TJA.The unprecedented postponement of elective TJA in response to the COVID-19 pandemic may impact patients awaiting surgery.
Research objectives
Our aim was to assess the impact of TJA postponement on the physical and mental health of patients awaiting elective surgery.We secondarily sought to determine the demand for TJA and average waiting time for our South African population.Additionally,we investigated the role of patient insight after providing education and counseling regarding the healthcare system’s response to the COVID-19 pandemic.The effect of TJA postponement on patients should be considered with the re-initiation of elective surgery and waiting lists should be prioritized to optimize outcomes.
Research methods
A prospective cross-sectional telephonic interview-based study of patients awaiting TJA at an academic referral institution in South Africa during the COVID-19 pandemic.We recorded baseline demographic data and length of time awaiting surgery and demand for TJA.A 5-point Likert scale was used to determine the degree to which the patient felt the postponement of surgery had affected various characteristics of their physical and mental health.We assessed patient insight regarding elective surgery cancellation in response to the COVID-19 pandemic and subsequently re-evaluated demand for TJA after providing education and counseling.
Research results
Patients with comorbidities were 8.45-fold less likely to want elective surgery at earliest possibility compared to those with no comorbid conditions (P = 0.013).In our study in South Africa,the mean length of time for patients awaiting total hip arthroplasty was 28.29 mo and total knee arthroplasty was 25.03 mo,respectively.Before and after receiving patient education,the number of patients who demanded elective TJA decreased respectively,from 164 patients (88.65%) to 100 patients (54.05%)(continued demand group).The continued demand group had a higher mean pain score (P< 0.000) and the greatest proportion of patients with increased joint pain (P=0.035) since the postponement of surgery compared to the other patients.
Research conclusions
The effect of TJA postponement on patients should be assessed on an individualized basis and waiting lists should be prioritized for urgency.Patient consent prior to elective surgery during the COVID-19 pandemic must focus on counseling and education,particularly for high-risk patients,to ensure optimal outcomes.The urgency to proceed with TJA should be based on both the potential harm of delaying surgery and the individual risk profile of performing surgery incurred by each patient,respectively,in the context of the COVID-19 pandemic.
Research perspectives
There is a demonstrated need to postpone elective surgery in response to the COVID-19 pandemic,particularly in high-risk patients.Patients should be reassessed and thoroughly counseled prior to rescheduling their elective procedures,particularly those at increased risk for morbidity and mortality if infected with COVID-19 perioperatively.In addition to the potential negative impact on patient outcomes,the economic implications of the postponement of elective surgery place an increasing burden of healthcare systems worldwide.The reinstitution of elective surgery must be carefully implemented to ensure patient and staff safety and the responsible management of institutional resources.
杂志排行
World Journal of Orthopedics的其它文章
- COVID-19 and its effects upon orthopaedic surgery:The Trinidad and Tobago experience
- Slacklining:An explanatory multi-dimensional model considering classical mechanics,biopsychosocial health and time
- Dual antibiotic loaded bone cement in patients at high infection risks in arthroplasty:Rationale of use for prophylaxis and scientific evidence
- Advantages of preoperative planning using computed tomography scan for treatment of malleolar ankle fractures
- Proximal tibial osteotomy for genu varum:Radiological evaluation of deformity correction with a plate vs external fixator
- Bibliometric analysis of research on the effects of human immunodeficiency virus in orthopaedic and trauma surgery