Recent advances in third space or intramural endoscopy
2021-01-11AkshayShanbhagPrashanthiThotaMadhusudhanSanaka
Akshay B Shanbhag,Prashanthi N Thota,Madhusudhan R Sanaka
Akshay B Shanbhag,Prashanthi N Thota,Madhusudhan R Sanaka,Department of Gastroenterology,Cleveland Clinic Foundation,Cleveland,OH 44195,United States
Abstract Third space endoscopy or intramural endoscopy is based on the principle that the deeper layers of the gastrointestinal tract can be accessed by tunneling in the submucosal space and maintaining the integrity of the overlying mucosa.The era of third space endoscopy started with peroral endoscopic myotomy (POEM) for treatment of achalasia and has expanded to treat various other gastrointestinal disorders.The technique is also currently used for treatment of refractory gastroparesis,Zenker’s diverticulum (ZD),resection of subepithelial tumors and early cancers of the gastrointestinal tract and Hirschsprung’s disease (HD).These procedures are rapidly emerging as minimally invasive alternatives to conventional surgery.They are safe and effective with excellent outcomes.This review focuses on the evolution and current applications of third space endoscopy in various gastrointestinal disorders.Key points:(1) Third space or intramural endoscopy initially started with the POEM procedure for treatment of achalasia;(2) Advancements in procedural techniques have expanded its application to treat other gastrointestinal disorders such as refractory gastroparesis,ZD,HD,resection of subepithelial tumors and early gastrointestinal cancers;(3) These procedures are highly effective with excellent outcomes and low complication rates;and (4) Third space endoscopic procedures are rapidly emerging as minimally invasive alternatives to conventional surgery.
Key Words:Third space endoscopy;Peroral endoscopy myotomy;Endoscopic submucosal dissection;Per-oral pyloromyotomy;Per-rectal endoscopic myotomy
INTRODUCTION
Conventional endoscopic procedures are performed within the natural lumen of the gastrointestinal tract which is considered as first space endoscopy.In the last two decades,endoscopic pioneers tried to venture into peritoneal cavity or second space through natural orifice transluminal endoscopic surgery (NOTES),in which the peritoneal cavity (second space) was accessed endoscopically through one of the natural orifices.In 2004,Kallooet al[1]described a transgastric peritoneoscopy for a liver biopsy in an animal model,a procedure which involved breaching the gastric wall for peritoneal access.Subsequently,few case reports of appendectomy and cholecystectomyviaNOTES in humans were reported[2,3].NOTES had many potential benefits such as absence of scarring,reduced length of hospitalization,along with minimal or no pain.However,there were several challenges as well.Lack of optimal instruments for dissection and retraction and difficulty with securely closing and suturing of the entry points increased the risk of pneumoperitoneum and lead to severe infectious complications such as peritonitis and sepsis[4].Hence,NOTES never took off in clinical practice and eventually faded away.In 2007,Sumiyamaet al[5]described a novel technique of submucosal endoscopy or intramural endoscopy with a mucosal flap safety valve.Using the principles of endoscopic submucosal dissection(ESD),the submucosal space or “third space” was accessed and used as a working plane while the mucosal flap prevented any peritoneal leakage[5].Pasrichaet al[6]adopted this principle and described the feasibility of esophageal myotomy in a porcine model.The technique was then refined and perfected by Inoueet al[7],who performed the first human case of endoscopic myotomy for achalasia in 2008,what is now known as the peroral endoscopic myotomy (POEM).This started the era of third space endoscopy,which disseminated rapidly all over the world.The technique evolved and is currently used to not only to treat achalasia but also other gastrointestinal disorders such as Zenker’s diverticulum (ZD),gastroparesis,resection of submucosal tumors and early gastrointestinal cancers (Table 1).
POEM
Achalasia is a rare,idiopathic esophageal motility disorder characterized by esophageal aperstalsis and impaired relaxation of lower esophageal sphincter (LES).Classic symptoms include dysphagia,regurgitation,chest discomfort and weight loss.There is no cure and all treatments are aimed at relieving the functional obstruction at the esophagus by targeting the distal esophagus,LES and proximal stomach.Standard treatments include pneumatic dilation,Heller myotomy (HM) and botulinum toxin injection into the LES.In the past decade,POEM has rapidly emerged as one of the preferable treatment options for achalasia.POEM has the advantages of minimal invasiveness of an endoscopic procedure along with the precision and efficacy of a surgical myotomy.The steps involved in POEM as illustrated in Figure 1 are:Submucosal injection in the mid esophagus to create a submucosal bleb,a mucosal incision to enter the submucosal space (Figure 1A) and to create a submucosal tunnel along the esophageal length (Figure 1B),then an esophagogastric myotomy (Figure 1C and D),followed by closure of submucosal entry point with endoscopic clips(Figure 1E)[8].POEM is performed under general anesthesia and patients are typically discharged home the next day after an overnight fasting and observation.Patients are initially started on clear liquid diet which is gradually advanced to a regular diet over the next few weeks.
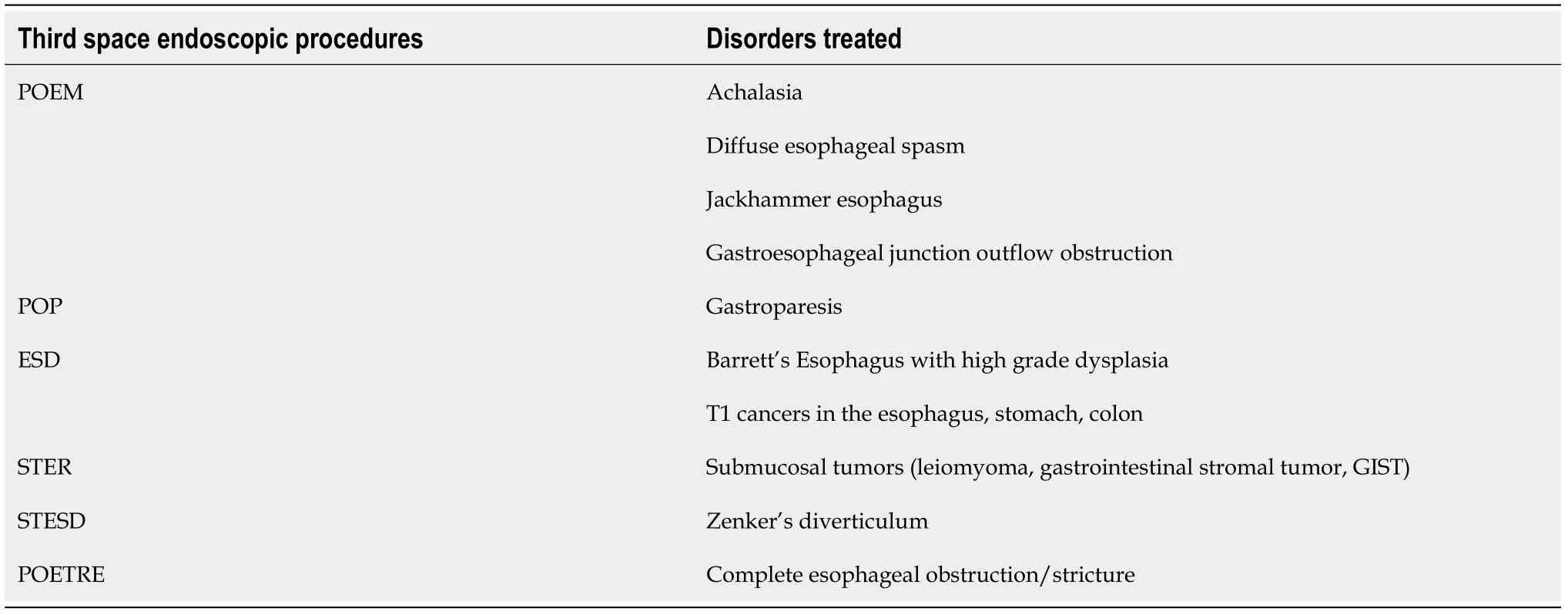
Table 1 Disorders treated with third space endoscopic procedures
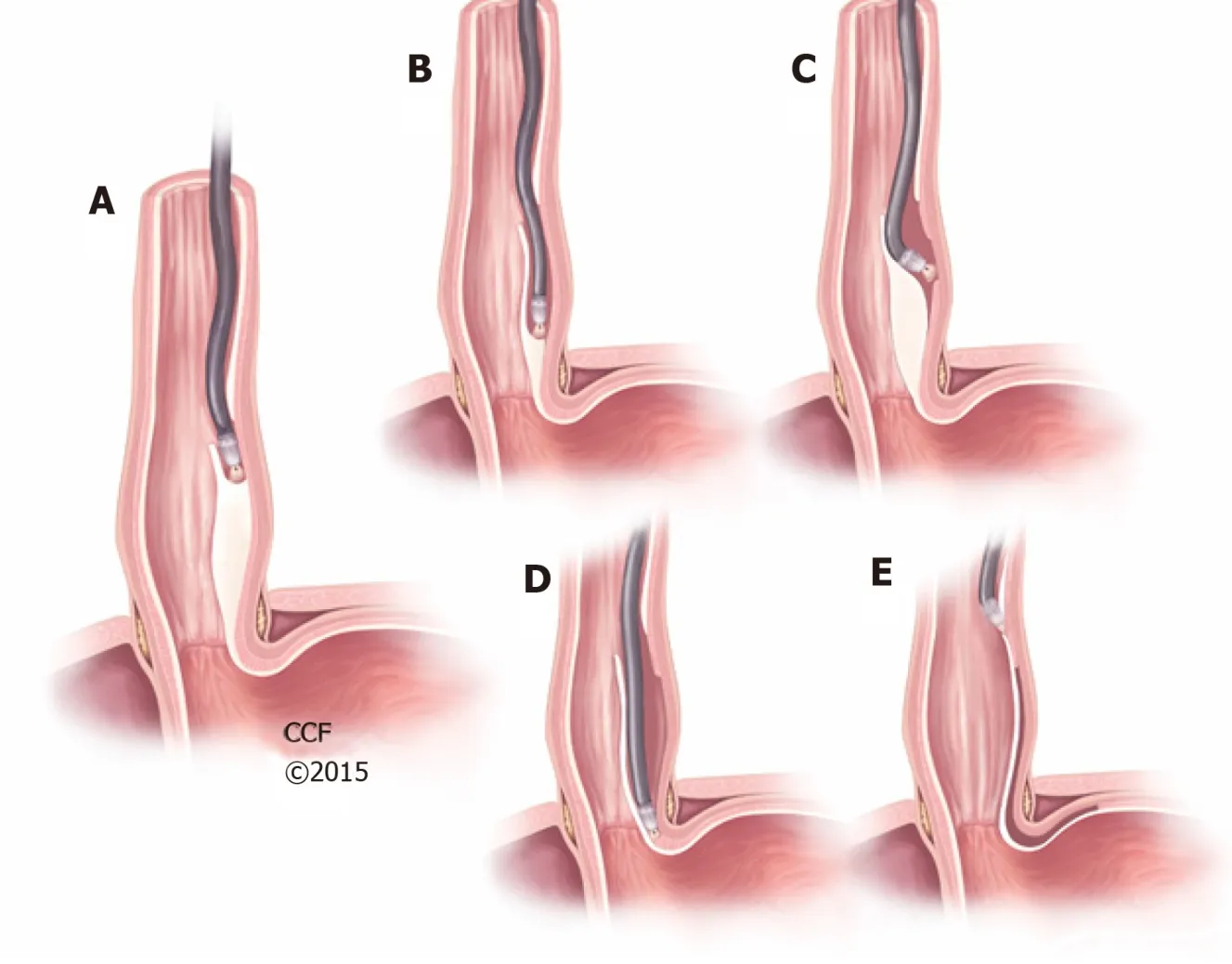
Figure 1 Peroral endoscopic myotomy.
Eckardt score is a clinical symptom score commonly used in achalasia ranging from 0-12 based on severity of symptoms (0 = least and 12 = most severe symptoms).Clinical success after POEM is usually defined as reduction of Eckardt score to ≤ 3.A systematic review by Akintoyeet al[9]involving 36 studies and 2373 patients who underwent POEM for achalasia showed a clinical success of 98% with a preoperative Eckardt score of 6.9 ± 0.15 reducing to 0.77 ± 1.0 post-procedure which continued to remain low (1.0 ± 0.08) at 12 mo follow-up.Reduction in LES pressures correlated with clinical efficacy and POEM led to significant reduction in LES pressures in that systematic review[9].
In a subset of patients with treatment failure to HM and pneumatic dilation,POEM was found to be successful[10].Achalasia is classified into 3 subtypes based on findings on high-resolution esophageal manometry.POEM was found to have good clinical success in all three subtypes of achalasia[11].A large study conducted by Nabiet al[10]looking at treatment naivevsprior treatment failures in 502 patients determined comparable clinical success in both groups.Nabiet al[12]performed a study involving pediatric patients with all three subtypes of achalasia which showed a clinical success of 83.3% at 4-year follow-up.POEM was also found to be as effective in elderly patients.There were no significant differences in clinical success,intraoperative complications or rates of gastroesophageal reflux disease (GERD) in patients >60 years when compared to younger patients[13].
Compared to other treatment modalities,POEM demonstrated greater efficacy.Clinical success of POEMvspneumatic balloon dilation at 36 mo was found to be 93%vs60%,respectively[14].This was further confirmed in a randomized control trial (RCT)comparing POEM to pneumatic dilation where,among treatment naive patients,POEM was found have greater clinical success at 2 years[15].In a RCT with 221 patients,POEM was also found to be non-inferior to laparoscopic Heller myotomy (LHM) in controlling achalasia symptoms at 2 years[16].However,when compared to LHM in a meta-analysis,the success rate in type I,II and III achalasia was found to be 81%,92%and 71% for LHM and 95%,97% and 93% for POEM,respectively[17].Based on current evidence,POEM has the potential to be the treatment of choice for all subtypes of achalasia in treatment naïve or prior treatment failure patients across all age groups.
There are only few studies about the learning curve for POEM procedure.Two studies that aimed to define the learning curve assessed the learning curve somewhat differently.The first study looked at procedural efficiency and mastery.Efficiency was defined as the point in the learning curve where the operator started engaging in performance refinements that lead to a decrease in procedure time and mastery was defined as the point at which the procedure time became consistent and no further change in mean procedure time was noted[18].This study showed that efficiency and mastery were attained after 40 and 60 procedures,respectively[18].The second study,however,looked at the “learning rate”,defined as the number of procedures required to reach 90% potential (speed at which the subject acclimated to the procedure) and found that the procedure time decreased as experience increased with a learning rate of 13 cases[19].However,both of these studies failed to show a statistical correlation between experience and improvements in postop Eckhart score or rate of accidental mucosotomies[18,19].Another prospective study involving 40 patients undergoing POEM showed that mastery of POEM,which was evidenced by a decrease in the length of procedure per centimeter of myotomy and inadvertent mucosotomies,was achieved after about 20 cases[20].A large retrospective analysis of POEM procedures involving 1346 patients with the primary outcome being a composite of technical failure and adverse events and secondary outcome being procedure time found that 100 cases were required to decrease the risk of technical failure and adverse events and 70 cases were needed to reduce the procedure time[21].This indicated that the outcomes after POEM were dependent on the operator skill[21].
ADVERSE EVENTS OF POEM
Since POEM is not combined with an anti-reflux procedure such as fundoplication,there is a higher probability of post-operative GERD,which is observed in a high percentage of post-POEM patients.A retrospective analysis of 849 patients showed clinical reflux was seen in 23.9% of post-POEM patients[22].Abnormal esophageal acid exposure was also found to be significantly higher in POEMvsLHM (39%vs17%) in a systematic review with meta-analysis[23].
The incidence of major adverse events is relatively uncommon after POEM and most of them can be managed non-operatively.First,complications related to insufflation such as capnoperitoneum and capnothorax can occur.However,the majority of the insufflation related events do not require any intervention and resolve spontaneously.A large multi-center study involving 1826 POEM patients showed an overall incidence of adverse events to be 7.5%,with only 0.5% being severe adverse events[24].The rate of bleeding (intraoperative and delayed) and mucosal perforations were found to be 0.9% and 2.8%,respectively[24].Technical failure (aborted POEM procedures),although rare,was reported to be less than 1%[25].Submucosal fibrosis was identified as the most common cause of technical failure[25].Other factors predictive of failure included multiple prior treatments,sigmoid esophagus and disease duration >10 years[22].
SUBMUCOSAL TUNNELING ENDOSCOPIC RESECTION
Subepithelial or submucosal tumors (SMT) in the GI tract are considered to be primarily benign,however,some SMT,such as gastrointestinal stromal tumors and carcinoids can have a malignant potential.Conventionally,these were treated by surgery.ESD has been used for treating SMT in the past,however,this can be challenging if the tumor arises from or infiltrates the muscularis propria (MP) layer.Submucosal tunneling endoscopic resection (STER) is a relatively new technique that emerged from the concept of POEM and has shown promise with a low risk of perforation and complications.The steps of STER are as follows:Injection of saline with a coloring agent to create a submucosal bleb followed by a mucosal incision approximately 3-5 cm proximal to the SMT,submucosal dissection and creation of a submucosal tunnel,dissection of the tumor from the MP layer,tumor excision,and closure of the mucosal flap/entry site with endoscopic clips[26].
First described by Inoueet al[27]in 2012,the STER technique has gained traction in treating submucosal tumors with no recurrence at follow-up[26].A large study that evaluated 165 patients with SMT undergoing STER showed anen blocresection rate to be 78.7% with a complication rate of 21.2%[26].However,a meta-analyses evaluating GI SMTs in the upper,middle,lower esophagus and the cardia found theen blocresection rate to be >94%[28].However,en blocresection rates were better for smaller tumors,typically less than 2 cm.Larger size usually resulted in piecemeal resection while lowering theen blocresection rate[29].Therefore,prior imaging with computed tomography (CT) or endoscopic ultrasoun to assess the lesion size is typically recommended.Typically,surgery is considered first line;however,when compared to thoracoscopic enucleation,STER demonstrated comparable complete anden blocresection rates.STER was,however,superior to thoracoscopic enucleation with shorter operative time and lower costs[29].Common adverse events included capnomediastinum and subcutaneous emphysema,which were managed nonoperatively[26].When compared to other resection procedures such as ESD,no difference was seen in the rates of complications between the two procedures[30].A retrospective study evaluated 137 patients with esophageal SMTs originating from the MP layer.The patients were divided in 3 groups:STER,ESD and thoracoscopic enucleation.The STER group had the shortest hospitalization and lowest cost,compared to ESD and thoracoscopic enucleation.However,when compared to ESD,STER had longer operation times and loweren blocresection rates.All patients were found to be free from local recurrence and metastasis after a 22-mo follow up[30].
Therefore,STER appears to be a safe and an effective treatment modality for SMT,preferably <2 cm,involving the MP layer.However,SMT extending into the serosa,would require a multi-disciplinary approach involving both the endoscopist and the surgeon to select an appropriate therapeutic approach.
PER-ORAL PYLOROMYOTOMY
Gastroparesis,defined as delayed gastric emptying in the absence of mechanical obstruction,is a chronic progressive disorder.Common causes include diabetes,idiopathic and post-surgical.Traditional treatment modalities include dietary modifications and prokinetic agents.Endoscopic botulinum injection into the pylorus has been used but it was not found to be superior to placebo[31].Laparoscopic pyloroplasty was shown to be effective in gastroparesis[32];however,a novel technique,per-oral pyloromyotomy (POP),also known as gastric per-oral endoscopic pyloromyotomy (G-POEM),is currently showing promising results for refractory gastroparesis.
Khashabet al[33]described the first human case of POP for refractory diabetic gastroparesis in 2013.The first prospective study by Rodriguezet al[34]evaluated the safety and efficacy of POP in one hundred consecutive cases.There was a significant improvement in both subjective and objective measures of gastroparesis including gastroparesis cardinal symptom index (GCSI) and gastric emptying time measured though a 4 h solid phase gastric emptying study (GES).In that study,78% of patients that completed a repeat GES at 3 mo had a significant improvement in gastric emptying times,while the study completely normalized in 57% of patients[34].Longer disease duration was associated with lower GCSI scores[35].Another study compared results in patients undergoing laparoscopic pyloroplastyvsPOP[36].Both groups experienced significant improvement in gastric emptying times at 3 mo.The endoscopic group,however,was found to have shorter procedure times,less blood loss,shorter length of stay,and a lower tendency of 30 d complications[36].
The steps of POP as illustrated in Figure 2 are:Submucosal injection with a coloring agent proximal to the pylorus to create a submucosal bleb (Figure 2A) followed by mucosotomy (Figure 2B),dissection of the submucosa until the pylorus is identified(Figure 2C),pyloromyotomy performed in a distal to proximal fashion (Figure 2D)followed by closure of the mucosotomy by endoscopic clips (Figure 2E)[37].Two approaches for POP were described.One where the procedure is performed along the lesser curvature and the other where it is performed along the greater curvature.The lesser curvature approach is preferred as it has a shorter operative time,and high success rate when compared to the greater curvature approach[37].Adverse events of POP include capnoperitoneum,bleeding and ulceration at the POP site[33].Most of these can be managed non-operatively.
SUBMUCOSAL TUNNELING ENDOSCOPIC SEPTUM DIVISION
ZD is a pulsion diverticulum that occurs due to outpouching of the esophageal mucosa through the Killian’s triangle due to a hypertensive cricopharyngeus.Traditionally treated with surgery,flexible endoscopic approaches are emerging as minimally invasive alternatives with lower morbidity.A meta-analysis of twenty studies found that the pooled success rates,adverse events and recurrence rates of flexible endoscopic septum division was 91%,11.3% and 11%,respectively[38].However,significant rates of adverse events and recurrences prompted the search for safer alternative treatment options.Submucosal tunneling endoscopic septum division(STESD),or Z-POEM,is a novel approach employing third space endoscopy technique.First described by Liet al[39]in 2016 for treating ZD,it has resulted in improvement in dysphagia without any procedure-related adverse events.STESD involves a mucosal incision proximal to the septum followed by creation of a submucosal tunnel (Figure 3A and B).The cricopharyngeal muscle fibers are then dissected to the bottom of the diverticulum which is then followed by closure of the entry site with endoscopic clips (Figure 3C-E)[39].Ability to perform complete dissection of the muscle,while minimizing the risk for perforation and mediastinitis,are potential advantages of STESD over conventional flexible endoscopic approach.Data on the efficacy and safety of STESD are emerging.
ESD
ESD technique was first described in 1988 as a non-operative modality to resect gastric neoplasia in Japan[40].Technological advancements have expanded its applications to other conditions across the GI tract,including early neoplastic lesions in the esophagus and colon.ESD is typically employed foren blocresections of early gastrointestinal neoplastic lesions confined to mucosal layer.The conventional method of ESD is typically used.However,en blocresection proves to be difficult in the presence of submucosal fibrosis which can lead to poor lifting after submucosal injection,causing technical difficulties.Furthermore,submucosal lifting is also compromised by fluid dispersion after a circumferential mucosal incision[41].Third space endoscopy techniques can be employed as modifications to traditional ESD technique to address this issue such as the pocket creation method (PCM) and the tunneling technique.These two techniques fall under the realm of third space or intramural endoscopy as submucosal dissection is used to create a tunnel or a pocket underneath the lesion,which are used as a working plane.Tunneling ESD is typically employed for resection of very large lesions and circumferential lesions,which are technically very challenging by conventional ESD technique.Typically,the steps of conventional ESD as illustrated in Figure 4 are as follows:Marking the perimeter of the lesion with cautery (Figure 4A),administering a submucosal injection to create a bleb (Figure 4B),creating a circumferential mucosal incision followed by submucosal dissection under the lesion until the lesion is completely resected (Figure 4C and D)[42].
The PCM technique is performed in the same way,however,instead of performing a circumferential mucosal incision around the lesion,the incision in PCM is very minimal.The minimal incision prevents the fluid dispersion and improves submucosal lifting which allows the endoscopists to create a submucosal pocket below the lesion which is followed by resection.Compared to conventional ESD,PCM was shown to have betteren blocresection rates in lesions with and without fibrosis and lower perforation rates[41].Therefore,ESD with PCM technique allows for a more reliable and safe resection.
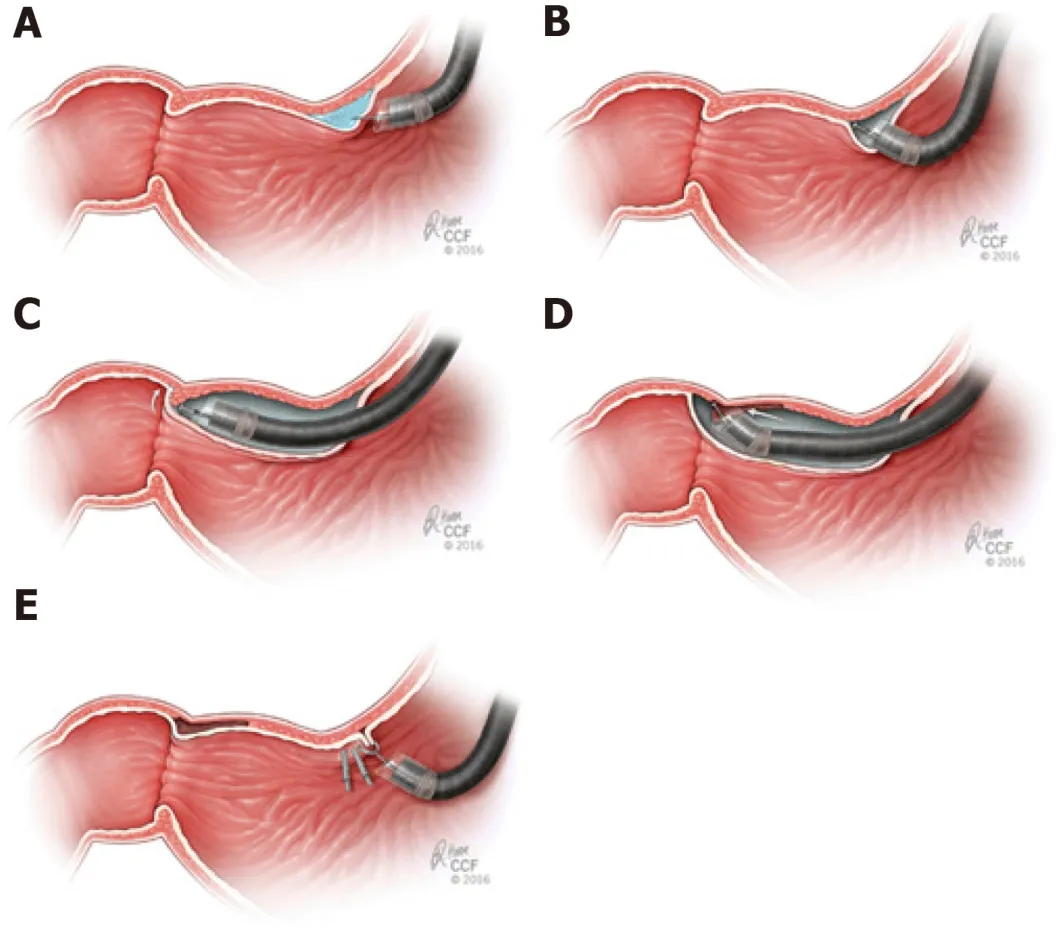
Figure 2 Per-oral Pyloromyotomy.
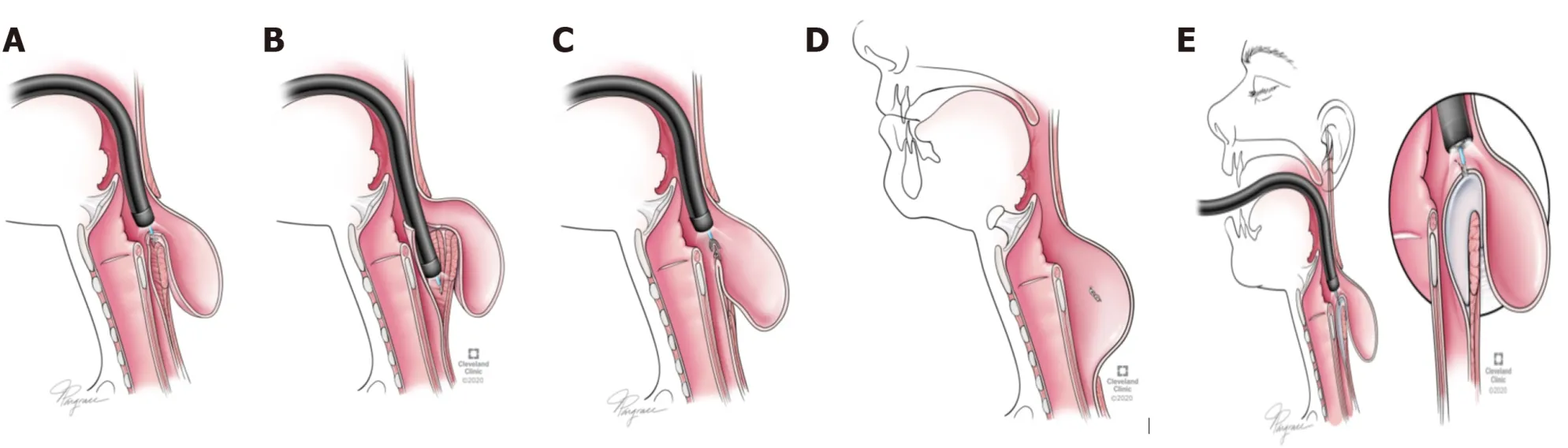
Figure 3 Submucosal tunneling endoscopic septum division.
RECENT ADVANCES IN THIRD SPACE ENDOSCOPY
Recently,third space endoscopy principles were applied in restoration of lumen in complete esophageal obstruction (CEO) and in the treatment of Hirschsprung’s disease (HD).
PER-RECTAL ENDOSCOPIC MYOTOMY
HD is a motor disorder that results from aganglionosis of the myenteric plexus,starting at the rectum and extending proximally.It normally presents with constipation and/or intestinal obstruction.Principles of third space endoscopy have been implemented in treating this disorder as well.Bapayeet al[43]performed the first per rectal endoscopic myotomy for short segment HD in a 24-year old male patient with no adverse effects and significant relief in symptoms at 24-wk follow-up.The same technique has been utilized in pediatric patients with HD with refractory constipation with symptom relief and absence of incontinence on follow-up[44].
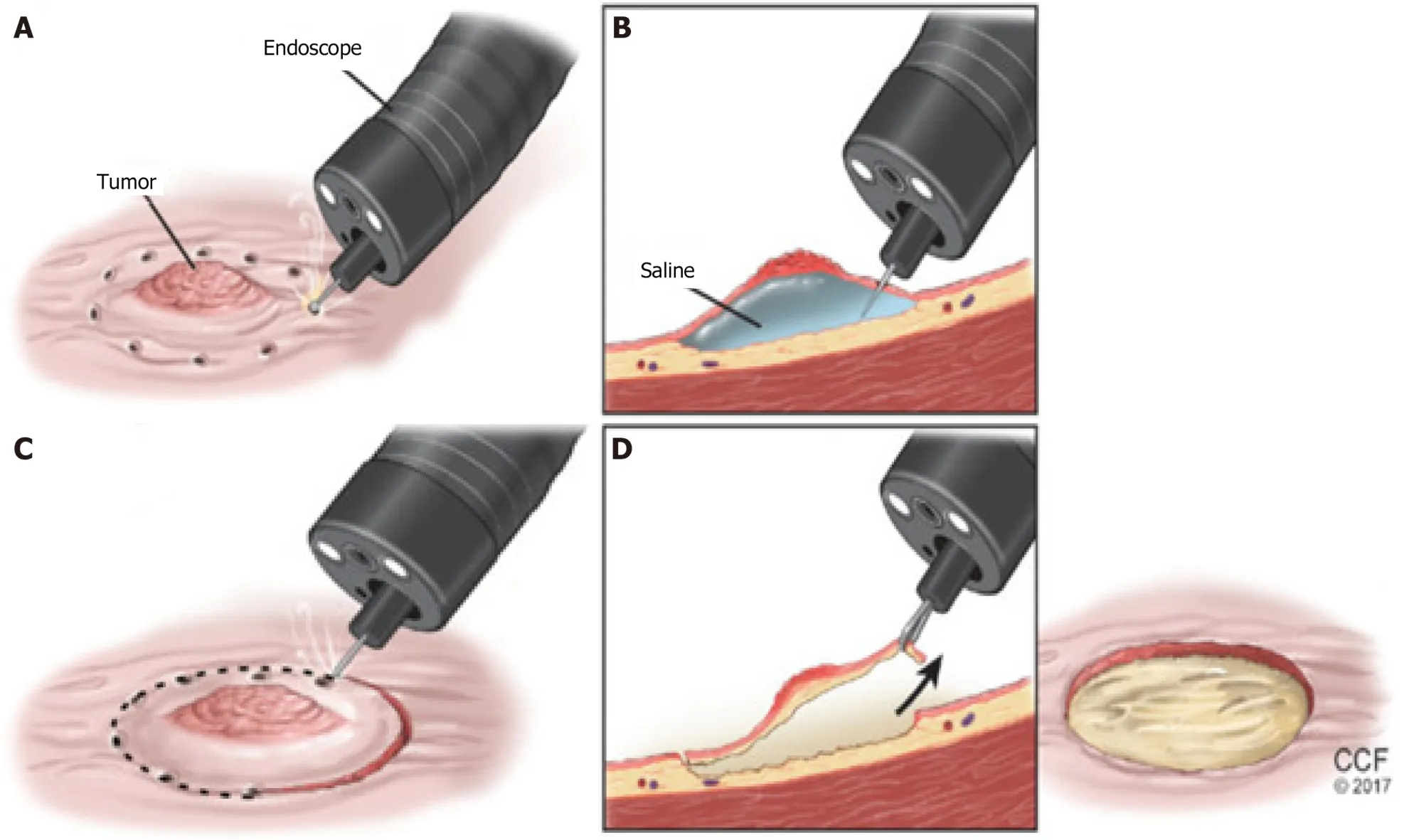
Figure 4 Endoscopic submucosal dissection.
PERORAL ENDOSCOPIC TUNNELING FOR RESTORATION OF THE ESOPHAGUS
Total aphagia from CEO is a rare adverse event in some patients after undergoing chemoradiation for esophageal malignancies.Waghet al[45]described a relatively new technique using the principles of third space endoscopy called peroral endoscopic tunneling for restoration of the esophagus in which a submucosal tunnel is created which traverses the stricture followed by placement of an esophageal stent to maintain lumen patency.This procedure was shown to be successful in all 4 patients in a case series,with a reduction in the dysphagia scores during a mean follow-up of over 6 mo.However,all patients did require serial endoscopic dilations post-procedure[45].
There have been other novel applications of third space endoscopy.Electrical stimulation of LES is a promising treatment for GERD with significant improvement in heartburn and regurgitation[46].Third space endoscopy has been used for implantation of stimulation leads in human subjects with positive results[47].Third space endoscopy has the potential to offer safer means for NOTES and peritoneoscopy.With further refinement and improvement in technology,it has potential to be an alternative to diagnostic laparoscopy for staging of malignancies.
CONCLUSION
Management of GI disorders continues to evolve with third space endoscopy.Initially used for achalasia,the application of third space endoscopy has expanded to other conditions such as refractory gastroparesis,ZD and resection of early gastrointestinal cancers and subepithelial tumors.Compared to the conventional treatment modalities,third space endoscopic procedures have been proven to be highly effective with an excellent safety profile.Although long term and prospective comparative studies are needed,third space endoscopy has a great potential and holds tremendous promise in the near future.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Assessment of disease activity in inflammatory bowel diseases:Non-invasive biomarkers and endoscopic scores
- Efficacy and safety of peroral endoscopic myotomy after prior sleeve gastrectomy and gastric bypass surgery
- Crohn’s strictures open with anti-mycobacterial antibiotic therapy:A retrospective review
- Common bile duct lesions-how cholangioscopy helps rule out intraductal papillary neoplasms of the bile duct:A case report
