Fecal microbiota transplant and dermatologic disorders:A retrospective cohort study assessing the gut microbiome’s role in skin disease
2021-02-23AshleySnyderJamesAbbottKyleJensenAaronSecrest
Ashley M Snyder,James Abbott,M Kyle Jensen,Aaron M Secrest
Ashley M Snyder,James Abbott,Aaron M Secrest,Department of Dermatology,University of Utah,Salt Lake City,UT 84132,United States
Ashley M Snyder,Aaron M Secrest,Department of Population Health Sciences,University of Utah,Salt Lake City,UT 84108,United States
M Kyle Jensen,Division of Pediatric Gastroenterology,Hepatology and Nutrition,Department of Pediatrics,University of Utah,Salt Lake City,UT 84113,United States
Abstract BACKGROUND There is indication that fecal microbiota transplant (FMT) has the potential to alter the course of chronic skin disease,but few studies have investigated this phenomenon beyond case reports.Research with larger sample sizes is needed to provide a more thorough assessment of possible associations and to establish a broader foundation upon which to base hypotheses.AIM To identify associations between FMT and skin conditions,particularly infectious and inflammatory etiologies,and the role of dermatology post-FMT.METHODS We conducted a retrospective cohort study involving a chart review of all patients whom received FMT between January 2013 and December 2019 at a single academic medical center.Dermatologic follow-up was assessed for the two years after FMT or through March 2020 for more recent procedures.Dermatologic diagnoses and visits within the study time frame were recorded and assessed for trends.This study was exploratory in nature.Descriptive statistics were calculated,and the t-test,Pearson’s chi-squared test,and Fisher’s exact test were used to calculate P values.RESULTS Most patients were female (61.5%) and ethnically not Hispanic or Latino (93.6%).Median age was 38 (range,17-90).In total,109 patients who underwent 111 fecal microbiota transplant events were included.Twenty-six events (23.4%) involved a dermatology office visit post-procedure,and of these events,20 out of the 26(76.9%) had an infectious or inflammatory skin condition.The mean time to first visit was 10.0 (± 7.0) mo.The most common diagnoses were dermatophyte,wart(s),and dermatitis,though no specific diagnoses predominated in a way indicating FMT had a significant impact.More patients with a post-FMT skin disease diagnosis had a history of Crohn’s disease compared to those without (P =0.022),but results could be affected by a small sample size.CONCLUSION Our study is limited by its retrospective nature,but the findings allow a glimpse at dermatologic conditions post-FMT.Few significant associations were found,but potential associations between FMT and skin disease should be further investigated,preferably in prospective studies,to identify how FMT might be of use for treating infectious and inflammatory skin diseases.
Key Words:Fecal microbiota transplantation;Infections;Inflammation;Microbiota;Skin diseases;Retrospective studies
INTRODUCTION
Chronic inflammatory diseases are increasingly being linked to the gut microbiome[1],but few publications have explored how the gut microbiome influences inflammatory and infectious skin conditions.The microbiome has long been considered a potential contributor to certain skin diseases,but research is still lacking to support associations between skin disease and treatments that target the microbiome,in particular the gut microbiome.Fecal microbiota transplant (FMT) is a procedure that introduces a healthy donor’s gut microbiome through feces to a patient with refractory or recalcitrantClostridioides difficile(C.difficile) infection.Though FMT has primarily been used to treatC.difficileinfections,this treatment has also been investigated in numerous studies for its effects on ulcerative colitis (UC) and Crohn’s disease[2],as well as more recent expansion to successfully treat other seemingly unrelated conditions like recurrent hepatic encephalopathy[3],milk allergy[4,5],and autism spectrum disorder[6].
The role of FMT in managing infectious and inflammatory conditions has now expanded into dermatology.Recent case reports provide evidence of temporal improvement in chronic inflammatory skin disease after FMT,including reports of two patients with alopecia universalis,who saw hair regrowth on multiple regions of the body after FMT[7].Also,patients with psoriasis[8]and psoriatic arthritis[9]reportedly experienced improvement after FMT.Further,some mouse studies have even attempted to understand the role of FMT for management of melanoma[10,11].However,larger studies on FMT and skin disease in humans are needed to better comprehend the extent of skin conditions which FMT could potentially influence.Here,we present a retrospective cohort study involving patients whom received FMT.We identify and describe dermatologic conditions post-FMT,specifically infectious and inflammatory etiologies,with the goal of better understanding the effects of FMT on skin disease.
MATERIALS AND METHODS
We conducted a retrospective cohort study using electronic medical record (EMR) data from University of Utah Health.A total of 141 patients with FMT code ICD-10-CM Z94.89 on their records from January 2013 to December 2019 were identified.Patients were included for analysis if (1) their record included a clinician’s report on the FMT procedure(s) at University of Utah Health;(2) their record included visit information at University of Utah Health up through March 2020 that was not related to an FMT procedure or follow-up onC.difficileinfection post-FMT;and (3) the patient had not died within eight weeks after FMT.Patients not meeting all three of these criteria were excluded.
Information for analysis was collected from the EMR on sex,ethnicity,age(calculated based on birth date and first FMT at our institution),fecal transplant history,history of gastrointestinal conditions and solid organ transplant[12]before FMT procedure,antibiotic use within eight weeks after FMT (excluding topical antibiotics),chronic inflammatory skin conditions pre-FMT and/or inflammatory or infectious skin conditions documented within six months prior to FMT,and subsequent dermatologic evaluation in our Department of Dermatology up to two years after FMT or through March 2020 for more recent FMT procedures.Antibiotic use (related to treating aC.difficileinfection or not) within eight weeks after FMT was collected due to research that indicates FMT may be less effective if there is antibiotic exposure in this time frame[13].Race calculations are not presented due to uncertainty about the accuracy of this information in the EMR;conversely,ethnicity information came from demographic information believed to be provided by the patients.
Information collected was based on FMT events,which could include more than one FMT procedure.If there were at least two years between two FMT procedures,the two procedures were counted as separate FMT events and had separate evaluations of antibiotic use,skin conditions prior to FMT,subsequent dermatologic evaluation,and FMT,gastrointestinal condition,and solid organ transplant histories.Procedures occurring within two years of each other were counted as the same FMT event,and information was collected for the most recent FMT procedure in an event.The variable of exception was age,which was calculated based on a patient’s first FMT at our institution.
We included two years of dermatology follow-up per FMT event to account for changes in skin conditions which might more directly be attributed to microbiota that persisted after FMT[6,14].Information on skin conditions was obtained from dermatology office visits,and information on occurrence of dermatology office visits was recorded as well,excluding visits that were classified as being specifically for elective/cosmetic surgery.Where needed,laboratory reports were reviewed to help assess what a skin condition reported for a visit was.
This study was exploratory in nature,so extensive statistical analyses were not performed and some analyses were post hoc.At-test was used for continuous variables,and Pearson’s chi-squared test or Fisher’s exact test were used for categorical variables as appropriate.Two-tailed tests were used where possible.The lead author of this study has had training and experience with biomedical statistics,and she determined and conducted the statistical analyses.Microsoft Excel 2016(Microsoft,Redmond,WA,United States) and STATA version 16 software (StataCorp LLC,College Station,TX,United States) were used for calculations.
Exempt status was obtained from the University of Utah Institutional Review Board(#76927).
RESULTS
Demographics
Thirty-two patients (22.7%) out of the 141 patients identified were excluded based on our inclusion criteria.Out of the remaining 109 patients,25 (22.9%) had a dermatology office visit post-FMT,and 19 (17.4%) had a skin condition diagnosis at one or more of these visits.Over one-third had additional gastrointestinal conditions beyondC.difficile.Nineteen patients (17.4%) had a history of Crohn’s disease,and 21 (19.3%) had a history of UC (Table 1).Other gastrointestinal conditions beyondC.difficile,Crohn’s disease,and UC that were observed include serrated polyposis syndrome,microscopic colitis,alcohol-related cirrhosis,primary sclerosing cholangitis (in addition to Crohn’s disease or UC),and small bowel obstruction with toxic megacolon.Eight patients(7.3%) had a documented chronic inflammatory skin condition and/or an inflammatory or infectious skin condition within six months prior to FMT,including acne (n= 3),antiphospholipid antibody syndrome with lupus,diffuse cutaneous systemic sclerosis,perianal strep,small plaque parapsoriasis,urticarial vasculitis,varicella zoster virus,and wart(s).Most patients were female (61.5%) and identified as ethnically not Hispanic or Latino (93.6%).The median age was 38,and the age range was 17 to 90 years.Solid organ transplant was seen in 5 patients (4.6%),and all solid organ transplants were performed at least 10 mo before FMT.Antibiotic use was reported in almost a quarter of patients.The distribution of these variables among patients whom had a noted skin condition at a post-FMT dermatology office visitvsthose whom did not is also shown in Table 1;most of the demographic characteristics were relatively similar between these groups,except that proportionally more patients with noted skin conditions had a history of Crohn’s disease (P= 0.022).Most patients with a post-FMT diagnosis of wart(s) had a history of Crohn’s disease as did both patients diagnosed with tinea versicolor post-FMT.
Two patients had more than one FMT event,leading to a total of 111 FMT events.Of these events,a strong majority (96.4%) were administeredviacolonoscopy,and other methods of administration included ileoscopy,pouchoscopy,and sigmoidoscopy.
Post-FMT dermatology office visits
Twenty-six FMT events (23.4%) had dermatology office visits post-FMT.Twenty of these events (76.9%) had a noted infectious or inflammatory skin condition at any of these visits,and 19 events (73.1%) had a noted condition at the first dermatology visit post-FMT.
A total of 53 dermatology office visits were noted (Table 2).First visits after the most recent FMT occurred within an average of 10.0 (± 7.0) mo post-FMT.There were nine first visits within six months after FMT,and of these visits,five (55.6%) included at least one diagnosis of the following:acne,intertrigo,rosacea,telogen effluvium,tinea versicolor,and urticaria.
Figure 1 illustrates the distribution of new skin conditions over the months post-FMT at any dermatology office visit.Diagnoses were included in this figure if they were not noted as a pre-FMT condition and they were not subsequent diagnoses of the same condition if the patient was seen more than once for a particular condition post-FMT [overall,this excluded diagnoses of diffuse cutaneous systemic sclerosis,rosacea,and wart(s)].Dermatophyte,wart(s),and dermatitis were the most common conditions to appear,and all occurred after the first eight months post-FMT.Overall,it seems there was not a clear pattern to the distribution of new diagnoses after FMT.
DISCUSSION
We present a retrospective review of FMTs performed at our institution to elucidate potential associations with dermatologic conditions and the role of dermatologic evaluation.Through our study,we were able to reveal that infectious and inflammatory etiologies were relatively infrequently documented post-FMT.Additionally,these patients did not appear to have predilection for any particular dermatologic etiologies.The results of this study present information to formulate new ideas on future research,but there are limitations to what conclusions can be drawn.
Previous research indicates there is a variety of skin conditions that appear to be potentially influenced by the gut microbiome.In addition to alopecia[7]and psoriasis[8,9],changes in acne[15]and eczema[4]in FMT recipients have been noted,though these particular studies provide minimal evidence.Acne patients do appear to have differences in gut microbial composition compared to non-acne patients,and these differences may be affected by environment-related factors like diet and stress[16].A gut-brain-skin axis hypothesis has been presented to explain connections between factors previously thought to be unrelated,and improvements in acne due to probiotic use provide further clues about the impact of gut bacteria[16].Atopic dermatitis patients also appear to have differences in bacterial composition as well as subsequent immune system-related gene expression compared to controls[17,18].This and other evidence indicates that the immune system may be impacted by the gut microbiome.For example,the gut microbiome has been investigated for its role in cancer immunotherapy[19]and appears to be involved in antitumor immunity and inhibition of tumor growth for melanoma[20].Studies on fecal transfer from human melanoma patients to mice have suggested that the gut microbiome is involved in immune responses and may impact tumor growth during immunotherapy[10,11].
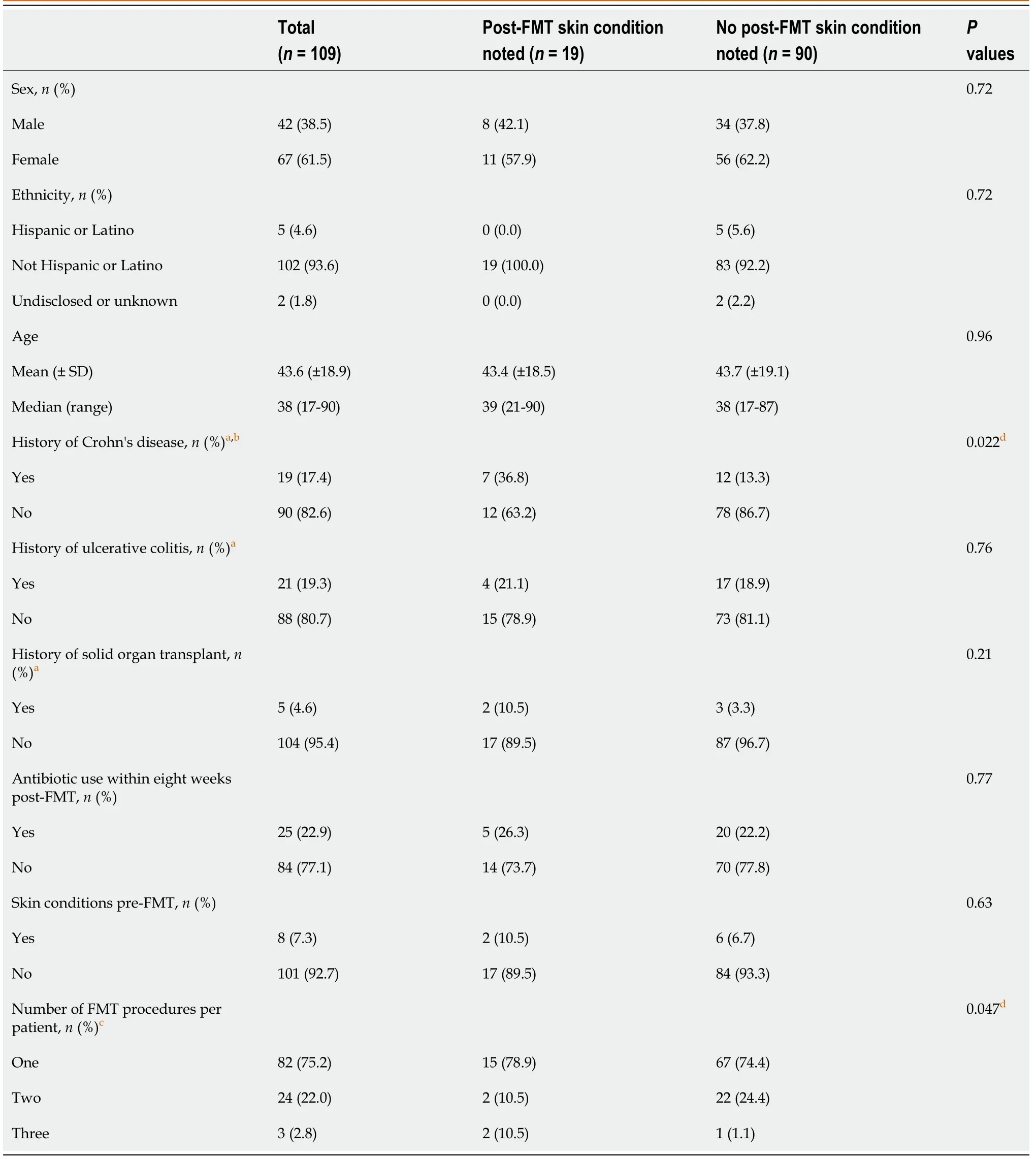
Table 1 Demographics of fecal microbiota transplant patients
Manipulating the mouse gut microbiome with antibiotics has also been shown to affect melanoma tumor growth given how the immune system was impacted[11,21].It is possible for antibiotics to impact immune system responsesviaeffects on the gut microbiome,and this can subsequently impact colonization resistance that would otherwise protect the body against certain infectious diseases,such asC.difficile–the bacterial species that is the primary reason for administering FMT[22].Some autoimmune disorders have been associated with antibiotics and the gut microbiome[23].However,it is still unclear how much antibiotics play a part in these conditions when considering other exposures,including medical interventions (such as delivery methods during the birth process),lifestyle,diet,and certain infectious diseases which have also been explored regarding their impact on the gut microbiome and subsequent impact on autoimmune disease[23].
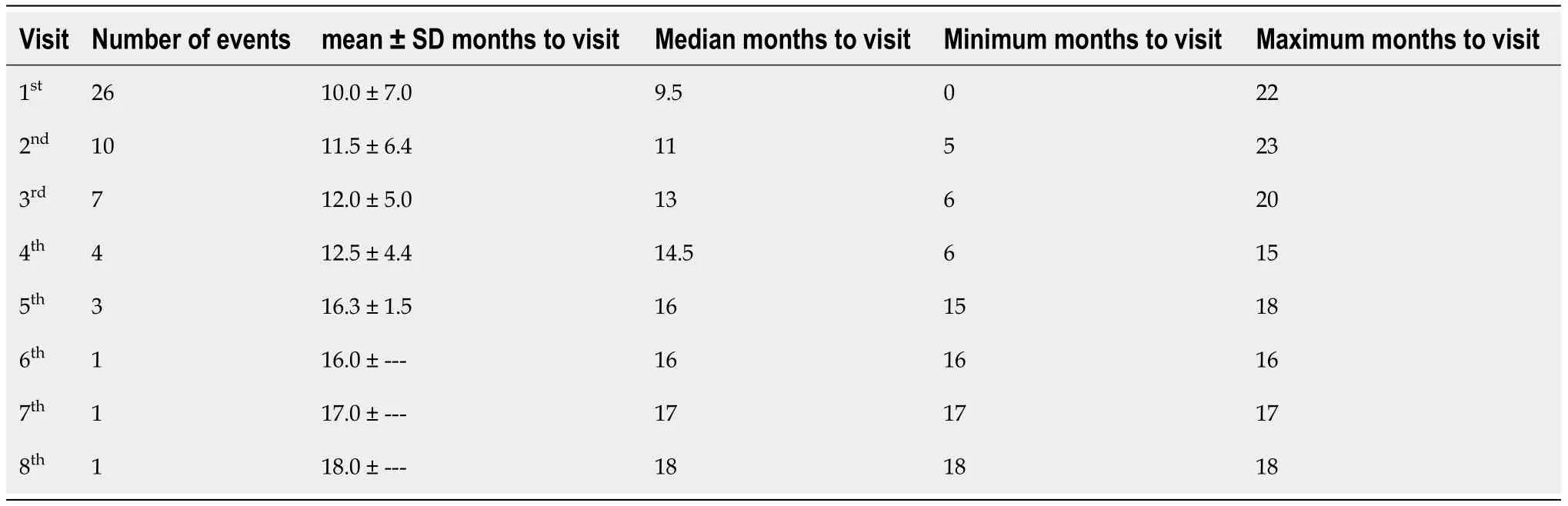
Table 2 Months between fecal microbiota transplant events and dermatology visits

Figure 1 Months after fecal microbiota transplant when new diagnoses were made
Given this evidence,it is plausible that effects on the immune system,whether due to FMT or other means of altering the gut microbiome,could impact infectious and inflammatory skin conditions.Interestingly,there was a wide variety of infectious and inflammatory skin conditions noted in our study,though many of these were unique to individual patients.Thus,our results do not suggest that FMT leads to flaring of specific acute or chronic dermatologic conditions,but given the limited evidence,we cannot identify clear cause-and-effect relationships between skin diseases and FMT.
Our study was limited by its retrospective nature.Most patients who received FMT at University of Utah Health did not have a follow-up dermatology office visit on record,and we cannot be certain that patients did not visit dermatologists at other healthcare institutions.Of note,some FMT procedures were fairly recent as of the time this report was written,and so this factor could have contributed to the lack of dermatology visits for some patients.There was no clear indication of FMT-induced changes in skin conditions for most patients,but for the same reasons we cannot assume there were associations,we cannot assume that there was no FMT-induced change.
Most diagnoses were made after the first six months post-FMT,which makes it difficult to determine whether the noted dermatologic conditions were influenced by FMT or other factors,such as antibiotics.In one study,most microbial species recovered within 1.5 mo after an antibiotic cocktail of meropenem,gentamicin,and vancomycin,though certain species did not recover even after 180 d[24].Another study found that microbial compositions remained changed up to four months after one course of clindamycin and up to 12 mo after one course of ciprofloxacin[25].Our study could assess treatments prescribed at our institution but cannot confirm through retrospective analysis that some patients did not receive antibiotics elsewhere if not reported in our EMR.We did find that use of antibiotics within eight weeks post-FMT was not common for our overall sample and did not differ significantly between those with or without a reported post-FMT skin condition.Thus,using only the records in our system,it would seem that antibiotics did not play a significant role in disease development.It is still reasonable to assume that any benefits from FMT could later have been offset by exposure to other factors in the months and years when post-FMT dermatology visits were conducted,and in our study,we limited the time frame of dermatology follow-up to two years after FMT to account for these other factors,given evidence that microbial changes from FMT may last up to two years[6,14].However,this time frame could also be a limitation.
Of further note,we did not conduct analyses on diet.Previous research indicates that the gut microbiome can be influenced by different aspects of diet[26-29],including use of probiotics[30],and so dietary factors would be important to assess where possible.However,using the EMR alone does not provide much detail to assess diet and dietary changes,and with the amount of time that passed before most of the dermatology office visits,we cannot confirm that dietary changes would not have impacted outcomes post-FMT.Further study involving dietary interventions or questionnaires would be needed to address how diet might be associated with the gut microbiome and subsequent skin disease.
Another significant limitation is that we were not able to find enough information on stool donors to determine how all donors were screened or whether donors had any of the noted skin conditions and could have transferred a disease-inducing microbial composition to recipients.Generally,stool donors might be screened for gastrointestinal diseases,certain pathogens,etc.related to overall health or gastroenterology concerns,but there is not much emphasis on screening for a broad range of dermatologic conditions[31].Overall,our study simply does not have enough data to be certain these other factors did not impact disease development or even the lack thereof post-FMT.
CONCLUSION
Potential associations between FMT and skin disease should be investigated to further elucidate the association between skin disease and the gut microbiome and to further understand how FMT might be of use for treating infectious and inflammatory skin conditions.Though dermatologic assessment might not seem important for treatment of aC.difficileinfection,FMT can affect more than just gastrointestinal disease.Better documentation of skin conditions before and after FMT are needed to perform more effective retrospective studies on this subject.Where possible,prospective studies may be necessary to ascertain better evidence of cause-and-effect relationships between FMT and skin disease as the complexity of the gut microbiome and environmental factors that influence it makes it difficult to find enough information retrospectively.Finally,clinicians administering FMT should be aware of the potential for dermatologic changes in their patients after FMT,and we encourage them to consider referring their FMT patients to a dermatologist for addressing dermatologic concerns.
ARTICLE HIGHLIGHTS
Research background
This retrospective cohort study was completed to evaluate the impact of fecal microbiota transplant (FMT) on skin disease,a subject not currently well-studied.
Research motivation
FMT has grown in popularity as a possible treatment for diseases beyond recurrent Clostridioides difficile infections,and there is growing evidence that FMT could be a treatment for skin disease.Overall,the goal was to assess potential patterns of skin disease that could be notable for future research on FMT.
Research objectives
To determine the impact of F MT on the development of skin disease post-FMT and identify pitfalls in dermatologic care that could impact future studies on this relatively underexplored subject.
Research methods
A retrospective chart review was conducted on all patients whom received FMT between January 2013 to December 2019 at a single academic medical center.Dermatologic follow-up was assessed for the two years after FMT or through March 2020 for more recent procedures.Dermatology visits and inflammatory and infectious dermatologic diagnoses were recorded.
Research results
The most common diagnoses were dermatophyte,wart(s),and dermatitis.Mean time to first dermatology visit was 10.0 (± 7.0) mo.Overall,no apparent FMT-related trends in skin disease were observed.Little information on the condition of most patients’skin pre- and post-FMT was captured in the electronic medical record.Thus,more information is needed on dermatology visits and particularly visits within the first few months post-FMT.
Research conclusions
Due to the extended interval between FMT and dermatology visits,it was difficult to assess whether reported diseases were affected by or resulted from FMT.While FMT could potentially have clinically significant effects on certain skin diseases,this study was limited by its retrospective nature and could not find clear patterns of post-FMT skin disease.It was concluded that prospective studies may be the best avenue for further assessing the relationship between FMT and skin disease.
Research perspectives
Future research will need to address temporality of dermatologic visits after FMT to provide a better indication of the effect on skin disease.Ideally,dermatologic followup should occur within two months post-FMT.Given limitations of the electronic medical record,prospective studies will need to be conducted to assess future relationships between FMT and skin disease.
