Endoscopic retrograde cholangiopancreatography guided interventions in the management of pancreatic cancer
2021-01-11MuhammadNadeemYousafHamidEhsanAhsanWahabAhmadMuneebFizahChaudharyRichardWilliamsChristopherHaas
Muhammad Nadeem Yousaf,Hamid Ehsan,Ahsan Wahab,Ahmad Muneeb,Fizah S Chaudhary,Richard Williams,Christopher J Haas
Muhammad Nadeem Yousaf,Hamid Ehsan,Fizah S Chaudhary,Richard Williams,Christopher J Haas,Department of Medicine,Medstar Union Memorial Hospital,Baltimore,MD 21218,United States
Muhammad Nadeem Yousaf,Fizah S Chaudhary,Richard Williams,Christopher J Haas,Department of Medicine,MedStar Good Samaritan Hospital,Baltimore,MD 21239,United States
Muhammad Nadeem Yousaf,Fizah S Chaudhary,Richard Williams,Christopher J Haas,Department of Medicine,Medstar Franklin Square Medical Center,Baltimore,MD 21237,United States
Muhammad Nadeem Yousaf,Fizah S Chaudhary,Richard Williams,Christopher J Haas,Department of Medicine,MedStar Harbor Hospital,Baltimore,MD 21225,United States
Ahsan Wahab,Department of Hospital Medicine,Baptist Medical Center South,Montgomery,AL 36116,United States
Ahmad Muneeb,Department of Medicine,Faisalabad Medical University,Faisalabald 38000,Punjab,Pakistan
Abstract Pancreatic cancer is the leading cause of cancer-related morbidity and mortality with an overall five-year survival of less than 9% in the United States.At presentation,the majority of patients have painless jaundice,pruritis,and malaise,a triad that develops secondary to obstruction,which often occurs late in the course of the disease process.The technical advancements in radiological imaging and endoscopic interventions have played a crucial role in the diagnosis,staging,and management of patients with pancreatic cancer.Endoscopic retrograde cholangiopancreatography(ERCP)-guided diagnosis(with brush cytology,serial pancreatic juice aspiration cytologic examination technique,or biliary biopsy)and therapeutic interventions such as pancreatobiliary decompression,intraductal and relief of gastric outlet obstruction play a pivotal role in the management of advanced pancreatic cancer and are increasingly used due to improved morbidity and complication rates compared to surgical management.In this review,we highlight various ERCP-guided diagnostic and therapeutic interventions for the management of pancreatic cancer.
Key Words:Pancreatic cancer;Endoscopic retrograde cholangiopancreatography;Malignant stricture;Biliary drainage;Biliary stent;Gastric outlet obstruction
INTRODUCTION
While pancreatic cancer is the 13thmost common type of cancer globally,it is the fourth leading cause of cancer-related death in the United States with an estimated 55600 new cases and 47050 deaths in 2020[1].Despite ongoing advances in the diagnosis and management of pancreatic cancer,its five-year survival rate is less than 9% due to a notable absence of symptoms in the early stages of the disease and relatively late patient presentation at a time when patients already have an advanced disease[1,2].When symptomatic,the extent of signs and symptoms vary depending on the size and location of the tumor(head,body,or tail)[3].Painless jaundice secondary to biliary obstruction is one of the most common presenting manifestations of pancreatic cancer involving the head of the pancreas,uncinate process,and occasionally the body of the pancreas in cases of locally advanced malignancy.Other clinical presentations include abdominal/epigastric pain,weight loss,anorexia,and fatigue.Cancers involving the head of the pancreas are detected at an earlier stage(1/3 in stage I)due to obstructive cholestasis,whereas cancer involving the body or tail of the pancreas often remains asymptomatic until stage IV at the time of diagnosis[3].
Pancreatic cancers originate from both exocrine(ductal adenocarcinoma,intraductal papillary mucinous neoplasm(IPMN)with invasive behavior,mucinous cystic neoplasms,and adenosquamous carcinoma)and endocrine components(neuroendocrine cancers).Pancreatic ductal adenocarcinoma is the most common exocrine malignancy,responsible for 83% of cases followed by IPMN,6% of cases[4].Pancreatic ductal adenocarcinoma is the most common pancreatic cancer associated with extrahepatic bile duct obstruction,resulting in jaundice during the course of its disease.Progressive biliary obstruction may result in cholestasis,pruritis,and if unchecked may result in malabsorption,liver failure,and premature mortality.Biliary decompression,therefore,has a crucial role in the management of pancreatic cancer.Among patients who have resectable pancreatic cancer,a preoperative biliary decompression is suggested[5].Palliation with biliary decompression is also critical to relieving symptoms among those with advanced or unresectable cancer[5].Percutaneous transhepatic or endoscopic retrograde cholangiopancreatography(ERCP)-guided biliary drainage are the most common interventions used in the management of pancreatic cancers associated with biliary obstruction.Endoscopic ultrasound(EUS)is an emerging intervention that is increasingly utilized in the management of pancreatic cancers.In this review,we specifically focus on the role of ERCP in the diagnosis and management of pancreatic cancer.
ERCP-GUIDED DIAGNOSTIC INTERVENTIONS
ERCP is a commonly performed diagnostic and therapeutic procedure in the management of pancreatobiliary disorders.Endoscopy is often combined with fluoroscopy and contrast medium,permitting a detailed visualization of the anatomy of the pancreatobiliary ductal systems.With the advancement of diagnostic imaging modalities such as high-resolution computed tomography and magnetic retrograde cholangiopancreatography,coupled with the significant risk of post-ERCP pancreatitis,the use of diagnostic ERCP has decreased.Cross-sectional radiological imaging is helpful for the identification and characterization of pancreatobiliary masses.Recently published consensus guidelines recommended ERCP-guided biliary sampling for an unresectable mass when there is a concurrent need for biliary decompression,however,for resectable masses,or when ERCP tissue acquisition unsuccessful,EUS-guided fine needle biopsy is preferred[6].The capability of EUS in obtaining tissue samples for pathological staining and diagnosis of pancreatic malignancy has shifted the role of ERCP primarily to therapeutic interventions[7-9].Indeed,the diagnostic yield of EUS is comparable to ERCP and carries a markedly reduced risk of complications.Multiple prospective and retrospective studies focusing on individuals with pancreatic cancer have shown the overall superior diagnostic yield of EUS over ERCP with a range of sensitivity of 43%-94%(median 81%)vs13%-81%(median 52%)and specificity of 93%-100%(median 100%)vs75%-100%(median 100%)(Table 1)[10-17].In a recent RCT,Leeet al[18]showed 96.7% sensitivity for diagnosis of malignancy in extrinsic type biliary stricture(due to pancreatic cancer)by using a combined approach of initial ERCP-guided transpapillary biliary biopsy(ERCP-TPB)followed by EUS-guided fine needle biopsy in those negative for malignancy on initial ERCP-TPB.For intrinsic(biliary tract cancer)biliary stricture,an initial and followed up ERCP-TPB are adequate in diagnosis of malignancy with a 96.6% sensitivity[18].ERCP,in contrast,allows for the opportunity to perform both intervention and diagnosis in the same procedure – pancreatobiliary drainage and specimen collection for cytopathology.In case of known or suspected pancreatic cancer,ERCP is used in the management of biliary obstruction.Cytological and histological specimens for pathological diagnosis are essential in the management of pancreatic cancer,guiding the selection of chemoradiation therapy,and ERCP-mediated procedures such as ERCP-guided brush cytology,needle aspiration,or forceps biopsy are occasionally utilized.Fluoroscopy guided biliary brush cytology,biliary biopsy,and cholangioscopy-guided biopsy are the most common ERCP techniques for tissue acquisition.
ERCP-guided biliary brush cytology
Biliary brush cytology is obtained by advancing 8 French(Fr)cytology brush over a guidewire beyond the stricture using a specialized catheter.The brush is moved back and forth across the stricture to obtain an adequate sample.The brush is then withdrawn into the catheter before removal of the endoscope and catheter as a unit to improve the diagnostic yield of a sample and prevent contamination.A series of prospective and retrospective studies including 1285 patients with malignant biliary strictures has shown the sensitivity of brush cytology sample obtained from the bile duct ranged from 30% to 78%(median 54%)with a specificity of 97% to 100%(median 100%)for the diagnosis of malignant biliary strictures(Table 2)[10,15,19-37].To increase the diagnostic yield of brush cytology,various technical modifications have been evaluated.Farrellet al[38]compared brushing alone with a combined approach of stricture dilation coupled with endoscopic aspiration with 22-gauge needle and brushing and demonstrated an increased diagnostic yield of cytology with a sensitivity of 57%vs85%(P<0.02)and a specificity of 80%vs100%,with the standard and modified techniques,respectively.Overall,biliary brushing is a safe technique associated with minimal risk of adverse events such as pancreatitis and bile duct perforation.
ERCP-guided endobiliary forceps biopsy
Fluoroscopic-guided biliary biopsy improves the diagnostic yield over simple biliary brush cytology by obtaining biliary tissue sampling deeper to the epithelial layer.It can be performed by passing 5-Fr to 10-Fr biopsy forceps at the lower edge of stricture.The specimen can be collected at the level of stricture by opening and closing the biopsy forceps under the guidance of fluoroscopy.While the optimal number of individual biopsy specimens remains a matter of contention,general protocol suggests a minimum of three tissue samples to establish the diagnosis of malignant stricture[30,39,40].A series of 19 prospective and retrospective studies on 1101 patients with malignant biliary strictures evaluated with endobiliary forceps biopsy have shown that sensitivity ranges from 36% to 81%(median 61%)with specificity from 90% to 100%(median 100%)for the diagnosis of malignant biliary strictures(Table 3)[10,15,26,29,30,34-37,41-51].The diagnostic yield is much higher with the combination of forceps biopsy and brush cytology with a pooled sensitivity of 63% to 86% and a specificity of 97% to 100%[30,52].Despite the increased sensitivity and specificity,forceps biopsy remains technically challenging and a user-dependent procedure,and as such is less commonly performed than brush cytology.Indeed,it is related to a number of unique adverse events,such as bleeding and perforation of common hepatic duct,secondary to a variety of factors – forceps size and stiffness,number of biopsy passes,and the technical capability of the endoscopist[20,30,44].
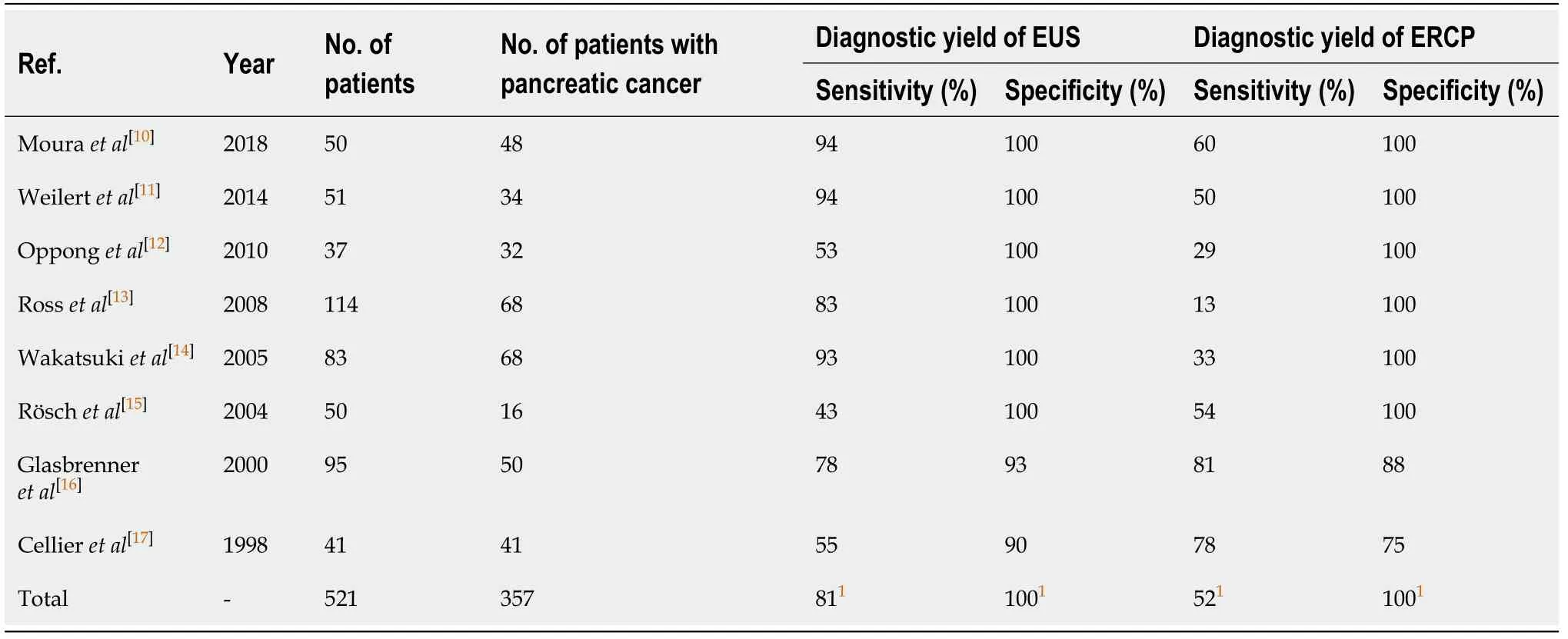
Table 1 Prospective/retrospective studies comparing the overall yield of endoscopic ultrasound and endoscopic retrograde cholangiopancreatography in the diagnosis of pancreatic cancer
Cholangiopancreatoscopic-guided biopsy
Cholangiopancreatoscopy involves direct luminal visualization of the biliary and pancreatic ductal systems.Conventionally,it was performed by two endoscopists using a mother-daughter per-oral scope setup where one endoscopist handle ERCP scope while other endoscopist operate a fragile scope within biopsy channel of main ERCP scope.The introduction of ultraslim gastroscope loaded with anchoring balloon(a slight modification in this technique)enabled a single operator to perform this procedure without issues of scope fragility.Novel intraductal visualization techniques employing the Spyglass system have augmented diagnostic yield by permitting the endoscopist the opportunity to obtain targeted tissue under direct visualization.This system involves the use of a disposable SpyScope with a tip-deflecting access catheter,working catheter,SpyBite biopsy forceps,and two irrigation channels enabling a single operator to perform the procedure.Cholangioscopy-guided biopsy can be performed by advancing a cholangioscope through the biopsy channel of a duodenoscope,enabling direct visualization and biopsy of a biliary stricture.The classic cholangioscopic features of malignant biliary strictures are cholangioscopic visualization of intraductal nodules surrounded by tortuous,irregularly dilated blood vessels,and the presence of papillary or villous mucosal projections[53,54].ERCP-guided cholangioscopy has increased the diagnostic yield of bile duct biopsy by allowing the collection of suspected neoplastic tissue under direct visualization.In cases of main pancreatic duct IPMN,a premalignant condition of the pancreas,ERCP-guided pancreatoscopy with biopsy may be helpful in making the diagnosis,particularly due to its classic,pathognomonic features fish egg-like,villous and prominent mucosal protrusions which carry a sensitivity of 68% and a specificity of 87%[55-57].Cholangioscopy is 88% to 100% sensitive and 77% to 92% specific for the diagnosis of pancreatobiliary malignancy[54,58-62].Common complications with cholangiopancreatoscopy are bile duct perforation,hemorrhage,air embolization,pancreatitis,and cholangitis.The overall risk of complications with this modality is higher than ERCP,therefore,the utility of cholangiopancreatoscopy is reserved for selected cases of inaccessible ductal lesions[63].
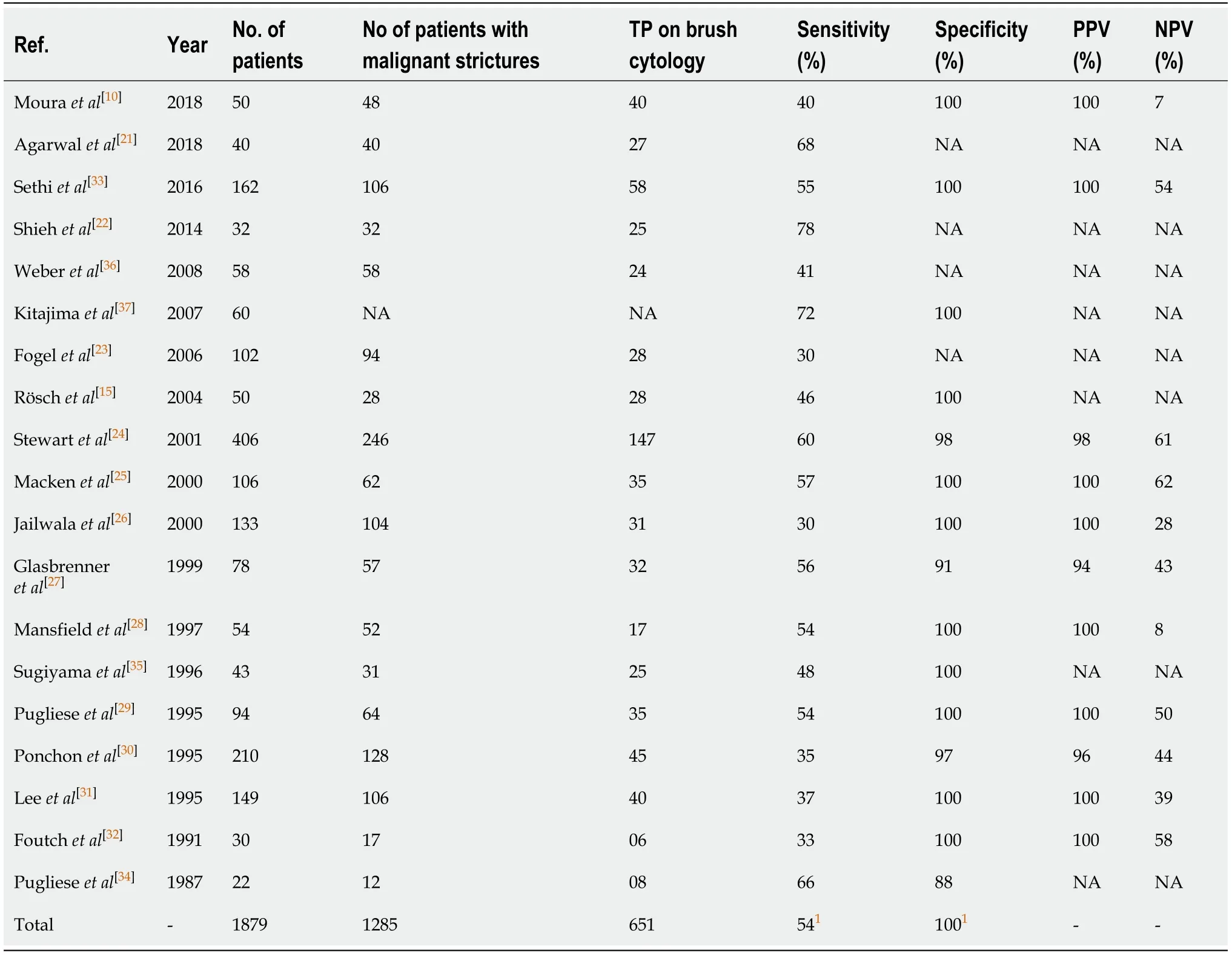
Table 2 Prospective/retrospective studies on the diagnostic yield of endoscopic retrograde cholangiopancreatography guided brush cytology for malignant biliary stricture
ERCP-guided naso-pancreatic drainage
ERCP-guided naso-pancreatic drainage(ENPD)is a method to collect pancreatic juice using a specialized drainage catheter compatible with standard duodenoscope.ENPD was first implemented by Endoet al[64]in 1974 for cytodiagnosis of pancreatic cancer.A slight modification of the standard ENPD technique wherein pancreatic juice collection is performed after injection of synthetic secretin,has been shown to provide a dedicated sample with a sufficient number of cells for cytological analysis and has improved the diagnostic sensitivity from 50.9% to 70.4%[65].Of note,in this study,an additional 13 pancreatic cancer patients were diagnosed using the modified ENPD technique that were missed with EUS-fine needle aspiration(EUS-FNA),making the modified ENPD technique preferred,particularly in instances where tissue collection with EUS-FNA is unsuccessful or impossible[65].Another modification of ENPD involving placement of a 4 or 5 Fr tube(with 8-12 hole)in the main pancreatic duct and collection of pancreatic juice 2-6 times daily for up to 3 d has increased the diagnostic yield for detection of pancreatic cancer with 80% sensitivity,100%specificity,100% positive predictive value,71% negative predictive value,and 87%overall accuracy[66].Iiboshiet al[67]reported similar results of ENPD with 100%sensitivity,83.3% specificity,and 95% accuracy in the diagnosis of in situ pancreatic cancer.For pancreatic cancers smaller than 1 cm,the diagnostic yield of EUS-FNA is limited.ERCP-guided serial pancreatic juice aspiration cytologic examination(SPACE)technique is a promising modality that may be superior to EUS-FNA for diagnosing pancreatic cancer at early stages(stage 0 and stage I)[68].A multicenter Japanese study on 200(51 with stage 0 and 149 with stage I)pancreatic cancer patients has shown a better cytological confirmation of stage 0 pancreatic cancer using ERCP-guided SPACE technique as compared to EUS-FNA(72%vs17%).In contrast,for stage I pancreatic cancer,EUS-FNA has been shown to be superior to ENPD(84%vs60%)[69].Post-ENPD pancreatitis and cholangitis are the commonly reported complications[65].
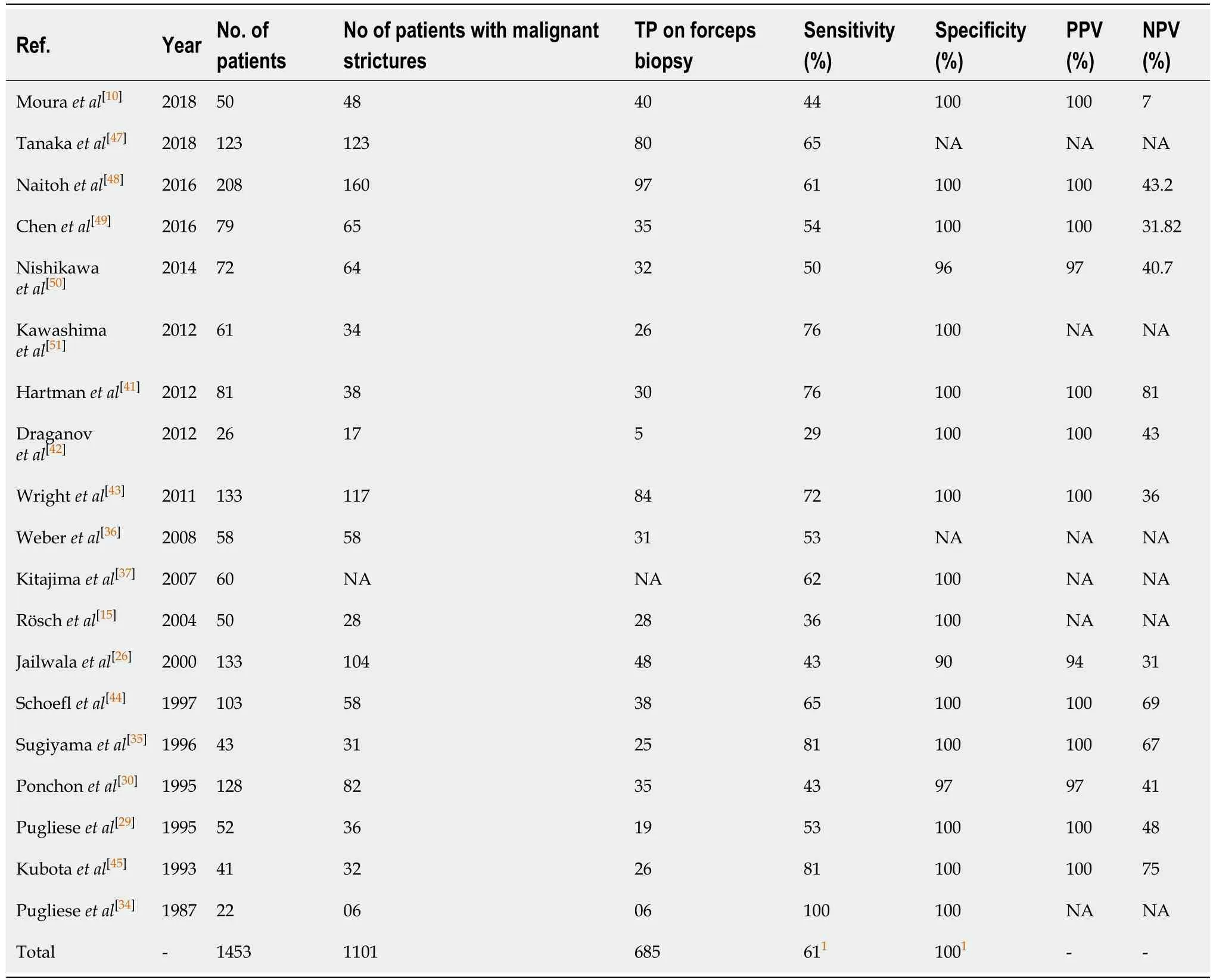
Table 3 Prospective/retrospective studies on the diagnostic yield of fluoroscopic guided endobiliary forceps biopsy for malignant biliary stricture
ENDOSCOPIC RETROGRADE-GUIDED THERAPEUTIC INTERVENTIONS
ERCP-guided biliary decompression
While 15% of pancreatic cancer patients are candidates for surgical resection,preoperative biliary decompression may be required.It is also a commonly employed feature in these individuals for palliation.ERCP-guided biliary drainage or decompression with transpapillary stenting is the mainstay of management for patients with biliary obstruction and its related complications.In patients with advanced pancreatic malignancy,endoscopic and surgical biliary drainage showed similar success rate and long-term symptomatic relief[70,71].Endoscopic biliary decompression,however,is minimally invasive,more convenient,and relatively safer than surgical bypass for biliary decompression,especially for patients with unresectable pancreatic cancer[72].Endoscopic decompression is associated with fewer complications,shorter hospital stays,lower cost,and better quality of life.
Indications
A recent cross-sectional study on 411409 inpatient ERCP procedures revealed that malignant biliary obstruction was the fourth most common indication for ERCP in the past decade,with balloon dilation or stenting of biliary or pancreatic strictures often performed[7].Indeed,with these interventions,there is a noted improvement of pruritus,jaundice,and known complications of malignant biliary obstruction such as acute cholangitis and renal dysfunction[73].Preoperative ERCP-guided biliary decompression is a preferred approach for patients who encounter delays in surgical intervention due to a decision to initiate neoadjuvant therapy and in those with severe malnourishment requiring nutritional support[74-76].In unresectable pancreatic cancer,ERCP-guided transpapillary biliary stenting not only improves patient’s symptoms and quality of life but is also associated with reduced mortality and morbidity[77].
Technical accessibility and consideration
The procedural feasibility of ERCP-guided transpapillary biliary stenting is above 90%with a short term efficacy in terms of symptomatic relief of over 80%[78,79].Sphincterotomy with adjunctive guidewire rather than standard catheter for biliary canalization is associated with rapid access to the bile duct,a higher success rate(85%to 95%),and lower risk of complications[80,81].ERCP-mediated biliary decompression can be performed by the deployment of either a self-expandable metal stent(SEMS)or plastic stent over the guidewire threaded across a malignant stricture.Stent selection depends on several factors such as the level of biliary dysfunction,the need for reintervention,complication rate,cost,and the likelihood of short- and long-term patient survival[82].SEMS have a significantly lower risk of complications and stent dysfunction compared with plastic stents[82].A recent meta-analysis showed a lower rate of stent dysfunction,subsequent rate of reinterventions,and longer median survival for SEMS when compared with plastic stents[83].Compared to percutaneous and surgical biliary decompressions,ERCP-mediated biliary stenting not only improved patient symptoms and quality of life but was also associated with reduced mortality and morbidity[77].In cases of unsuccessful ERCP-transpapillary biliary stenting,EUS-guided biliary drainage with transmural stenting has been increasingly used as an alternative option for palliation in malignant biliary obstruction[6].A recent meta-analysis(10 studies including 3 RCT)compared the efficacy of EUS-guided biliary decompression with ERCP in the palliation of malignant biliary obstruction and demonstrated a similar technical(94.8%vs96.5%)and clinical(93.8%vs95.7%)success rates respectively[84].
Types of biliary stents
Plastic stents:Plastic biliary stents are usually made of polyethylene,polyurethane,or Teflon that are available in different sized diameters including 7,8.5,10 and 11.5 Fr and lengths ranging from 5 cm to 15 cm.Large diameter stents are preferable because of better flow rate,infrequent stasis,and decreased incidence of stent occlusion.These stents are designed into various shapes - straight,curved,single,or double pigtails.The introduction of sidewall anchoring flaps and pigtails on either end of the stent prevents stent migration.The choice of stent depends upon multiple factors including the likely etiology of the lesion,as well as location and length of the biliary stricture.Plastic stents are preferred for benign lesions,whereas metal stents are favored in malignant lesions.Plastic stents offer the benefit of ease of deployment,abrogate the need for biliary sphincterotomy,and are less expensive in the management of individuals with shorter life expectancy[85,86].Plastic stents also have a more limited duration of patency and often require stent exchange every 10 to 12 wk to circumvent stent occlusion,thus making them a relatively unfavorable therapeutic option for the management of malignant biliary obstruction in those with a longer life expectancy.A large RCT has shown an overall superiority of metal stents over plastic stents in managing patients with longer survival times,whereas no differences in the rate of adverse events and mortality were reported[87].
Self-expanding metal stents:Endoscopic biliary SEMS employ a large diameter stent(8-10 mm),which has been shown to significantly reduce the risk of stent occlusion(approximately 50% lower than plastic stents)while not completely eliminating the risk of complete obstruction[82].SEMS are manufactured as fully-covered or partiallycovered devices.While the original SEMS were comprised of uncovered metal[stainless steel,nitinol(a mixture of titanium and nickel)] or platinol(a combination of the platinum core with encasement of nitinol),which reduced the risk of stent migration,but these were associated with significant stent dysfunction secondary to tumor ingrowth or occlusive biliary sludge,which when coupled with the limited ability to remove these metal stents,created major disadvantages and further complications.To address these issues,second-generation SEMS were manufactured as partially-covered or fully-covered devices with a polyurethane,polycaprolactone,or silicone membrane that resulted in a significantly lower risk of tumor ingrowth and reduced difficulties associated with stent retrieval/removal.Despite these advances,fully-covered biliary SEMS pose several challenges such as higher risks of stent migration,pancreatitis,and cholecystitis.Furthermore,fully-covered SEMS have several specific anatomical restrictions,primarily due to their covered nature.For example,proximal biliary lesions at the level of hilum have unique anatomical considerations specifically related to biliary drainage from intrahepatic side branches.As such in this scenario,partially-covered SEMS are preferred over fully-covered SEMS particularly as lesions become more proximal,as partially-covered SEMS would allow effective drainage of the intrahepatic side branches through fenestrations of uncovered portions of the stent.Multiple RCT and retrospective studies have shown the superiority of uncovered SEMS over covered SEMS for long-term stent patency,however no significant difference in patency between two SEMS after 6 and 12 mo,and no difference in patient survival or complication rates such as pancreatitis,cholangitis,cholecystitis,perforation,bleeding,length of hospital stay,and incidence of recurrent biliary obstruction(Table 4)[47,88-106].Taken together,uncovered SEMS are associated with higher rates of stent dysfunction due to tumor ingrowth whereas covered SEMS have a higher rate of stent migration and a lower risk of sludgemediated occlusion(Table 4)[47,88-106].Overall,no difference was observed in the rates of pancreatitis and cholecystitis between covered and uncovered SEMS[47,88-106].
Compared to plastic stents,metal stents are 15-30 times more expensive and technically difficult to deploy[82].SEMS provides longer stent patency(6 to 9 mo)than plastic stents(3 to 4 mo).Multiple studies have shown no significant difference in technical or therapeutic success rates,complication rates,and 30 d mortality,however,these studies did show a lower rate of stent occlusion and overall risk of obstruction for uncovered SEMS at four-months[85].The selection of biliary stent subtype depends on multiple factors including life expectancy,risk of complications,cost,and the need for ERCP-guided reinterventions(if needed)for stent replacement / manipulation.
Safety and complications of ERCP-guided biliary decompression:ERCP-guided biliary drainage is a relatively safe,minimally invasive intervention compared to percutaneous or surgical biliary decompression.It is however associated with several complications including post-ERCP pancreatitis,cholangitis,cholecystitis,biliary ductal perforation,stent migration or obstruction,liver abscess,and hemorrhage[107,108].Several factors have been associated with higher complication rates such as degree of obstructive jaundice,previous gastrointestinal surgeries,and multiple comorbidities[109-112].Such high-risk patients have demonstrated an increased risk of post-ERCP complications and are managed conservatively with rectal indomethacin or diclofenac,adequate hydration,nutritional support,and early use of antibiotics.After plastic biliary stenting,close follow up is required for early identification of recurrent biliary obstruction due to stent occlusion.For those patients with a longer life expectancy(more than 3 mo)and when close follow up is impossible,scheduled stent exchange is required[6].In case of biliary decompression using SEMS,on demand biliary reintervention is recommended based on clinical judgement[6].
ERCP-guided preoperative biliary drainage for resectable pancreatic cancers
The role of preoperative biliary drainage(PBD)in the management of resectable pancreatic cancer is still controversial.Routine PBD is not recommended,however,in cases of pruritus or cholangitis,biliary stenting can be considered following interdisciplinary consultation[6].Factors such as liver dysfunction,hyperbilirubinemia,coagulopathy,and cholangitis correlate with the severity of biliary obstruction and are associated with deleterious effects on renal or cardiovascular function,malnutrition,and an increased risk of postoperative morbidities[111,112].Therefore,some surgeons recommend PBD before performing a Whipple procedure for symptomatic relief and associated prevention of complications due to cholestasis in patients with obstructive jaundice.In a retrospective study,Coateset al[113]compared the impact of PBD on short term(90 d)postoperative outcome and demonstrated a need for repeat surgical intervention in patients who underwent pancreatoduodenectomy without preoperative ERCP,with no significant difference in the rate of complications,hospital stay,and 30-90 d mortality between two groups.PBD also prepares the patient for neoadjuvant chemotherapy due to improved liver function test and the relative contraindication to chemotherapy use with hyperbilirubinemia after relieving biliary obstruction.However,PBD was criticized in several studies because of reported increased morbidity,mortality,prolonged hospital stay after preoperative biliary stenting[114-116].
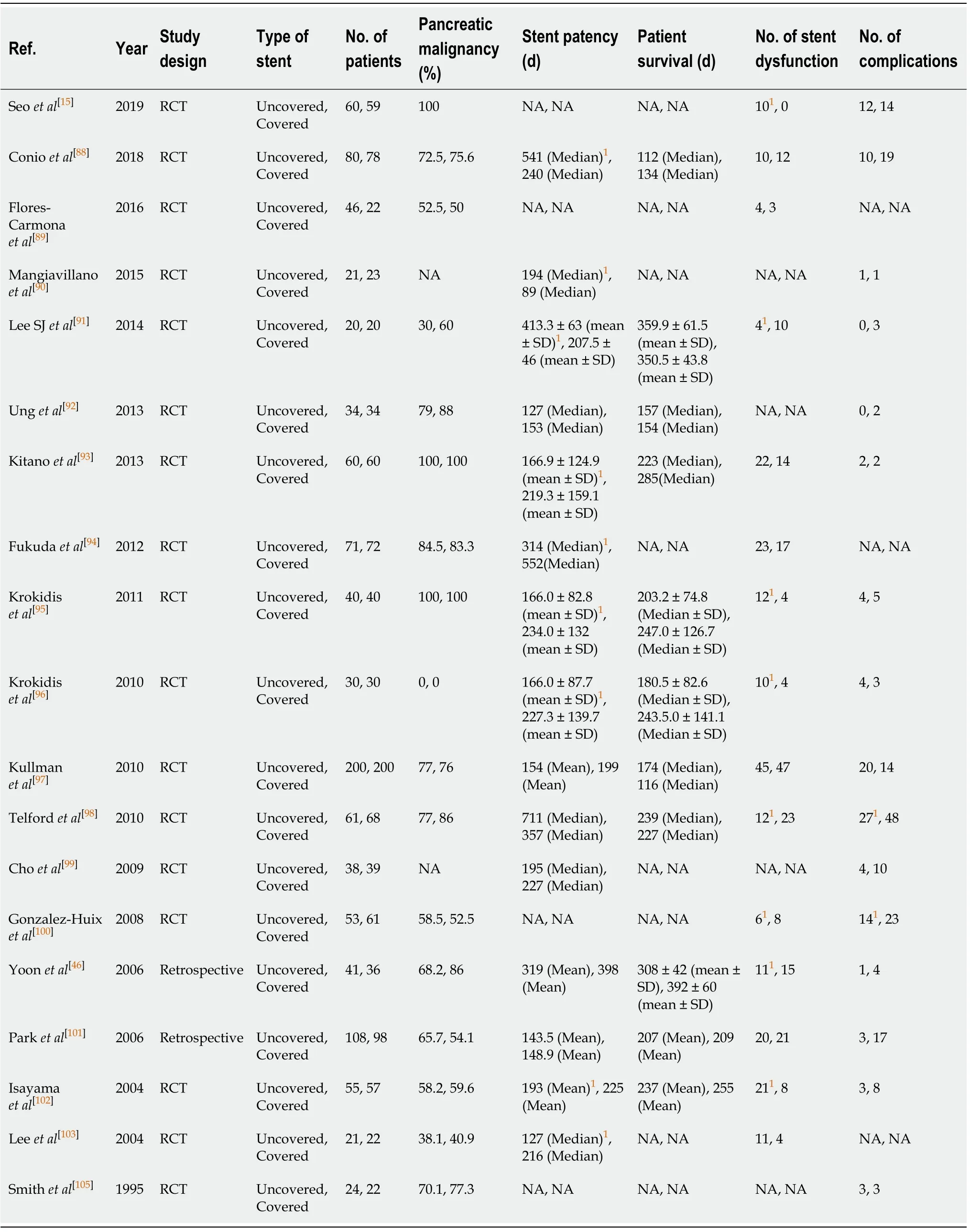
Table 4 Randomized controlled trials and retrospective studies comparing covered with un-covered biliary self-expanding metal stents for malignant distal biliary obstruction
ERCP-PBD using covered SEMS is preferred over uncovered SEMS and plastic stents because of a decreased risk of stent dysfunction and longer stent patency[6].In a recent RCT,Seoet al[106]have shown comparable success rates of covered and uncovered SEMS in pancreatic cancer patients undergoing PBD before and after neoadjuvant therapy,however,covered SEMS were suggested to be superior in cases of diagnosis uncertainty.If a biliary stricture turns out to be malignant,there is no need to replace covered SEMS with uncovered SEMS because risk of stent dysfunction due to tumor ingrowth is negligible.Shorter stent lengths(4 cm as opposed to 6 or 8 cm)and the presence of an in situ gallbladder were significant predictors associated with failure to attain prolonged biliary drainage with a hazard ratio of 2.1 and 6.9[106].The type of stent selection should be individualized based on these factors.Recent meta-analyses and systematic reviews demonstrated an increased risk of complications without a significant survival difference in patients undergoing PBDvsdirect surgery[76,117-119].Severe hyperbilirubinemia was not present in the majority of studies included in meta-analysis,hence the role of PBD in patients with severe biliary obstruction is uncertain.To further investigate the effects of preoperative ERCP on pancreatic cancer survival rates,Rustgiet al[120]assessed overall survival among 2890 patients with pancreatic cancers from 2000 through 2011.Of these,1864 patients underwent ERCP within 6 mo of surgery and 1026 patients underwent surgical resection without preoperative ERCP.After adjustment of confounding factors,patients in the preoperative ERCP group did not demonstrate an increased risk of mortality compared to patients who proceeded directly to surgical resection[121,122].This study did not comment on ERCP-related adverse events such as biliary sepsis,and thus warrants further analysis.In clinical practice,however,preoperative ERCP is often performed due to issues related to either delay in the definitive surgical resection or the provision of neoadjuvant chemotherapy.Overall,PBD should be avoided in patients undergoing early surgical resection(usually under 2 wk),however,those with persistent symptoms(pruritis),severe jaundice,and delay in surgery for medical optimization,PBD may be justified.
ERCP-guided biliary drainage in neoadjuvant treatment of pancreatic cancer
In patients with borderline resectable pancreatic malignancy,neoadjuvant chemotherapy or chemoradiation is clearly beneficial,whereas their role in outright surgically resectable malignancy remains unclear[76].Neoadjuvant therapy enables the surgical resection of a borderline resectable disease by downstaging of pancreatic tumors and has shown to improve the outcomes of surgical management in treating patients with metastasis.Furthermore,PBD is a prerequisite for neoadjuvant therapy to prevent chemotherapy-induced hepatotoxicity and may be pursued 3 mo prior to surgical resection[76].A meta-analysis including six RCT favored the biliary decompression using SEMS in patients with unresectable cancer or those unfit for surgical resection due to multiple comorbidities or advanced disease[75].Among patients with resectable pancreatic cancer who may undergo surgical resection within three months,the placement of a plastic biliary stent should be adequate as prolonged biliary drainage avoids interruptions of medical treatment by improving symptoms of biliary obstruction or cholangitis.Hence the placement of SEMS appears reasonable to consider in these patients.An RCT on SEMSvssurgery to palliate malignant obstructive jaundice in stage IV pancreatic cancer has demonstrated the added benefits of cost-effectiveness,reduced hospital stay,and procedural morbidity in patients palliated with SEMS,a finding that was balanced however by the noted difficulty in SEMS removal during surgery[74].
Role of ERCP in gastric outlet obstruction
Indications:An estimated of 15% of patients with pancreatic cancer experience mechanical gastric outlet obstruction(GOO)during the course of their disease,especially if malignant lesions involve the gastric antrum,proximal or distal duodenum[121,122].Endoscopic-guided enteral stent placement is an effective palliative option in the management of advanced pancreatic cancer[121].Endoscopic palliation of GOO is typically indicated in patients with a shorter life expectancy usually less than 6 mo.
Technical accessibility and consideration:Endoscopic palliation of GOO involves the advancement of a guidewire across the malignant stricture and endoscopic deployment of an enteral stent(covered or uncovered).Simultaneous obstructions of both gastro-duodenal outlet and bile duct are often found in patients with advanced pancreatic cancer.In these cases,the anatomical level of the malignant stricture is classified as obstruction involving proximal duodenum at the level of duodenal bulb or genu(type I),second part of duodenum involving papilla(type II)or distal to papilla in the third part of duodenum(type III)[122].This anatomical classification is important because the level of obstruction determines the management approach.In type I obstruction,an anatomical consideration that enables the advancement of a scope through the duodenal stricture(often with dilatation),biliary stenting should be performed prior to duodenal stent placement.If there are technical difficulties associated with endoscope passage through a duodenal stricture,then duodenal stenting should be performed first,with subsequent advancement of the scope through the duodenal stent to perform either immediate or delayed(after a few days)biliary stenting.In type II obstruction,ERCP-guided transpapillary stenting may be challenging due to difficulty in finding papillary opening.In this situation,EUSguided transmural or antegrade biliary stenting is recommended and duodenal stenting could be performed simultaneously[122].In type III obstruction,the sequence of either biliary or duodenal stent placement is not critical.ERCP-guided transpapillary stenting is associated with poor clinical outcome in patients with combined biliary and GOO because of risk of cholangitis from duodenobiliary reflux of food particles and digestive juice[122].Endoscopic enteral stenting should be performed in cases of a solitary malignant stricture without evidence of distal obstruction from the site of stent deployment.Palliative gastric decompression with the placement of jejunal feeding tube or total parenteral nutrition should be considered in case of multiple strictures or GOO,especially if distal to the location of planned stent deployment[123].In patients who fail standard endoscopic management of GOO,there is increasing use of less invasive EUS-guided gastrojejunostomy due to its advantages to establish longer patency,fewer adverse events,and higher clinical and technical success rates[122,124].
Safety and complications:Overall,the placement of SEMS is associated with more favorable results in patients with poor performance status and a relatively shorter life expectancy,whereas gastrojejunostomy(GJJ)may offer more durable results in patients with a more favorable prognosis[123,125].A systemic review(including 32 studies)and several prospective studies on the endoscopic placement of SEMS studies have shown an overall technical success rate of 97%(91% to 100%)and the clinical success rate of 89%(63% to 95%)[126-134].Another systemic review(44 studies)has shown a higher clinical success rate(89%)of endoscopically placed enteral stents compared to GJJ[125].Placement of enteral SEMS is associated with a shorter hospital stay and early resumption of oral intake,with similar major complication rates noted between SEMS and GJJ[126].Enteral stents are associated with an increased risk of stent migration or malfunction(17%)typically due to tumor ingrowth and/or food impaction,a complication that is managed endoscopically with the clearance of impacted food or stent replacement[123].More recently,a meta-analysis(including 13 studies)on 1624 patients with malignant GOO showed comparable stent dysfunction and similar clinical and technical success rates of coveredvsuncovered SEMS.Covered SEMS,however,showed lower rates of luminal occlusion(RR:0.44;95%CI:0.28-0.68)at the expense of higher stent migration(RR:4.28;95%CI:2.89-6.34)and overall adverse events(RR:1.75;95%CI:1.09-2.83)[135].Covered SEMS are associated with stent migration,usually within 8 wk of placement,requiring endoscopic repositioning or replacement.Other complications of enteral stenting are hemorrhage(1%),enteral perforation(1%),peritonitis,pancreatitis,cholangitis,biliary or intestinal obstruction,and abdominal pain[123].
CONCLUSION
ERCP plays a vital role in the management of pancreatic cancer.ERCP-guided brush cytology and forceps biopsy of malignant biliary strictures provide reasonable tissue for diagnostic confirmation of disease.ERCP-guided SPACE technique is a promising modality that may be superior than EUS-FNA for diagnosing pancreatic case at early stages.The therapeutic interventions of ERCP are helpful in effective preoperative biliary decompression in those with resectable pancreatic cancer.In patients with unresectable pancreatic cancer,palliation with ERCP-guided biliary decompression by the placement of either plastic or self-expanding metal stents relieves symptoms to improve quality of life.Selection of stents should be individualized depending upon patient’s clinical presentation,weighing not only the risks and benefits,but also the physician’s clinical judgement.GOO is a common complication of advanced pancreatic cancer,ERCP-guided enteral stenting is preferred modality over surgical gastrojejunostomy in the management of GOO in patients with poor performance and shorter life expectancy.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Real-world clinical data of endoscopy-based cancer detection during the emergency declaration for COVID-19 in Japan
- Role of endoscopic ultrasound in pediatric patients:A single tertiary center experience and review of the literature
- Endotracheal intubation in patients with COVID-19 using an ultrathin flexible gastrointestinal endoscope
- Fluorescence guided intraluminal endoscopy in the gastrointestinal tract:A systematic review
- Predictor of respiratory disturbances during gastric endoscopic submucosal dissection under deep sedation
- Defining the advantages and exposing the limitations of endoscopic variceal ligation in controlling acute bleeding and achieving complete variceal eradication