Exploring the safety and efficacy of adding ketoconazole to tacrolimus in pediatric renal transplant immunosuppression
2020-12-25SindyndezBrookeRamayAngieAguilarGonzlezRandallLouMeda
Sindy Méndez, Brooke M Ramay,Angie Aguilar-González, Randall Lou-Meda,
Sindy Méndez, Angie Aguilar-González, Randall Lou-Meda, Fundación para el Niño Enfermo Renal - FUNDANIER, Hospital Roosevelt Guatemala, Guatemala 01010, Guatemala
Brooke M Ramay, Department of Pharmaceutical Chemistry, Universidad del Valle de Guatemala, Guatemala 01015, Guatemala
Abstract
Key Words: Transplant; Immunosuppression; Tacrolimus; Ketoconazole; Pediatric; Chart review
INTRODUCTION
Treating pediatric patients with End-Stage Renal Disease (ESRD) in low to middle income countries is challenging[1-3]. Unfavorable socioeconomic conditions, insufficient numbers of pediatric clinics treating ESRD, limited access to medication, and clinics working with limited resources to treat patients with renal replacement therapy (RRT), all pose serious challenges for clinicians and patients with ESRD[1,4,5]. In addition to clinical challenges, government expenditures on health in Low to Middle Income Countries (LMIC) have been shown to range from 2.6% to 9% of the national Gross Domestic Product (GDP), a small fraction of each nation's income[1]. These clinical barriers to care, combined with paucity in national investment in RRT, result in a significant number of patients left without healthcare services treating RRT. Worldwide data show that over 2 million people are kept alive by RRT, the majority of whom are treated in only five countries (United States, Japan, Germany, Brazil, and Italy) constituting only 12% of the world´s population[6]. In contrast, only 20% are treated in about 100 LMIC that make up over 50% of the world's population[6]. For every 1 million population with ESRD, less than 100 are treated in LMIC countries. In contrast, more than 1000 per million population are treated in high income countries; the prevalence of RRT is higher in countries with higher incomes[7]. This depicts a clear and direct association between GDP and availability of RRT.
The population of Guatemala exceeds 16 million inhabitants, 61% of which are under the age of twenty one[8]. ESRD incidence in children in Guatemala is 4.6 per million age-related population (pmarp)[9,10]. As in other LMIC, clinics struggle to obtain the necessary resources to provide RRT for pediatric patients. The Foundation for Children with Kidney Diseases (FUNDANIER) was founded in 2007 in agreement with the Ministry of Health through Roosevelt Hospital, and created the first program providing free access to comprehensive RRT including transplantation, and immunosuppressive treatment, to Guatemalan children[9,10]. In our program we previously reported a patient population of 432 patients with chronic kidney disease (CKD) stage 2 or more. Of these, 193 were stage 5 CKD of whom 40% received peritoneal dialysis, 26.4% received hemodialysis, 12.4% received a transplant, and 17.6 % were managed without RRT[9].
Transplant clinics in developing countries other than Guatemala have similar goals and objectives in expanding successful renal transplant care at the lowest possible cost, and have reported the combined use of ketoconazole with low-dose tacrolimus to increase tacrolimus bioavailability through metabolic inhibitionviaP450 3A4[11-17]. Small short-term studies had previously supported such practice in Egypt, México, United States and India resulting in an annual cost savings of up to 60% in the immunosuppressive protocol while maintaining safety and efficacy of therapy in adults[11-14]. This combination has yet to be used in Central America where outcomes using the combination, especially in children, are still unknown[11,12].
The objective of this study was to identify the changes in tacrolimus dose and plasma concentration associated with the use of ketoconazole as a pharmacokinetic booster. We explore the safety, efficacy and the associated cost reduction of this combination in a retrospective cohort of children with kidney transplant in the FUNDANIER.
MATERIALS AND METHODS
After approval by the Research Ethics Committee at the Universidad del Valle de Guatemala (QF-010-febrero2015), we performed a retrospective evaluation of all pediatric renal recipients who received concomitant ketoconazole in tacrolimus-based immunosuppression in the FUNDANIER, a tertiary care renal transplant center in Guatemala. FUNDANIER carries out approximately 8-10 pediatric renal transplants per year in a population where patients are at, or below the national poverty line. Maintenance immunosuppressive treatment costs USD 725 per month for an average patient weighing 20 kg (this cost represents the average of protocol A and protocol B for a 20 kg-patient)[18-21].
At FUNDANIER, patients do not have to pay for transplant services and medications, as they are provided by the clinic. In order to achieve optimal cost benefit outcomes while maximizing patient coverage, immunosuppressive protocols are designed to treat patients at the lowest possible price[22-27]. For example, initial posttransplant protocol calls for use of tacrolimus, mycophenolate and prednisone (protocol A) after completing one year on maintenance therapy at FUNDANIER, mycophenolate is replaced by azathioprine, a more affordable immunosuppressive medication (protocol B). With this intervention, FUNDANIER has improved the access to maintenance immunosuppressive therapy, reducing the cost by 40%. For example, replacing protocol A with protocol B in a patient who weighs 20 kg results in a cost reduction from USD 904 per month to USD 544 per month[18-21]. These types of changes to immunosuppressive regimens have been used at FUNDANIER to successfully overcome budget constraints and more effectively provide medication to patients.
We carried out a retrospective observational study, with a pre-post single arm design[22]collecting information from 2011 to 2015 from a cohort of patient records stored in the FUNDANIER database before and after the addition of ketoconazole to the usual immunosuppressive protocol. Inclusion criteria for chart review were: Age younger than 18 years old, at least 3 mo in the program post-transplantation currently on the tacrolimus protocol, and switched to ketoconazole/tacrolimus combination during their outpatient transplant clinic attendance. Charts were reviewed to identify the point at which ketoconazole was added to the post-transplant treatment. A total of six documented visits were reviewed for each patient chart during the study: 3 visits prior to ketoconazole initiation and 3 visits after the combination was initiated. An average of 2 mo between each visit was documented.
Based on the pediatric nephrology service protocol, all patients in the chart review initially received the following maintenance immunosuppressive treatment (“protocol A”): Tacrolimus (0.1-0.3 mg/kg/d), mycophenolate (1200 mg/m2/d) and prednisone (5 mg/d). Ketoconazole suspension (100 mg/5 mL) at a dose of 1.5 mg/kg/d in one dose per 24 h was added to the immunosuppressive treatment (Ketospor Qualipharm®) during the period of 2011-2015. Patients were instructed not to take macrolides or grapefruit at the time of the study.
Outcome measures obtained from patient charts were: (1) Tacrolimus dose/kg; (2) Serum tacrolimus levels (taken at hospital laboratory by the electrochemiluminescence (ECL) method and documented in charts); (3) Estimated glomerular filtration rate (eGFR) was estimated by the Schwartz formula[22]through creatinine measured by the Jaffe method; (4) Graft rejection, defined by the transplant team at the hospital as biopsy findings or a 50% elevation in serum creatinine without apparent cause, and with a favorable response to treatment with steroids; (5) Ketoconazole hepatotoxicity was defined as an increase in liver enzymes greater than twice the normal value compared to the reference laboratory (transaminases); and (6) Cost difference of immunosuppressive treatment.
Data analysis
Descriptive statistics were used to define the tacrolimus dose and serum concentration for each patient and for the entire population before, and after initiating therapy with ketoconazole. eGFR values were calculated during follow-up for graft stability and function. The number of graft rejection episodes before and after ketoconazole were reported, additionally, the number of cases where transaminases were two times the normal limit compared to laboratory reference values during ketoconazole combination were monitored and used as an indication of toxicity. The cost of immunosuppressive treatment is reported prior to and after ketoconazole use.
Mean differences in the dose of tacrolimus and eGFR before and after addition of ketoconazole were compared using the paired student’st-test. Statistical significance was defined using a 95% confidence interval andPvalues less than 0.05.
RESULTS
According to the FUNDANIER database in 2015, twenty-five post-transplant patients used ketoconazole combined with tacrolimus. Twelve (48%) patients were male and the average age of the patients was 13 years. Ninety six percent of transplants were from living donors with a mean follow-up of 18.5 mo (± 20).
Tacrolimus dose and serum concentrations
The average recorded tacrolimus weight-based doses at six, four and two months prior to ketoconazole initiation were 0.13 mg/kg/d; 0.12 mg/kg/d; and 0.11 mg/kg/d, respectively. The average recorded tacrolimus weight-based doses at two, four and six months post-ketoconazole initiation were 0.09 mg/kg/d; 0.07 mg/kg/d; and 0.06 mg/kg/d, respectively.
The mean tacrolimus blood levels at six, four and two months prior to ketoconazole initiation were: 7.4 ± 2.6 ng/dL; 7.4 ± 2.5 ng/dL; and 7.4 ± 2.6 ng/dL, respectively. The mean tacrolimus blood levels recorded at two, four and six month visits postketoconazole initiation were: 8.8 ± 4.9 ng/dL; 6.9 ± 3.6 ng/dL; and 6.8 ± 3.2 ng/dL, respectively (Table 1).
There was a non-significant difference between the mean tacrolimus doses at six months and two months prior to ketoconazole: -0.10 ± 0.04 (95%CI: 0.007, -0.029),P= 0.23. However, the difference between the mean tacrolimus doses six months prior to ketoconazole initiation and six months after ketoconazole addition was significant: 0.06 ± 0.05 (95%CI: -0.034, -0.086)P< 0.001.
There were no observed fluctuations in the blood levels of tacrolimus among patients during the visits before the combination, as compared to after the combination with ketoconazole (Table 1). None of the patient charts documented a variation in serum transaminase levels during the visits pertaining to use of the ketoconazoletacrolimus combination. Overall, a reduction in tacrolimus dose was observed. The mean tacrolimus dose reduction was 45% (± 25%) after the addition of ketoconazole.
Renal function
The mean eGFR before the addition of ketoconazole was 69.2 (± 29.7) mL/min/1.73 m2and after the initiation of ketoconazole was 66.4 (± 23) mL/min/1.73 m2. Changes in eGFR were not significant (P= 0.062) (Table 1). However, patients demonstrated an increased eGFR level from 2 mo prior to the combination and 6 mo post-combination during the study period (P <0.050).
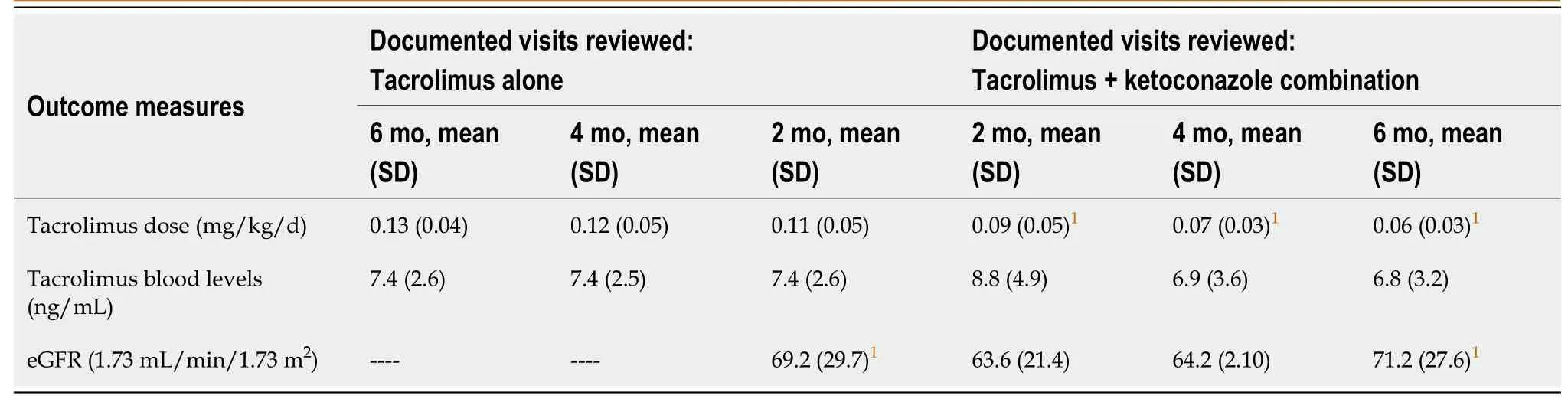
Table 1 Outcome measures
Graft rejections
10 rejection episodes were reported during the study, the majority of which were reported before initiation of ketoconazole. Eight of ten cases (80%) were reported before the combination of ketoconazole and 2 of 10 (20%) episodes after the addition of ketoconazole to tacrolimus (Table 1).
Cost savings
The combination of tacrolimus and ketoconazole resulted in a substantial cost saving. The immunosuppressive therapy cost dropped from USD 872 (SD, 168) per patient to USD 691 (SD, 128) per patient. Given the variation in patient weight and the resulting associated cost of treatment, the mean cost reduction for the sample was 21% (SD, 17). This includes 18 patients with a reduction in cost ranging from (21%-42%), 6 patients with no change in cost (0%) and 1 patient with an increase in cost (+27%).
DISCUSSION
The combination of tacrolimus and ketoconazole resulted in a substantial tacrolimus dose reduction (45% reduction) while maintaining therapeutic levels (5-7 ng/mL) in pediatric transplant patients at FUNDANIER. Findings from this chart review are similar to other reports where the combination has been used in adults[15-18,20,23-26]. In one study from Mexico, eleven patients using the ketoconazole-tacrolimus combination post-transplant were followed for 15 mo (± 10 mo), and demonstrated a 78% dose reduction in tacrolimus while maintaining therapeutic immunosuppressive levels[25]. el-Dahshanet al[15], described a 59% reduction in the tacrolimus dose after six months of therapy in 70 Egyptian post-transplant patients. These patients ranged in age from 16 to 45 years and demonstrated therapeutic tacrolimus levels upon using the ketoconazole combination[20]. After two years of therapy, the same Egyptian cohort successfully maintained immunosuppressive therapy using a reduced dose at 53.8% of the normal tacrolimus dose compared to the control group[27]. Elaminet al[13]also reported a 63% median tacrolimus dose reduction, ranging from 50% to 83% in 30 Sudan patients. The mean age of these patients was 36 ± 12 years. During the one-year follow-up, tacrolimus remained in the therapeutic range, between 5-7 ng/mL. The differences in mean tacrolimus dose showed no significant variation upon ketoconazole initiation, nevertheless, 6 mo after initiation of the combination, there was a significant decrease in the tacrolimus dose. Here we describe the successful use of tacrolimus combined with ketoconazole in a population of pediatric transplant patients.
In our study, none of the patients in the ketoconazole group experienced a decrease in eGFR. We observed an improvement in eGFR when we compared the last visit of patients on the ketoconazole combination and the visit before the combination (P< 0.001). Improvements in graft function with the addition of ketoconazole have been reported in previous studies[18,26]suggesting that a reduction in tacrolimus dose decreases the risk and prevalence of tacrolimus nephrotoxicity. Studies have demonstrated that improvement in eGFR leads to an increase in patient graft survival, and a reduction in graft loss[28,29], we therefore expect that patients using the ketoconazole-tacrolimus combination have an equally high chance of graft survival compared to patients on usual doses of tacrolimus.
In our study, the rejection rate remained unchanged during treatment with the combination of ketoconazole and tacrolimus. However, other similar studies have demonstrated an increase in rejection rates in patients exposed to the combination of ketoconazole and tacrolimus when these patients have a high immunological risk, for example, those with African ethnicity, transplant recipients from cadaveric donors, and previously sensitized patients[16]. We found that the number of rejections did not differ before and after drug combination, most likely because the patient population at FUNDANIER fits into a low immunological risk group characterized as transplant recipients from living donors, HLA compatible and non-sensitized patients. Most importantly, stability in graft function did not fluctuate with the use of combination therapy.
In 2013, the United States Food and Drug Administration and the “Agencia Española de Medicamentos y Productos Sanitarios (AEMPS)” issued a restriction on ketoconazole use due to side effects, primarily hepatotoxicity and adrenal gland insufficiency[21]. Restrictions on ketoconazole were initiated in Guatemala several years later (after this study, 2016), but no policy changes in Guatemala regarding ketoconazole use in adults or children have been made. Despite these warnings and restrictions, we found no hepatotoxicity in our study and this is likely attributed to the small doses used in our pediatric population (1.3 mg/kg/d)[30,31]. Of note, tacrolimus itself is known to cause an increase in transaminases[32], therefore our patients may have been protected by the dose reduction of tacrolimus with the combination of ketoconazole. Findings from our observational study may be supported by larger experimental studies in order to draw conclusions regarding the safety of ketoconazole.
The combination of tacrolimus and ketoconazole resulted in substantial cost savings while preserving the safety profile for our post-transplant patients[16,24,26]. Other similar studies, from Sudan, United Kingdom and Egypt have shown substantial cost reductions, ranging from 52% to 60% when using the combination[15,18,20]. As in many other LMIC, the small percent of GDP dedicated to health care in Guatemala compromises the local government’s ability to provide transplant medication to the population. Cost reduction in transplant medications helps to mitigate barriers in treatment access[33]. Within the socioeconomic setting of FUNDANIER, 18 of 25 patients experienced a cost reduction allowing the clinic to treat a greater number of transplant patients.
We recognize the limitations of this study which are typical of retrospective chart reviews carried out with few patients during short periods of time. For example, liver function tests were the only values recorded from patient charts to document the side effects of ketoconazole use. Metabolic and adrenal side effects, that may be the result of ketoconazole use, were not documented in this study. Nevertheless, if serious adverse events due to ketoconazole use had occurred (i.e., metabolic adverse events, abnormalities in EKG), they would have been reported to the equivalent of the regulatory department in Guatemala and documented within this study. Also, our study represents a small proportion of patients who receive renal transplants in the LMIC setting and may not be representative of all patients in other countries. In the FUNDANIER clinic population, the safety and efficacy of tacrolimus and ketoconazole have been successfully observed in pediatric post-renal transplant patients demonstrating a significant cost reduction. However, larger studies need to be carried out to capture broad safety and efficacy profiles in this patient population. These types of interventions are of added benefit in the LMIC setting where access to medications post-transplant is problematic.
CONCLUSION
Patients experienced an effective dose-reduction of tacrolimus with the administration of ketoconazole. No relevant variations in tacrolimus serum levels, number of rejections, or significant liver toxicity were observed. This allowed a significant cost reduction in the use of pediatric immunosuppressive therapy.
ARTICLE HIGHLIGHTS
Research background
Transplant clinics in developing countries continually aim to provide successful renal transplant care at the lowest possible cost, and have reported that the combined use of ketoconazole with low-dose tacrolimus increases tacrolimus bioavailability through metabolic inhibitionviaP450 3A4.
Research motivation
This combination has been used successfully in adult transplant patients, but has not been demonstrated in pediatric patients. In order to expand successful renal transplant care to children and adolescents at the lowest possible cost, our pediatric renal transplant clinic uses a post-transplant tacrolimus-sparing strategyviainhibition of CYP3A4.
Research objectives
The objective of this study was to identify the changes in tacrolimus dose and plasma concentration associated with the use of ketoconazole as a pharmacokinetic booster. We describe the safety, efficacy and the associated cost reduction of this combination from a retrospective cohort of children with a kidney transplant in the FUNDANIER.
Research methods
We carried out a retrospective observational study, with a pre-post single arm design collecting information from 2011 to 2015 from a cohort of patient records stored in FUNDANIER database before and after the addition of ketoconazole to the usual immunosuppressive protocol. Inclusion criteria for chart review were: Age younger than 18 years, at least 3 mo post-transplantation, currently on the tacrolimus protocol, and switched to ketoconazole/tacrolimus combination during their outpatient transplant clinic attendance. Charts were reviewed to identify the point at which ketoconazole was added to the post-transplant treatment. A total of six documented visits were reviewed for each patient chart during the study: 3 visits prior to ketoconazole initiation and 3 visits after the combination was initiated. An average of 2 mo between each visit was documented.
Research results
Of the 25 patient charts reviewed, 12 (48%) patients were male and the average age of the patients was 13 years. Twenty-four (96%) transplants were from living donors. There was a non-significant difference between the mean tacrolimus doses six months and two months prior to ketoconazole: -0.10 ± 0.04 (95%CI: 0.007, -0.029),P= 0.23. However, the difference between the mean tacrolimus doses six months prior to ketoconazole initiation and six months after ketoconazole addition was significant: 0.06 ± 0.05 (95%CI: -0.034, -0.086)P< 0.001. All tacrolimus doses were reduced by 45% after the addition of ketoconazole. Therapeutic levels of tacrolimus were preserved during the study period and patients demonstrated an improvement in eGFR. The combination of tacrolimus and ketoconazole resulted in a 21% reduction in cost.
Research conclusions
Patients experienced an effective dose-reduction of tacrolimus with the administration of ketoconazole. No relevant variations in tacrolimus serum levels, number of rejections, or significant liver toxicity were observed. This allowed for a safe, efficacious, and significant cost reduction in pediatric immunosuppressive therapy.
Research perspectives
In the FUNDANIER clinic population, the safety and efficacy of tacrolimus and ketoconazole were successfully observed in pediatric post-renal transplant patients demonstrating a significant cost reduction. However, larger studies need to be carried out to capture broad safety and efficacy profiles in this patient population. These types of interventions are of added benefit in the low to middle income countries setting where access to medications post-transplant is problematic.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the detailed review and helpful comments provided by Dr. Alejandro Cerón and Marilia Fuentes for her contributions in data collection.
杂志排行
World Journal of Transplantation的其它文章
- COVID-19 infection in a kidney transplant recipient—special emphasis on pharmacokinetic interactions: A case report
- Intraoperative thromboelastography as a tool to predict postoperative thrombosis during liver transplantation
- Extracellular vesicles as mediators of alloimmunity and their therapeutic potential in liver transplantation
- Obstetrical and gynecologic challenges in the liver transplant patient
- Donor-specific cell-free DNA as a biomarker in liver transplantation: A review
- Lenvatinib as first-line therapy for recurrent hepatocellular carcinoma after liver transplantation: Is the current evidence applicable to these patients?
