COVID-19 or non-COVID viral pneumonia: How to differentiate based on the radiologic findings?
2021-01-13AzadehEslambolchiAnaMaligligAmitGuptaAliGholamrezanezhad
Azadeh Eslambolchi, Ana Maliglig, Amit Gupta, Ali Gholamrezanezhad
Abstract Influenza viruses were responsible for most adult viral pneumonia. Presently,coronavirus disease 2019 (COVID-19) has evolved into serious global pandemic.COVID-19 outbreak is expected to persist in months to come that will be synchronous with the influenza season. The management, prognosis, and protection for these two viral pneumonias differ considerably and differentiating between them has a high impact on the patient outcome. Reverse transcriptase polymerase chain reaction is highly specific but has suboptimal sensitivity. Chest computed tomography (CT) has a high sensitivity for detection of pulmonary disease manifestations and can play a key-role in diagnosing COVID-19. We reviewed 47 studies and delineated CT findings of COVID-19 and influenza pneumonia. The differences observed in the chest CT scan can be helpful in differentiation. For instance, ground glass opacities (GGOs), as the most frequent imaging finding in both diseases, can differ in the pattern of distribution.Peripheral and posterior distribution, multilobular distribution, pure or clear margin GGOs were more commonly reported in COVID-19, whereas central or peri-bronchovascular GGOs and pure consolidations were more seen in influenza A (H1N1). In review of other imaging findings, further differences were noticed.Subpleural curvilinear lines, sugar melted sign, intra-lesional vascular enlargement, reverse halo sign, and fibrotic bands were more reported in COVID-19 than H1N1, while air space nodule, tree-in-bud, bronchiectasia, pleural effusion, and cavitation were more seen in H1N1. This delineation, when combined with clinical manifestations and laboratory results may help to differentiate these two viral infections.
Key Words: Coronavirus; COVID-19; Computed tomography; Viral pneumonia; H1N1;Influenza
INTRODUCTION
Community-acquired pneumonia is a major public health concern, as it is the most common infectious disease worldwide and a significant cause of morbidity and mortality. Although bacteria have been a major cause of pneumonia in adults,respiratory viruses are increasingly implicated recently. In some instances, they are found to be higher in incidence than bacterial etiologies. Prior to the emergence of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), influenza virus was the most common cause of viral pneumonia in adults. It has been an important health challenge of recent history. Influenza type A (H1N1) is the most common type of influenza viruses. It is also the most significant in terms of morbidity and mortality in the general population.
In late December 2019, a new viral pneumonia emerged in China that rapidly disseminated worldwide. On February 11, 2020, the International Committee on Taxonomy of Viruses termed this new variant, SARS-CoV-2 and World Health Organization (WHO) labelled the disease caused by this virus as corona virus disease of 2019 (COVID-19 virus). WHO designated this outbreak a public health emergency of international concern on January 30, 2020, and declared it as a global pandemic on March 11, 2020.
The COVID-19 outbreak is ongoing and is expected to persist a period more than a year. There is evidence that it may wax and wane, with a new incidence rise in late fall and winter months within temperate regions. This timing will coincide with influenza season. Upper and lower respiratory infections due to influenza virus will also loom again in the form of common cold, pneumonias, and possible unpredictable epidemics in the next few months. This can be overwhelming, particularly for healthcare systems in resource-limited contexts. Public health officials and clinicians,therefore, will be compelled to differentiate pneumonia caused by COVID-19 and influenza viruses. The impact of intercurrent infection of two viral pneumonias due to simultaneous seasonal peak occurrences in some individuals raises great concern.
Although clinical manifestations of these two respiratory viruses may have similarities, the approach with respect to health care worker precautions, treatment,and prognosis are different. Reverse transcriptase polymerase chain reaction (RT-PCR)with high specificity, is now the confirmatory and reference standard for COVID-19 diagnosis; this method is also highly accurate for detecting influenza. However,suboptimal test sensitivity for COVID-19 has led to false negative results, failure to detect infected patients, and created challenges in decision making for suspected cases. Studies have shown that chest computed tomography (CT) with its high sensitivity and availability can play a key role in diagnosing COVID-19, particularly in the early stages of the disease when even RT-PCR can be negative. However,resources comparing chest CT findings of COVID-19 and influenza pneumonia, in search of differentiating characteristics of each, are of great scarcity. Therefore, given the emerging role of imaging in diagnosis of these novel viral infections with low reliability of clinical symptoms, and sub-optimal performance of RT-PCR, we have explored the added benefit of chest CT in better differentiation of COVID-19 and influenza pneumonia.
DIAGNOSTIC APPPROACH
Pulmonary infection with different viruses usually demonstrates common symptoms particularly in the early stages of the disease, although signs and symptoms can vary between individual patients. Clinical manifestations are diverse but have considerable overlap. In the Wangcomparison of the symptoms of COVID-19 and influenza pneumonia, the most common clinical manifestations were fever, cough, and malaise.Other frequently reported symptoms were sputum production, rhinorrhea, dyspnea,headache, nausea and vomiting, chest pain, fatigue, sore throat, and diarrhea.Although the range of symptoms in COVID-19 and H1N1 are similar, the fraction of patients with severe disease differs significantly and the proportion of severe and critical infection in COVID-19 is higher than anticipated for influenza infection. In COVID-19, 80% of infections are asymptomatic or mild, 15% are severe, requiring oxygen therapy and 5% are critical, requiring ventilation aid. As the signs and symptoms of either influenza or COVID-19 pulmonary disease cannot be used with sufficient confidence to confirm a specific viral etiology, health care providers are challenged to make a timely diagnosis for effective management. Clinical characteristics of patients with COVID-19 and Influenza are summarized in Table 1.
Traditionally, diagnosis of viral pneumonia has been based on evaluation of respiratory tract samples and detection of the virus or its antigens by culture or immunofluorescence microscopy. Measurement of the antibodies in patients’ serum has been another useful diagnostic method. Invention of PCR has enhanced the power of detection of the causative factor of viral pneumonia. Although various PCR methods such as RT, quantitative, or real time are the most specific methods for diagnosis of viral pneumonia, their sensitivity is not optimal for all viruses (, 79%for COVID-19).
Recent studies have shown that chest CT with high sensitivity is a helpful modality in the early identification of pneumonia. Combination of PCR and chest CT can improve the sensitivity and specificity for diagnosing clinically suspected cases.Additionally, radiation dose can be decreased - particularly for children and pregnant women- with low radiation dose protocols with greater than 50% decrease in ionizing radiation exposure and no significant impact on the diagnostic assessment.
Prior to the emergence of the new SARS-CoV-2 virus, other known viruses were among common causes of respiratory tract infection. In immunocompetent adults,influenza virus and human parainfluenza virus (HPIV) were the most common,followed by adenovirus and respiratory syncytial virus (RSV). In immunocompetent children, RSV and HPIV were the most common causative agents for viral pneumonia,followed by parainfluenza and human metapneumovirus (HMPV).
In addition to RT-PCR, serologic tests are also helpful in supporting the diagnosis of H1N1 pneumonia. Increased levels of C-reactive protein (CRP), serum lactate dehydrogenase (LDH, can reach more than 1000 IU/L and is correlated with the severity of disease), and creatine kinase are reported in H1N1. Lymphopenia,thrombocytopenia, and elevated level of transaminase can also occur. Similarly in COVID-19, increased level of CRP, LDH, aspartate aminotransferase and alanine aminotransferase, and lymphopenia has been reported. In imaging-based diagnosis,viral pneumonias generally show more diffuse and bilateral pattern of involvement with greater preponderance of interstitial findings when compared to bacterial pneumonias. The latter more commonly demonstrate unilateral, segmental, or lobar consolidations, limited by pleural surfaces, centrilobular nodules, bronchial wall thickening and mucus impaction. Viral agents have similar virulence factors andunderlying mechanism of invasion by causing alveolar and bronchiolar injury,hemorrhage and inflammatory responses that lead to interstitial cellular infiltration,and edema. The radiologic features of viral pneumonia also demonstrate similarities concomitant with their similar means of pathogenesis.
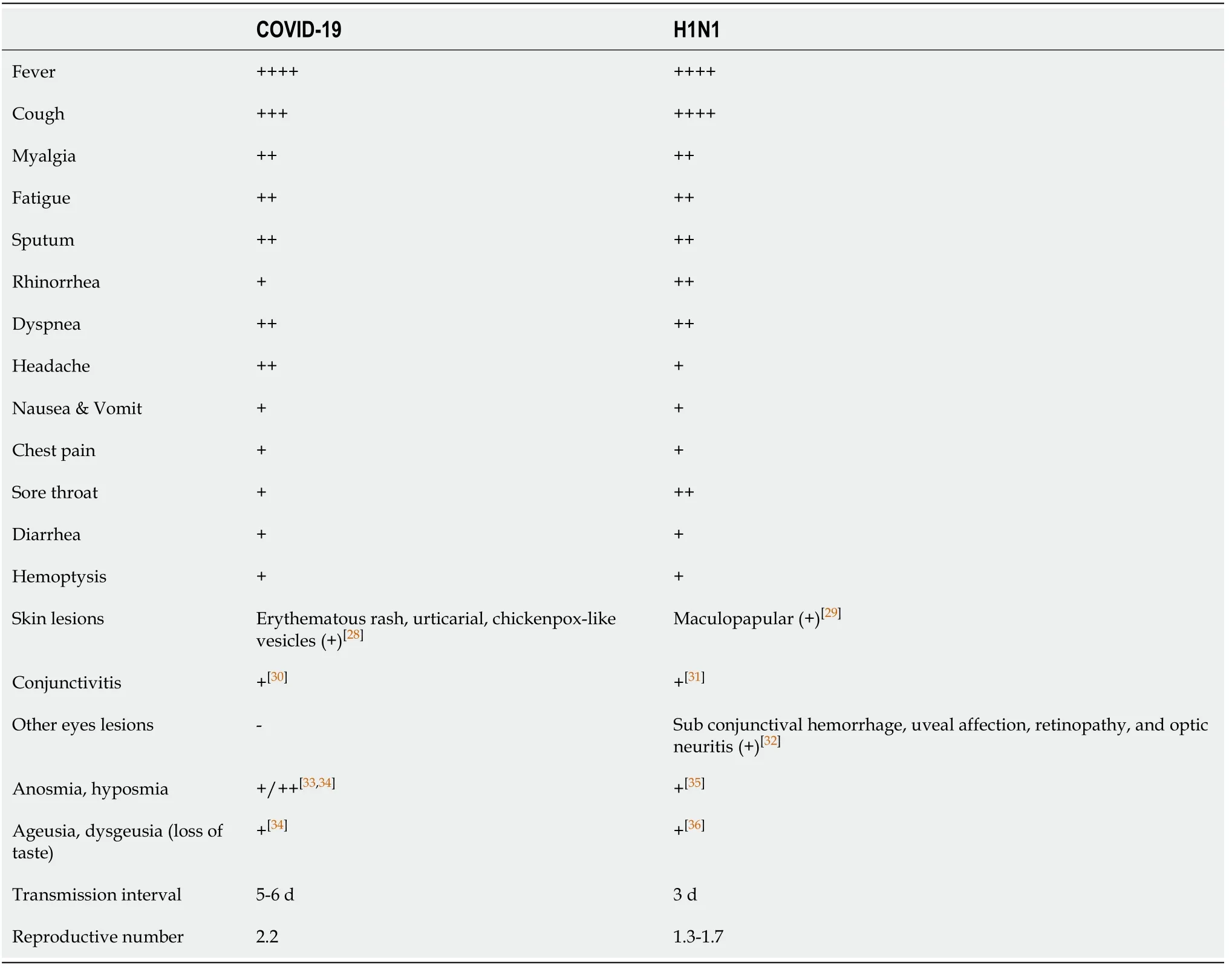
Table 1 Clinical features of coronavirus disease 2019 and influenza A[11,18,20-27]
The main CT findings of viral pneumonia include changes in pulmonary parenchymal density with areas of ground glass opacity (GGO) or consolidation,nodular, or micro nodular opacities, sometimes with tree-in-bud pattern, reticular opacities as inter- or intra-lobular septal thickening and signs of bronchiolar inflammation as evidenced by increased thickness of bronchial wall. However, some viral infections may have some distinctive features in chest imaging. For example,adenovirus invades terminal bronchioles causing bronchopneumonia.Cytomegalovirus leads to acute interstitial pneumonia with diffuse edema and alveolar exudate, exhibiting diffuse GGOs and interstitial reticular opacities or may exhibit nodular infiltration (Figure 1). Herpes simplex virus invades both the airways and alveoli leading to multifocal scattered airspace opacities and consolidations mainly in peribronchial distribution (Figure 2). Varicella-zoster virus exhibits well defined or ill- defined tiny nodules with or without surrounding halo or patchy bilateral GGOs. On the healing process, the lesions can calcify and persist as randomly scattered calcified nodules (Figure 1). However, this appearance is not specific and, in appropriate clinical context, can be seen with various other conditions, such as pulmonary hemosiderosis, Goodpasture syndrome, silicosis, pulmonary alvelolar microlithiasis, and in some calcified metastasis, such as osteosarcoma.
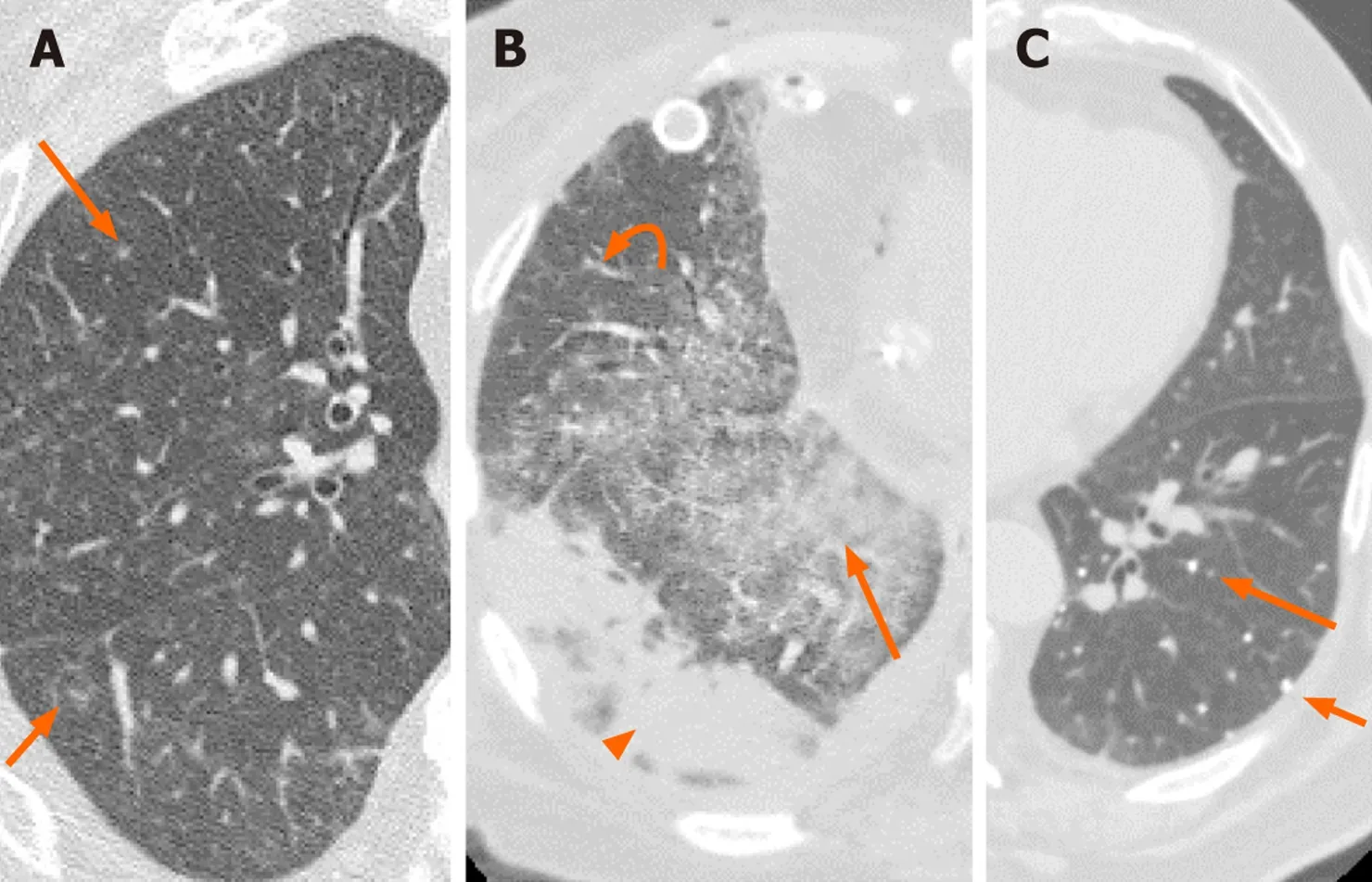
Figure 1 Two patients with double lung transplants and cytomegalovirus pneumonia diagnosed via transbronchial biopsy and lavage respectively. A: Axial chest computed tomography (CT) in a 67-year-old male shows numerous nodular infiltrates (arrows); B: The CT for a 56-year-old female shows ground glass opacities (arrow), reticular opacities (curved arrow) and sub pleural consolidation (arrowhead); C: The third patient is a 76-year-old male with a history of varicella pneumonia. There are numerous small calcified nodules (arrows). However, this appearance can also be seen in pulmonary hemosiderosis,Goodpasture syndrome, silicosis, pulmonary alveolar microlithiasis, and calcified metastasis.

Figure 2 A 37-year-old female with a history of double lung transplant presented with progressive dyspnea. Axial computed tomography of the chest demonstrates bronchocentric multifocal opacities (black circles; A-C). Transbronchial lung biopsy demonstrated herpes simplex virus pneumonia.
Chest CT features of HPIV, RSV, and HMPV can be similar and include multifocal patchy GGOs, consolidation, centrilobular nodules, and bronchial wall thickening.Influenza virus usually involves lung parenchyma extensively, leading to diffuse and multifocal parenchymal lesions. Influenza pneumonia can be classified into different types based on parenchymal changes that include interstitial pneumonia with patchy GGOs and interlobular septal thickening as the main findings; bronchopneumonia with multifocal consolidations more along the bronchovascular bundles; and an uncommon type histologically consistent with cryptogenic organizing pneumonia (COP). Diffuse parenchymal damage can be indicated by peribronchovascular interstitial thickening and air space or centrilobular nodules; the latter may demonstrate the “tree-in-bud” pattern that is usually associated with small airways disease and/or endobronchial spread of disease. Bronchial wall thickening and centrilobular nodules (including tree-in-bud) are signs of bronchiolitis or bronchitis; GGOs, consolidations, and crazy-paving (thick septal line over areas of GGOs or consolidation) pattern indicate parenchymal involvement of pneumonia.Although there is no specific CT for diagnosing H1N1, the main suggestive findings are scattered lung consolidations, GGOs, or both in a z or peripheral distributing pattern, air bronchograms, and septal thickening (Figure 3). Crazy paving, halo sign(GGO surrounding a consolidation), nodules, irregular lines of fibrotic change associated bronchiectasis, round mass-like opacity, pleural effusion, and adenopathy are more uncommon findings.
In COVID-19 pneumonia, the main CT features are pure GGOs, GGO with superimposed consolidation, bronchiolar wall thickening, rounded opacities, and interlobular septal thickening (Figure 4-6). GGOs, as the most frequent finding, are mainly seen as bilateral and multifocal opacities, with peripheral and posterior distribution. Pure consolidations are less common and can be seen later in the course of the disease or in older ages.
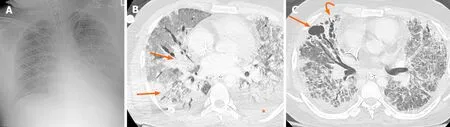
Figure 3 A 33-year-old man with hypoxic respiratory failure, requiring intubation was polymerase chain reaction positive for influenza A.A: Radiograph shows diffuse granular opacities resembling pulmonary interstitial edema; B: A contemporaneous axial computed tomography (CT) (arrows) shows diffuse ground glass opacities with patchy consolidations that are both in peripheral and central zones. Pleural effusion (asterisk) is more common in influenza A pneumonia than coronavirus disease 2019 (COVID-19); C: Axial CT two months later demonstrates cavitation (arrow) and traction bronchiectasis (curved arrow)which are not frequently reported in COVID-19.
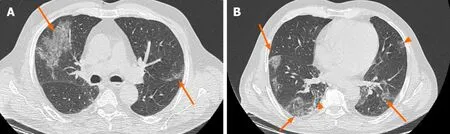
Figure 4 A 72-year-old man presented with fever, dry cough and shortness of breath. Polymerase chain reaction was positive for severe acute respiratory syndrome coronavirus 2 infection. A and B: Axial chest computed tomography shows bilateral peripheral ground glass opacities (arrows; A and B) and superimposed reticulation (arrowhead; B), consistent with coronavirus disease 2019 pneumonia.
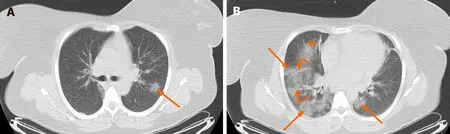
Figure 5 A 46-year-old woman presented with fever and dry cough. Polymerase chain reaction was positive for severe acute respiratory syndrome coronavirus 2 infection. A and B: Axial chest computed tomography shows bilateral multifocal ground glass opacities (arrows; A and B), peribronchial interstitial thickening (arrowhead; B) and reticular opacities (curved arrows; B), consistent with coronavirus disease 2019 pneumonia.
IMAGING-BASED DIFFERENTIATION
By reviewing the literature and comparing CT findings of COVID-19 and H1N1 pneumonia, the following information was extracted and charted in Table 2; important differences are annotated (). Although both infections commonly involve multiple lobes bilaterally, GGOs were more common in patents with COVID-19, while consolidations were more common in H1N1. In COVID-19, mainly peripheral and posterior zones were involved, whereas in H1N1 pneumonia, the pattern of involvement was more diffuse with both central and peripheral involvement. It is noteworthy that in the advanced stage of COVID 19 infection, the imaging findings become non-specific and indistinguishable from other pneumonias.
The incidence of air space nodules ranges widely in reviewed studies. However,most studies demonstrated that air space nodules and tree-in-bud nodules (as clustered 1-4 mm nodules with a linear branching pattern) were more frequently seen in H1N1. Some combination of simultaneous findings can be more suggestive for each.For example, pure GGOs, interlobular septal thickening, and the absence of nodules and pleural effusions were more suggestive of COVID-19. The incidence of interlobular septal thickening was equivocal in the reviewed literature. These findings were more commonly reported in COVID-19 than H1N1. The discrepant incidence of interlobular septal thickenings has been postulated to reflect evaluation of patients in different stages of disease. Interstitial disease appears to present in latter and more advanced stages of disease. Subsegmental vascular enlargement is a unique and not uncommon finding observed COVID-19 patients. This finding is not greatly reported in H1N1 pneumonia. Therefore, its appearance may be more specific for COVID-19, especially if observed with imaging manifestations that support a diagnosis of COVID-19.
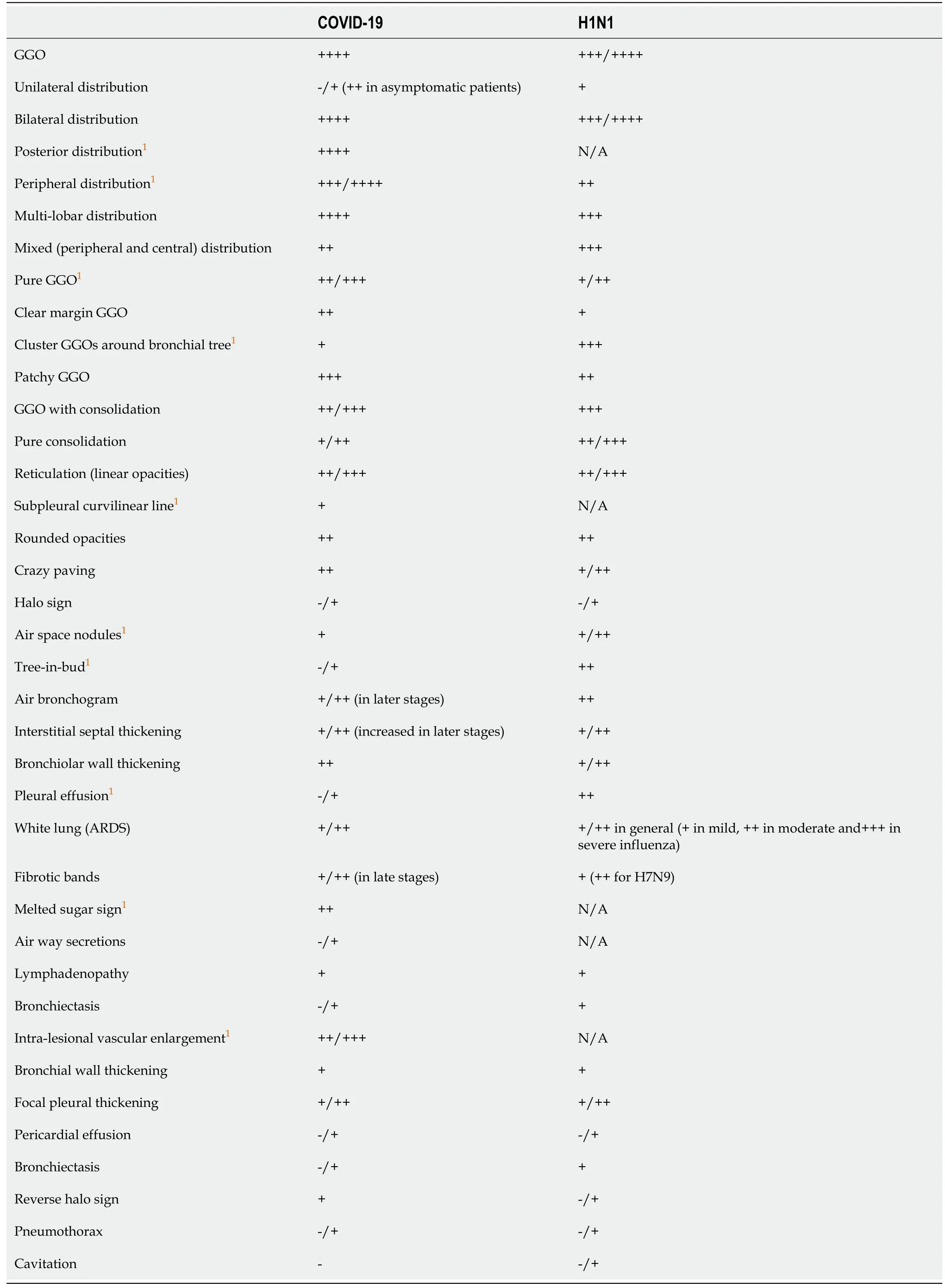
Table 2 Comparison of chest computed tomography findings of coronavirus disease 2019 and influenza A[18,43,47-51,53-73]
Another non-specific CT finding is interstitial thickening within areas of GGOs - the“crazy paving” disease pattern, which was more reported in COVID-19 patients.Reticular opacities refer to opacification in or around interstitial septal structures.Causes of interstitial thickening include edema, fibrosis, and other parenchymal opacification around septal lines (including GGOs) can cause reticular opacifications.This definition may explain why the reviewed literature report more linear opacities than septal thickening in COVID-19 patients. However, this finding is not an uncommon finding in H1N1 as well. Fibrotic lines with appearance of linear opacities were reported at a higher rate at the third week after H1N1 pneumonia; these findings can resolve slowly over time.
Reverse halo sign (consolidation surrounding central GGO was reported previously in few infectious diseases such as TB, invasive pulmonary aspergillosis,pneumonia, histoplasmosis, and cryptococcosis or in non-infectious granulomatosis diseases such as sarcoidosis, granulomatosis with polyangiitis, and COP. This CT sign is also reported in COVID-19 patients. In a study by Zhaothe reverse halo sign was observed in 25.2% of COVID-19 patients. Such finding suggests that organizing pneumonia can be one of the mechanisms for parenchymal damage in COVID-19. This finding was reported in relatively fewer cases of H1N1. It is not uncommon for consolidations in both COVID-19 and H1N1 to present as a round opacity. In few studies the incidence of round opacity was slightly higher in COVID-19 than H1N1. In a study by Liuthe combination of round opacity with absence of nodule was significantly more in COVID-19 than in H1N1.They found some other statistically significant combination of CT findings in favor of COVID-19 included the presence of pure GGO with absence of nodules; GGO and septal thickening; septal thickening and absence of nodules; and the combined presence of rounded opacities, septal thickening, and the absence of pleural effusion.
In a follow up evaluation of patients with H1N1, evidence of traction bronchiectasis was reported in some cases in the regions of previous consolidation suggestive of fibrotic changes. This finding appears to be rare in COVID-19, although it was reported in few cases. No cavitation has been reported in COVID-19 patients thus far; these are rarely reported in influenza, especially in more severe forms of avian influenza (H5N1). Cavitation was described in a case report of an immunocompromised patient with H1N1.
Focal pleural thickening in the setting of other suggestive COVID-19 findings is not uncommon; however, pleural effusion is an atypical finding for COVID-19. Pleural effusions have been reported in some H1N1 patients. Mediastinal lymphadenopathy is an atypical finding in both COVID and H1N1; however, it was more reported in influenza especially in younger ages and in children. Pneumothorax is a rare finding in both COVID-19 and H1N1. Just few cases with this finding as the complication of COVID-19 or during recovery phase of H1N1 have been reported in literature.
CONCLUSION
COVID-19 and influenza pneumonia have relatively similar clinical manifestations.However, the precautions required of the public and health workers to prevent transmission, the disease management protocols, and prognosis are quite different.Therefore, differentiating COVID-19 and influenza pneumonia is important in the early stages of the infection for a well-timed and appropriate management plan. There are imaging features of influenza and COVID-19 that sufficiently differ such that the two may be distinguishable. However, even in cases where CT findings have overlap,the addition of clinical history, lab data (including RT-PCR) has potential to improve diagnostic accuracy.
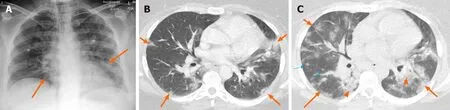
Figure 6 A 35-year-old previously healthy woman presented with fever, dry cough and shortness of breath 10 d after contact with a sick person with coronavirus disease 2019. A: Radiograph shows haziness (arrows) in basilar portions; B: Axial chest computed tomography (CT) in the same day demonstrates bilateral multifocal ground glass opacities (GGOs) (arrows) in favor of coronavirus disease 2019 infection that was confirmed with positive reverse transcriptase polymerase chain reaction. The patient’s condition worsened and she was intubated; C: Follow-up CT after 3 d shows progression of GGOs (arrows),superimposed consolidations (arrowheads), and ill-defined nodular opacities (thin arrows). Ultimately, her condition improved and she was discharged in a good condition after 20 d.