Life after recovery from SARS, influenza, and Middle East respiratory syndrome: An insight into possible long-term consequences of COVID-19
2021-03-11AmirMasoudAfsahiAlecioLombardiSaraValizadehAliGholamrezanezhad
Amir Masoud Afsahi, Alecio F Lombardi, Sara Valizadeh, Ali Gholamrezanezhad
Amir Masoud Afsahi, Alecio F Lombardi, Department of Radiology, UCSD, La Jolla, CA 92093,United States
Sara Valizadeh, Department of Restorative Dentistry, School of Dentistry, Tehran University of Medical Sciences, Tehran 1439955991, Iran
Ali Gholamrezanezhad, Department of Radiology, Keck School of Medicine of USC, Los Angeles, CA 90033, United States
Abstract Viral infectious diseases have become an increased public health issue in the past 20 years. The outbreaks of severe acute respiratory syndrome coronavirus (SARSCoV-1) in 2002, influenza H1N1 in 2009, Middle East respiratory syndrome-CoV in 2012, and the current new coronavirus SARS-CoV-2 have shown that viral infectious diseases are a major concern in the 21st century. As the world lives under the pandemic of a new coronavirus (COVID-19), knowing the clinical characteristics from those past diseases and their long-term outcomes is important to understand the current coronavirus pandemic and its complications and consequences better and plan for possible future outbreaks. Several long-term complications have been described with these respiratory viral diseases, such as decreased pulmonary function, pulmonary fibrosis, chronic fatigue syndrome,avascular necrosis of bone, polyneuropathy, encephalitis, posttraumatic stress disorder, depression, and anxiety. This article summarizes several studies describing chronic complications and long-term outcomes of patients recovered from these viral syndromes.
Key Words: COVID-19; Long-term; Consequences; SARS; Middle East respiratory syndrome; Influenza
INTRODUCTION
The widespread infectious diseases became a significant public health issue globally in the past 20 years. There have been four major viral contagious outbreaks in the 21st century: The severe acute respiratory syndrome (SARS) in 2002, the H1N1 influenza pandemic in 2009, the Middle East respiratory syndrome (MERS) in 2012 and the current novel coronavirus (COVID-19) in 2019-2020. In between, every year, thousands of people die from complications of seasonal influenza around the world. Besides their high mortality rates, these viral infectious diseases proved to cause long-term outcomes for those who survive. Pulmonary lung dysfunction and residual parenchymal/imaging abnormalities can persist several years after hospital discharge.Many patients can develop avascular necrosis of bone due to the high doses of corticosteroids used in treatment. Several studies reported chronic fatigue syndrome with neuromuscular dysfunction as complications of these viral syndromes. The psychological and mental burden has also been proved in patients and health care workers involved in the treatment and coordination of these pandemics. Acute neurologic complications may cause long-term disability, which can have a significant impact on the health care system and the quality of life of those affected. This article aims to review studies describing long-term multi-system clinical outcomes in patients affected by SARS, MERS, and Influenza following the most recent outbreaks. A summary of main complications and long-term outcomes in patients affected by these outbreaks is shown in Table 1.
RESPIRATORY SYSTEM
SARS
The first cases of a new severe lower respiratory tract infection were reported in early 2003 in Guangdong, China, rapidly spreading throughout Asia and Canada in the following months. Later in that year, this infection became known to be caused by a new coronavirus, named SARS-CoV, that spread through 29 countries from January to September 2003, infecting a total of 8098 patients and causing 774 deaths, with a mortality rate of 9.5%[1]. SARS-CoV is a single-stranded positive RNA virus that belongs to the coronavirus genus and can be spread through the respiratory system,droplets, aerosol, and contaminated surfaces. Young adults between 20-50 years old were the most affected population. Most patients presented initially with fever,headache, joint pain, and dyspnea and could progress to pneumonia and spread to other systems with recovery or death.
Pulmonary involvement of SARS is described to occur in three distinct phases: From 1-7 d of infection (initial phase) mild unilateral ground-glass opacities predominates,from 7-14 d of infection (progression phase) there is an expansion of the ground-glass opacities that becomes multi-focal, bilateral and can progress to consolidations, finally after 2-3 wk of symptom onset the recovery phase begins, with the absorption of the lesions. Some patients may develop interstitial, lobular, and lobar thickening,honeycomb manifestations and traction bronchiectasis characterizing pulmonary fibrosis[1].
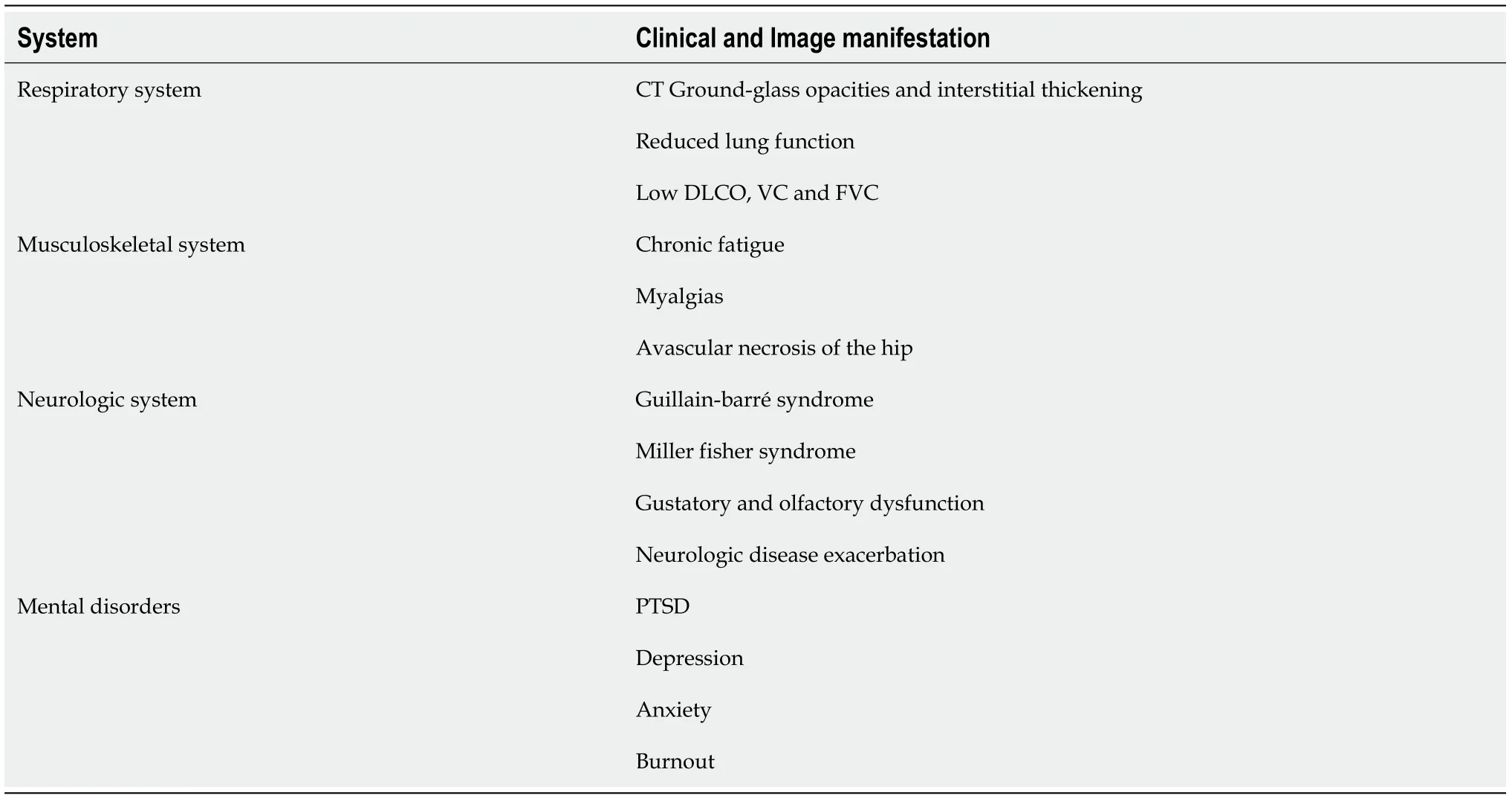
Table 1 General complications and long-term manifestations associated with SARS, Middle East respiratory syndrome, and influenza
Chronic complications of SARS have been described in the following years of the outbreak. The respiratory system is the most affected, characterized by pulmonary fibrosis and decreased lung function. A recent systematic review and meta-analysis by Ahmedet al[2]showed that critically ill patients recovered from SARS presented with significant pulmonary function impairment and reduced exercise tolerance 3 to 6 mo post disease recovery[2]. These patients had also reduced diffuse capacity of the lung for Carbon monoxide (DLCO), vital capacity (VC), and forced vital capacity (FVC),which according to the authors, might have impacted aerobic capacity, general physical conditioning and exercise tolerance. The authors also describe that although many patients had improvement in lung function, the meta-analysis has shown that reduction in DLCO and lung fibrosis may persist for years in some patients[2].
Nget al[3]studied the pulmonary function and persistent pulmonary CT abnormalities in patients recovered from SARS in Hong Kong, six months after hospital discharge. The investigators found that 43 out of 57 patients had some pulmonary function abnormality (with the mild obstructive defect as the most common finding), 20 patients had reductions in the carbon monoxide transfer factor(TLCO), 17 patients had abnormal total lung capacity, and four patients had abnormal FVC. Radiological abnormalities were also found in 43 patients out of 57: The median number of segments involved were three in the upper and lower lobes, and the use of corticosteroids was associated with the persistent findings[3].
The most common image findings in high-resolution pulmonary CT in the late stage of acute respiratory distress syndrome (ARDS) caused by SARS were ground-glass opacification, interstitial thickening, and consolidation, according to a study by Joyntet al[4]. Other findings were lung fibrosis, cysts, and even pneumothorax, which could be associated with mechanical ventilation, according to the authors. The use of mechanical ventilation or duration of treatment did not appear to have influenced imaging findings[4]. Wuet al[5]studied lung function and high-resolution CT image of the chest in 11 patients recovered from SARS at six and 84 mo after hospital discharge[5]. The investigators found that eight patients (72.7%) presented reticulation and interlobular thickening at 84 mo follow-up, two patients (18.2%) showed groundglass opacification and only 1 had no lung abnormality. Traction bronchiectasis was found in six patients. As for the lung function, at 84 mo follow-up nine (81.8%) from the eleven patients had a low DLCO, eight (72.7%) had mild lung function damage,and 1 (9.1%) had moderate lung function damage[5].
SARS may show a clinical presentation similar to ARDS in the acute phase and shares with ARDS some imaging characteristics and long-term sequela represented by pulmonary interstitial thickening and ground-glass opacities[6].
Chanet al[7]described a series of patients treated from SARS in China in which 20%were found to have mild restrictive pulmonary defect six weeks after discharge[7]. The investigators also described other case series that showed reduced lung inspiratory and expiratory pressures, low DLCO, reduced FVC, and muscle fatigue that could partially explain restricted function lung defects in some patients[7].
Zhanget al[8]studied 71 health care workers that contracted and recovered from SARS during the outbreak in 2003 in China for 15 years, from August 2003 to March 2018[8]. Most of the patients had a diminished percentage of pulmonary lesions on CT scans (9.4% to 3.2%) from 2003 to 2004 that remained stable until 2018[8]. Image abnormalities most described were residual ground-glass opacities and interstitial thickening. Pulmonary function was the same between 2006 and 2018, and patients showed a mild decline in diffusion capacity from 2006 to 2018[8].
MERS
MERS is an ongoing coronavirus outbreak caused by the MERS-CoV which had the first case diagnosed in 2012 in Saudi Arabia. According to the most recent report from the World Health Organization, a total of 2494 cases of MERS, including 858 deaths(case-fatality rate: 34.4%), were reported globally in 27 countries. The clinical presentation is comprised of fever, chills, malaise, anorexia cough and dyspnea,nausea and vomiting that can progress to severe lower respiratory tract disease,ARDS, acute kidney injury and multi-organ failure, frequently requiring mechanical ventilation and intensive care hospital treatment[9]. The risk of transmission is increased with direct or indirect contact with dromedary camels and patients infected with MERS-CoV. People from 30 to 50 years are the most commonly affected, but higher mortality rates occur among patients 50-79 years, according to the WHO[10].
Batawiet al[11]studied the quality of life reported by survivors from MERS that required hospitalization in Saudi Arabia after one year of the diagnosis[11]. Average scores were low for physical functioning, general health, emotional role, and were worst among those patients that required intensive care unit (ICU) treatment compared with patients treated in the non-ICU environment.
Image findings in MERS are nonspecific, with ground-glass opacities and consolidation being the most commonly reported[12]. Lung fibrosis, ground-glass opacities, and pleural thickening are the most common chronic radiographic findings,with more abnormalities being associated with higher days of ICU treatment and older age upon diagnosis[13]. Some patients can develop traction bronchiectasis and fibrosis,along with subpleural bands and architectural distortion[14,15]. In one study with 14 critically ill patients diagnosed with MERS in 2014, nine patients died, and those who survived had good clinical outcomes after one year. However, the authors did not detail the pulmonary function status or image findings[16].
Influenza
Influenza viruses are negative-sense, segmented RNA viruses from the Orthomyxoviridae family that cause annual seasonal epidemics worldwide, and under some circumstances, can go through reassortment of its segmented genetic material, giving origin to different strains causing pandemics[17,18]. According to the centers for disease control and prevention (CDC), there were five influenza pandemics in the twentieth century (1918, 1930, 1957, and 1968) and one in the 21stcentury (2009 H1N1). The most recent one, caused by the H1N1pdm09 Flu Virus, caused 12469 deaths in the United States from April 2009 to April 2010 and has circulated seasonally throughout the country[19].
The most common acute and subacute respiratory and overall complications of seasonal and epidemic influenza are primary viral pneumonia, secondary bacterial pneumonia, pneumonia caused by opportunistic agents and exacerbation of chronic obstructive pulmonary disease, and asthma. However, during epidemics, infections tend to be more serious, usually requiring ICU treatment, presenting with a higher mortality rate than the seasonal disease[20,21].
Chenet al[22]reported chronic pulmonary complications from influenza A (H7N9)during two years after discharge from the hospital and showed interstitial abnormalities and fibrosis on lung image after six months, along with restrictive and obstructive lung function throughout the follow-up period[22].
Luytet al[23]studied a total of 24 patients recovered from influenza A (H1N1)infection treated in ICUs with and without extracorporeal lung assist (ECLA) one year after hospital discharge and found that 50% of the patients in the group treated with ECLA and 40% of them not treated with ECLA reported significant exertion dyspnea,and 75% and 64% of the patients in each group respectively had decreased diffusion lung capacity across the blood-gas barrier[23]. Both groups also had reduced exercise capacities and reported lower health-related quality of life compared with a group from the healthy population[23].
Liet al[24]showed in a study with children recovered from SARS that 34% had highresolution CT residual abnormalities: Ground-glass opacities (31.2%), air trapping(8.5%), and combination of ground-glass and air trapping (18.8%). The investigators also found mild decreased pulmonary function in four out of 38 patients[24].
A summary of the main chronic clinical and imaging manifestations of SARS, MERS and Influenza is described on Table 2.
Musculoskeletal system
Avascular necrosis (AVN) of bone has been described as a significant complication of SARS, as critically ill patients frequently require high doses of corticosteroid treatment.Honget al[25]described an incidence of 28 patients with AVN among 67 patients diagnosed with SARS, and that presented joint pain between March and May 2003[25].The mean time from SARS diagnosis and development of AVN was 119 days, and all patients received a total dose of corticosteroid above 700 mg[25]. The most common affected sites were femoral head and knees. Magnetic resonance imaging (MRI) played an essential role in the diagnosis since no abnormalities were found on the radiographs. Later the investigators described in another study that Diffusionweighted MRI could be used to reliably diagnose AVN in patients treated from SARS with corticosteroid[26].
Another study by Sunet al[27]investigated the possible role of anticardiolipin antibodies in the etiology of AVN in 62 patients diagnosed with post-SARS osteonecrosis and found that 33.9% of patients had at least one type of anticardiolipin antibodies (IgA, IgG, and IgM) compared to 7.7% in the control group. They concluded that these antibodies might play a role in the pathogenesis of post-SARS osteonecrosis[27].
The incidence of AVN after SARS varies among studies. Shenet al[28]described a 3%incidence in a group of 84 health care workers diagnosed with SARS and treated with different dosages of corticosteroids[28]. Liet al[29]found an incidence of 30% among a cohort of 40 patients diagnosed with SARS and treated with corticosteroids[29].
Lvet al[30]conducted a longitudinal study with 71 patients treated with corticosteroids for SARS over 36 mo after diagnosis. They showed that 29% of the patients developed AVN of the hips within 3-4 mo after treatment, two patients developed AVN after one year of the diagnosis and 11 patients after three years of observation outlining the long-term adverse effects[30].
Zhaoet al[31]studied 190 hips from 117 patients that developed post-SARS AVN during seven years from diagnosis and found that 66 hips progressed in symptoms, 55 hips collapsed, and ten hips showed lesion regression[31]. According to the authors, the progression of symptoms and the bone collapse was associated with lesions with higher dimensions and lower viable lateral columns in the femoral heads. The mean time from the administration of corticosteroids and the development of AVN was 6.26 mo, and the mean time from the corticosteroid use and the development of symptoms was 18.39 mo[31]. In the 15-year follow-up study by Zhanget al[8], though, patients diagnosed with femoral head necrosis after treatment of SARS showed decreased AVN volume from 2005 to 2013 and plateaued until 2018[8].
Several patients that recovered from SARS were presented late with musculoskeletal pain, weakness, fatigue, shortness of breath, psychological distress, and significant sleep problems, known as the post-SARS syndrome. A retrospective study by Moldofskyet al[32]showed that chronic post-SARS syndrome was characterized by persistent fatigue, diffuse myalgia, weakness, depression, and nonrestorative sleep with associated REM-related apneas/hypopneas[32]. The authors suggested that this may be caused by the direct viral invasion of the central nervous system and peripheral tissues resulting in chronic post-inflammatory CNS pathology.
In a case-series by Stainsbyet al[33], three patients diagnosed with SARS presented with a variety of neurological, muscular and joint findings that improved after conservative treatment, which according to the authors, could be caused by a viral myositis or from the use of corticosteroids in the treatment of the patients. The acute inflammatory condition with increased cytokines, platelet-activating factors, free radicals, and proteases was also raised as possible causes[33]. Table 3 summarizes the main chronic musculoskeletal findings in patients treated for SARS.
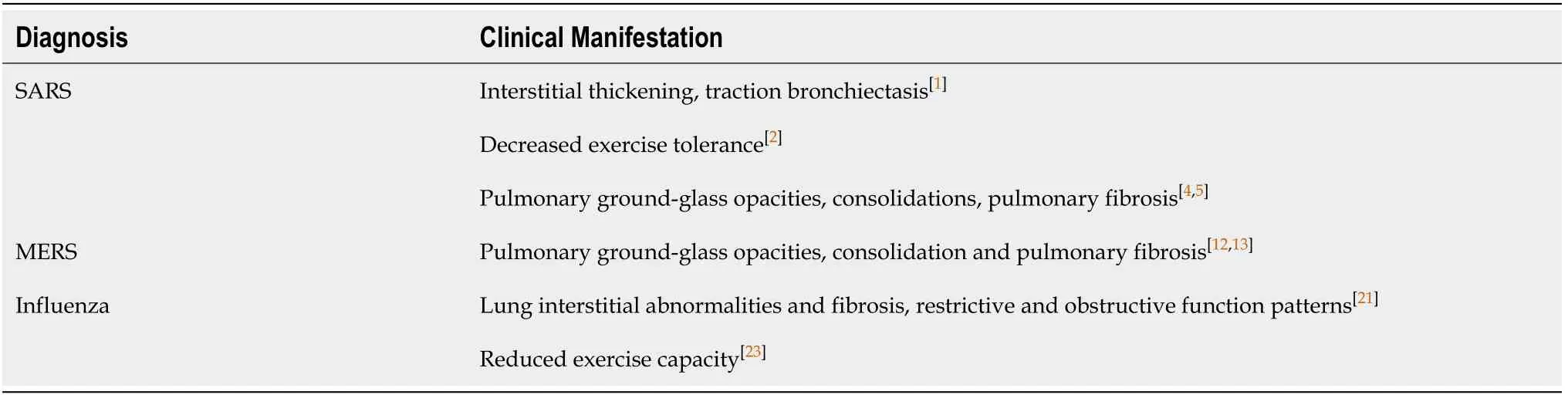
Table 2 Common respiratory system long-term manifestations associated with severe acute respiratory syndrome, Middle East respiratory syndrome, and influenza
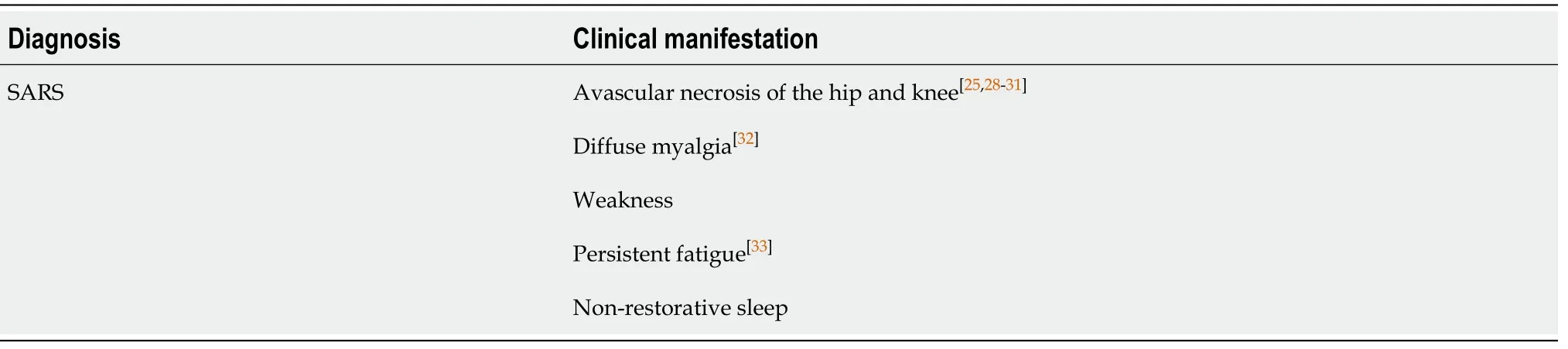
Table 3 Common chronic musculoskeletal disorders associated with severe acute respiratory syndrome
Neurologic system
Coronaviruses can invade the nervous system by several routes, including transsynaptic transfer, direct invasionviathe olfactory nerve, or migration across the blood-brain barrier, spreading to different central nervous system locations, including the brain, basal ganglia, midbrain, where neuronal death can occur[34], causing a wide range of neurological complications[35]. Immunologic process are also suggested as possible contributors to neurologic complications in these patients[36]. Patients with preexisting neurological disorders are at risk of developing complications from coronaviruses diseases in association with neurological disease exacerbation,especially those with previous diagnosis of dementia and Parkinson’s disease[37].Clinicians should be aware of this risk of exacerbation of neurologic disorders to take early preventive measures and long-term follow-up.
Most of the neurologic complications found in patients with viral infections like SARS, MERS, and Influenza are acute, with headache, anosmia, seizures, and encephalitis as the most common. Encephalitis and Guillain-Barre syndrome have been reported 2-3 wk after the acute symptoms of MERS and are diseases with the potential to cause long-term sequelae[38].
Recent case reports have linked SARS coronavirus to rapid-onset Guillain-Barré syndrome that evolved to tetraparesis or tetraplegia over a period of 36 h to 4 d and necessitated mechanical ventilation; and Miller-Fisher syndrome, presenting with ageusia, oculomotor palsy, ataxia, areflexia[39,40]. One patient presented with increased serum immunoglobulin antibodies and treatment with intra-venous immune globulin resulted in complete recovery.
It is important to mention the gustatory and olfactory dysfunction referred by patients after infection by COVID-19[41], that needs further long-term investigation and follow-up considering its potential to cause low quality of life.
Mental / psychiatric abnormalities
Psychiatric symptoms were common in patients affected by SARS and MERS and in health care workers involved in the frontlines of treatment. A study with 90 patients that survived the SARS outbreak showed 58.9% incidence of psychiatric disorders and 33.3% prevalence of any mental disorder after 30 mo[42]. Depression, anxiety, and posttraumatic stress disorder (PTSD) were the most commonly diagnosed, and the symptoms were worst in health care workers affected by the disease[42].
In another study with patients recovered from SARS in Hong Kong, about 35% of the patients reported “moderate to severe” or “severe” anxiety and depressive symptoms, which were more prevalent in those who had family members killed by the disease or were health care workers[43]. PTSD symptoms have been found in 4% of patients one month after hospital discharge for SARS and 5% after three months of discharge in a cohort of 131 patients[44]. Parket al[45]evaluated survivors of MERS in a prospective cohort study at multiple centers throughout Korea, assessing PTSD and depression 12 mo after hospital discharge and found a 42.9% prevalence of PTSD symptoms and 27% prevalence of depression[45].
Another follow-up study from Lamet al[46]showed that even four years of hospital discharge patients affected by SARS had active psychiatric illnesses (40% prevalence)and chronic fatigue symptoms (40.3% prevalence)[46]. The quality of life of patients recovered from MERS and SARS has been assessed in a study by Batawiet al[11]one year after diagnosis showing similar results in both groups, but lower scores for those patients admitted to ICU during treatment[11].
Health care workers comprise a group especially sensitive to mental health problems during infectious disease outbreaks. The long-term impact 13 to 26 mo after the SARS outbreak in 769 health care workers has been assessed and showed significantly higher levels of burnout, psychological distress, and posttraumatic stress[47]. According to the investigators, personal variables that contributed to adverse outcomes were maladaptive coping by avoidance, hostile confrontation, self-blame contributed, and attachment anxiety[47].
An interesting topic that emerged during the COVID-19 pandemic is the widespread use of telemedicine, not only in clinical specialties but also in surgery specialties[48], which could be an option in the future to help underserved patients and reduce health care workers burden by consulting less-severe patients that should not go to a hospital through online counseling. Table 4 gives a summary of the main neurologic and mental chronic disorders associated with SARS, MERS and Influenza.
CONCLUSION
Viral infections and especially the recent SARS, MERS, and Influenza, can affect different systems with potential long-term clinical outcomes that may reduce the quality of life and impair the work capacity of the patients. A high prevalence of mental and psychiatric symptoms has been associated with SARS, and MERS recovered patients and health care workers involved in treatment. Chronic fatigue and neurologic sequelae were common complications among patients with SARS and influenza. Avascular necrosis of the hip and joint pain has also been described as a common complication from the high doses of corticosteroid treatment necessary in critically ill patients.
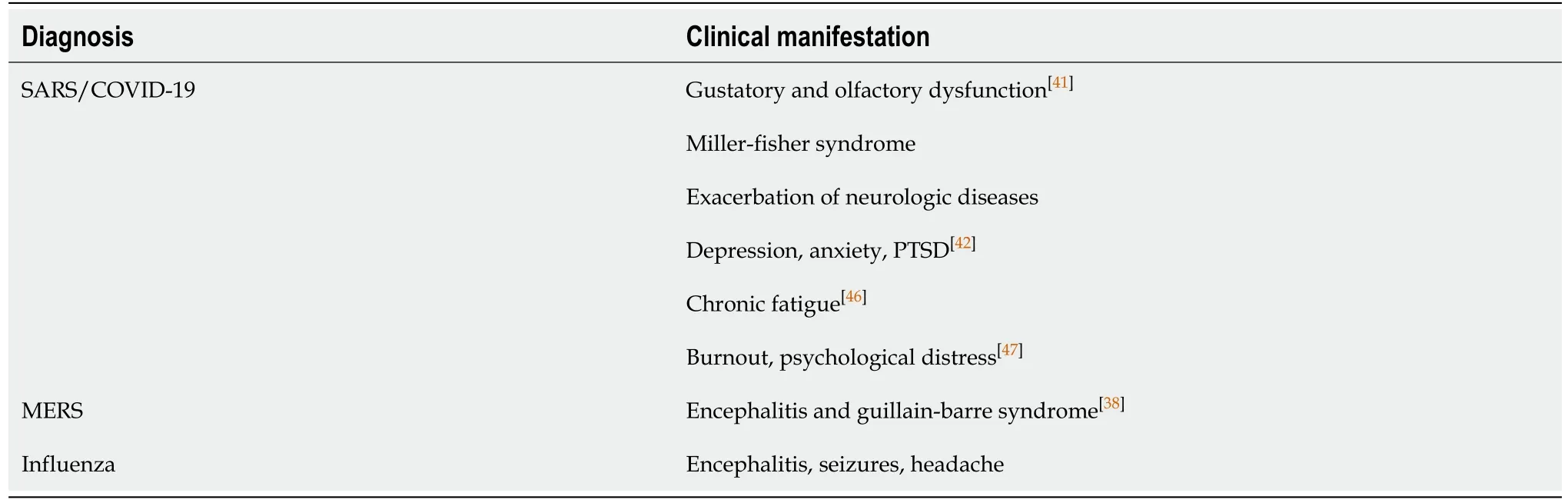
Table 4 Neurologic and mental chronic manifestations associated with severe acute respiratory syndrome, Middle East respiratory syndrome, and influenza
