Hallux rigidus treated with adipose-derived mesenchymal stem cells:A case report
2021-02-23AdrianoBraileGiuseppeToroAnnalisaDeCiccoAntonioBenedettoCecereFabioZanchiniAlfredoSchiavonePanni
Adriano Braile, Giuseppe Toro, Annalisa De Cicco, Antonio Benedetto Cecere, Fabio Zanchini, Alfredo Schiavone Panni
Adriano Braile, Giuseppe Toro, Annalisa De Cicco, Antonio Benedetto Cecere, Fabio Zanchini, Alfredo Schiavone Panni, Department of Medical and Surgical Specialties and Dentistry, University of Campania “Luigi Vanvitelli”, Naples 80138, Italy
Abstract BACKGROUND First metatarsophalangeal joint arthritis (FMTPA), also known as hallux rigidus, is the most frequent degenerative disease of the foot. Diagnosis is made through both clinical and radiological evaluation. Regenerative medicine showed promising results in the treatment of early osteoarthritis. The aim of the present study was to report the results of a case of FMTPA treated with the injection of autologous adipose-derived mesenchymal stem cells.CASE SUMMARY A gentleman of 50 years of age presented with a painful hallux rigidus grade 2 resistant to any previous conservative treatment (including nonsteroidal antiinflammatory drugs and hyaluronic acid injections). An injection of autologous adipose-derived mesenchymal stem cells into the first metatarsophalangeal joint was performed. No adverse events were reported, and both function and pain scales improved after 9 mo of follow-up.CONCLUSION The FMTP joint injection of mesenchymal stem cells improved symptoms and function in our patient with FMTPA at 9 mo of follow-up.
Key Words: First metatarsophalangeal joint arthritis; Hallux rigidus; Stem cells; Regenerative medicine; Early osteoarthritis; Adipose derived-mesenchymal stem cells; Case report
INTRODUCTION
First metatarsophalangeal joint arthritis (FMTPA), also known as hallux rigidus, is the most frequent degenerative arthritis disease of the foot[1].Depending on the severity of the disease, the symptoms in the case of FMTPA are pain, gait discomfort, articular effusion, and a reduction in range of motion. The diagnosis is generally completed by observing the typical findings of osteoarthritis (OA) revealed by X-rays. Coughlin and Shurnas proposed a classification for FMTPA based on both clinical features and imaging[2](Table 1).
Different types of treatments had been proposed, both conservative [i.e., orthosis, nonsteroidal anti-inflammatory drugs, hyaluronic acid (HA) injections] and operative (i.e.,cheilectomy, arthroplasty, arthrodesis)[3].
Recently, emerging evidence has supported the use of autologous adipose-derived mesenchymal stem cells (aAMSCs) for the treatment of early OA[4-7].
The aim of the present study was to report the clinical results of a case of FMTPA treated with the injection of aAMSCs.
CASE PRESENTATION
Chief complaints
A gentleman of 50 years of age presented with a painful FMTP joint in the left foot.
History of present illness
His symptoms were resistant to both nonsteroidal anti-inflammatory drugs and HA injections.
History of past illness
The patient was already scheduled for an aAMSCs injection due to right knee Kellgren-Lawrence grade 2 OA.
Personal and family history
Personal and family history were negative for foot pathologies.
Physical examination
The clinical examination showed a positive axial grind test and joint pain, exacerbated by the dorsiflexion that impaired the patient’s ability to walk.
Laboratory examinations
Laboratory tests did not support the final diagnosis.
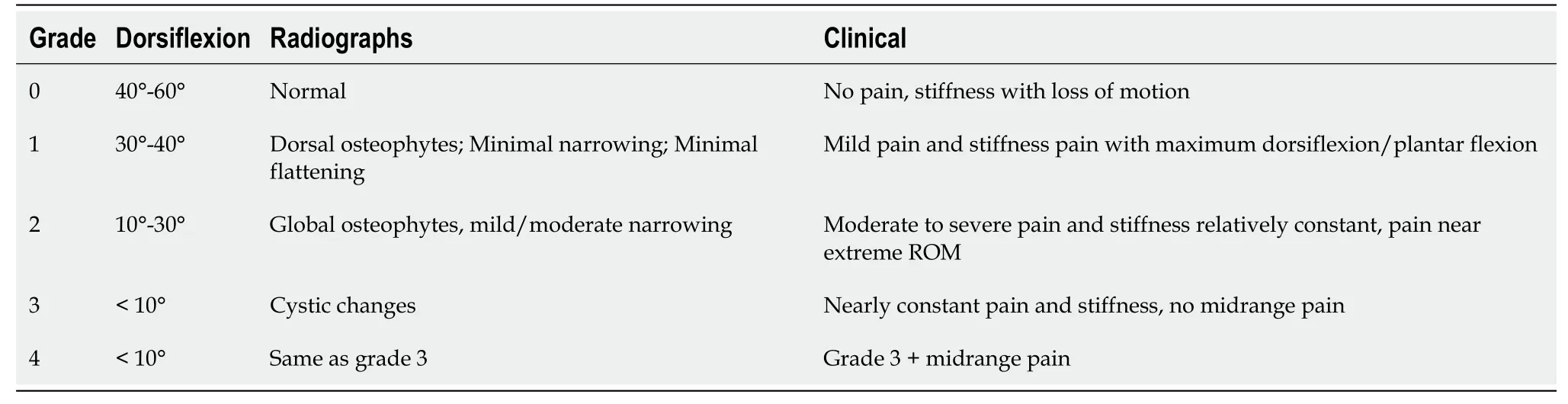
Table 1 Coughlin and Shurnas clinical and radiographic classification of hallux rigidus
Imaging examinations
Antero-posterior and latero-lateral standard X-rays showed FMTPA stage 2.
FINAL DIAGNOSIS
FMTPA stage 2 was diagnosed.
TREATMENT
The patient was already scheduled for an aAMSCs injection due to right knee Kellgren-Lawrence grade 2 OA, and therefore a similar injection was proposed to treat the hallux rigidus.
Concentrated aAMSCs were obtained from the abdomen, filtered as previously reported[5], and then injected into the FMTP joint after its distraction (Figure 1).
Protected weight bearing was prescribed during the first week after the procedure.
OUTCOME AND FOLLOW-UP
The patient was followed up at regular intervals. The clinical evaluation was completed using both the American Orthopedic Foot and Ankle Society (AOFAS) for hallux metatarsophalangeal-interphalangeal scale and the Visual Analog Scale (VAS).
No adverse effects were reported, excluding a transient pain in the FMPT joint in the first week after surgery. During the entire follow-up, an improvement in both VAS and AOFAS scales were observed (Table 2), leading to a final VAS scale of 0 and an AOFAS of 78 at 9 mo of follow-up.
DISCUSSION
Recently, the use of regenerative medicine principles has been proposed for various applications in both trauma and orthopedics, and especially for the treatment of early OA[4-6,8-11]. While conventional therapies for early OA (i.e.physical therapy, glucosamine and chondroitin sulfate supplementation) showed little benefits, regenerative medicine was demonstrated to be a promising option, due to the paracrine, anti-apoptotic, anti-inflammatory, and anti-aging effects of stem cells[12,13].
aAMSCs showed some theoretical advantages over other sources of stem cells. In fact, aAMSCs are easy to harvest, because of the wide availability of adipose tissue, and their sampling is generally associated with minimal discomfort, considering that it can be carried out using local anesthesia[7]. Moreover, aAMSCs demonstrated a high capacity for proliferation and fibroblastic differentiation[14]. Hasset al[15]showed that adipose tissue should be considered a primary source of cells for regenerative medicine as it contains 500 times more MSCs than the same volume of bone marrow.
Emerging literature has underlined the role of aAMSCs in the treatment of early OA. Schiavone Panniet al[5]conducted a study of 52 patients with early knee OA treated with arthroscopic debridement and aAMSCs injection, and showed improvement in both function and pain at an average of 15.3 mo of follow-up.Similarly, Songet al[16]reported the amelioration of pain, function and cartilage volume of the knee after multiple injections of aAMSCs. The efficacy of aAMSCs in OA was recently confirmed in a systematic review conducted by McIntyreet al[17].
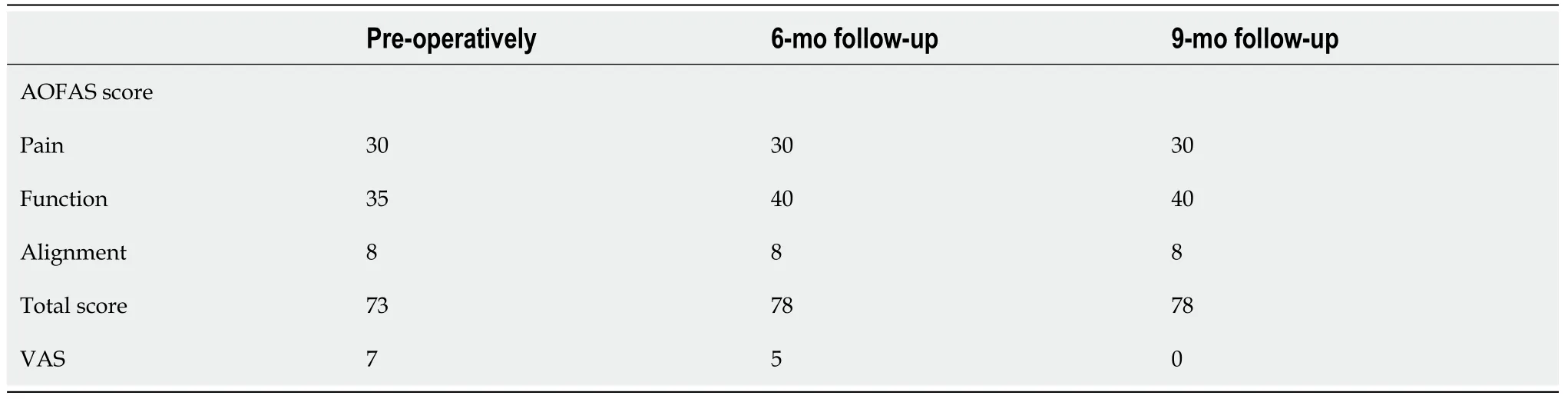
Table 2 American Orthopedic Foot and Ankle Society and Visual Analog Scale scores

Figure 1 Intraoperative picture showing the autologous adipose-derived mesenchymal stem cells injection into the first metatarsophalangeal joint.
FMTPA is a degenerative disease with an incidence of 2.5% in patients over 50 years of age. Its treatment might be frustrating for both the orthopedic and the patient, considering the conflicting outcomes reported after conservative treatment, including HA injections. Petrellaet al[18]in their study of 47 patients with FTMPA, described the long-term improvement in both pain and function after multiple HA injections; however, Munteanuet al[19]in their randomized controlled trial did not observe any differences when HA was compared with placebo.
Ponset al[20]in a randomized study compared the use of sodium hyaluronate with triamcinolone acetonide in FMTPA, and reported an improvement in pain relief and function at 3 mo after the injections. However, a high percentage of patients in both groups required subsequent surgery after 1 year of follow-up, due to further progression of the disease with worsening of both pain and function.
To the best of our knowledge, this is the first report on the use of aAMSCs for FMTPA. A single injection was effective in treating FMTPA, improving both the AOFAS and VAS score at 9 mo of follow-up.
CONCLUSION
The present case report indicates that the injection of aAMSCs might be a promising treatment for FMTPA. Obviously, larger cohorts and longer follow-up studies are needed to confirm these findings.
杂志排行
World Journal of Orthopedics的其它文章
- Ceramic-on-ceramic vs ceramic-on-polyethylene, a comparative study with 10-year follow-up
- Hello, can you hear me? Orthopaedic clinic telephone consultations in the COVID-19 era- a patient and clinician perspective
- Thirty-day mortality of patients with hip fracture during COVID-19 pandemic and pre-pandemic periods: A systematic review and metaanalysis
