Risk score for predicting abdominal complications after coronary artery bypass grafting
2020-11-25DmitryVladimirovichBelovDmitryVictorovichGarbuzenkoKseniaAlekseevnaAbramovskikhNikolayOlegovichArefyev
Dmitry Vladimirovich Belov, Dmitry Victorovich Garbuzenko, Ksenia Alekseevna Abramovskikh, Nikolay Olegovich Arefyev
Abstract
Key Words:Coronary artery bypass grafting;Cardiopulmonary bypass;Abdominal complications;Risk factors;Risk score
INTRODUCTION
Abdominal complications in patients who underwent coronary artery bypass grafting(CABG) with cardiopulmonary bypass (CPB) are rare (1.1%) but associated with high mortality, which reaches 90%[1,2].Predicting the risk of their development may be one of the ways to solve this problem.
One way to reduce mortality in this category of patients is to predict the risk of abdominal complications[3].Our aim was to develop a score for predicting early abdominal complications after CABG with CPB.
MATERIALS AND METHODS
Patients
We retrospectively analyzed individual medical records of 6586 patients who underwent CABG with CPB in the Federal Center of Cardiovascular Surgery of the Ministry of Health of Russia (the city of Chelyabinsk) during 2011-2017.Cases of acute cholecystitis, acute pancreatitis, acute mesenteric ischemia, intestinal necrosis, and acute intestinal obstruction that developed prior to discharge of the patient were referred to as early abdominal complications.
Some patients had postinfarction cardiosclerosis, chronic kidney disease, or type 1 or type 2 diabetes in the anamnesis.
Diabetes was diagnosed using one of the following diagnostic criteria:(1) Classic symptoms of diabetes (polyuria, polydipsia, ketonuria, and rapid weight loss) and a random venous plasma glucose concentration of ≥ 11.1 mmol/L;(2) Fasting glucose concentration of ≥ 7.0 mmol/L in venous plasma or ≥ 6.1 mmol/L in whole blood;and(3) 2-h plasma glucose concentration of ≥ 11.1 mmol/L during a 75-g oral glucose tolerance test.
In each case, measurement of glucose concentration was repeated on a second occasion to confirm the diagnosis[4].
Chronic kidney disease was diagnosed if either of the following was present for >3 mo:Glomerular filtration rate of <60 mL/min/1.73 m2;One or more markers of kidney damage:(1) Albuminuria (ACR ≥ 30 mg/g), (2) Urine sediment abnormalities,(3) Electrolyte and other abnormalities due to tubular disorders, (4) Abnormalities detected by histology, (5) Structural abnormalities detected by imaging, and (6)History of kidney transplantation[5].
图22为不同加工条件下工件表面粗糙度与灰度直方图标准差的实验结果。其中表面粗糙度采用触针式测量仪获得,标准差计算的原始图像为上述便携式系统所获得。显然,随着表面粗糙度的增大,标准差也呈单调增大趋势,在两者之间存在着良好的相关关系。虽然将两者直接拟合成函数关系会出现一定误差,但如果保留在数据库中,便可通过工件表面图像的灰度直方图标准差直接获得加工表面的粗糙度值。
Each medical record contained a completed and signed informed voluntary consent of the patient to the processing and use of his/her personal data and written consent to treatment.Information that was taken into account to evaluate the risk factors for abdominal complications is presented in Table 1.
Assessment of risk factors and statistical analysis
The anamnestic risk factors and the risk factors that occurred within 2 d from the date of surgery were taken for evaluation and compared between patients with early abdominal complications (n= 73) and without them (n= 6513), and the relative risks(RRs) were calculated.Statistical data processing was performed using Statistica 10.0(Statsoft, Tulsa, OK, United States) and SPSS 23.0 (IBM Corp., Armonk, NY, United States).In order to describe the risks, contingency tables were used to calculate the RR and the odds ratio.
An integrated score for assessing the risk of early abdominal complications was created on the basis of the above-mentioned factors by using multivariate logistic regression analysis.The presence or absence of complications was a dependent variable, while the above-mentioned factors were independent variables.Then, the obtained risk score was evaluated by using a receiver operating characteristic (ROC)curve analysis.The presence or absence of early abdominal complications was an outcome variable.The ordinate axis (sensitivity) corresponded to the true positive rate;the abscissa axis (1-specificity) corresponded to the false positive rate.It is generally supposed that the area under the ROC curve that is in the range of 0.9-1.0 should be considered as an indicator of the highest informativeness of the diagnostic method.The range of 0.8-0.9 is good, 0.7-0.8 is acceptable, 0.6-0.7 is weak, and 0.5-0.6 is extremely weak.
RESULTS
In order to determine the probability of early abdominal complications after CABG with CPB, the RRs of their development were analyzed according to the presence and absence of the factors included in the study.Gender and the presence of postinfarction cardiosclerosis, chronic kidney disease, or type 1 or type 2 diabetes in the anamnesis did not affect the occurrence of abdominal complications.
At the same time, abdominal complications most often occurred in patients with extracorporeal membrane oxygenation (RR = 38.7), intra-aortic balloon pump (RR =29.3), and acute myocardial infarction diagnosed after surgery (RR = 21.9).In addition,the development of early abdominal complications was possible in patients who had the following risk factors:Resternotomy (RR = 14.1);ischemic and hemorrhagic brain stroke (RR = 9.4);atrial fibrillation (RR = 8.2);multifocal atherosclerosis, namely the presence of hemodynamically significant stenoses, not only in coronary arteries but also in the brachiocephalic arteries, arteries of the upper and lower extremities, and renal arteries (RR = 4.0);CPB with the duration of more than 125 min (RR = 3.19);a combination of CABG with valve correction (RR = 3.4);aortic clamping time of more than 70 min (RR = 2.5);and age over 70 years (RR = 2.3) (Table 2).
Based on the data obtained, a multivariate logistic regression model analysis was done in order to create an integrated score for assessing the risk of early abdominal complications after CABG with CPB.The presence or absence of complications was a dependent variable and the six most significant risk factors were independent variables (Table 3).
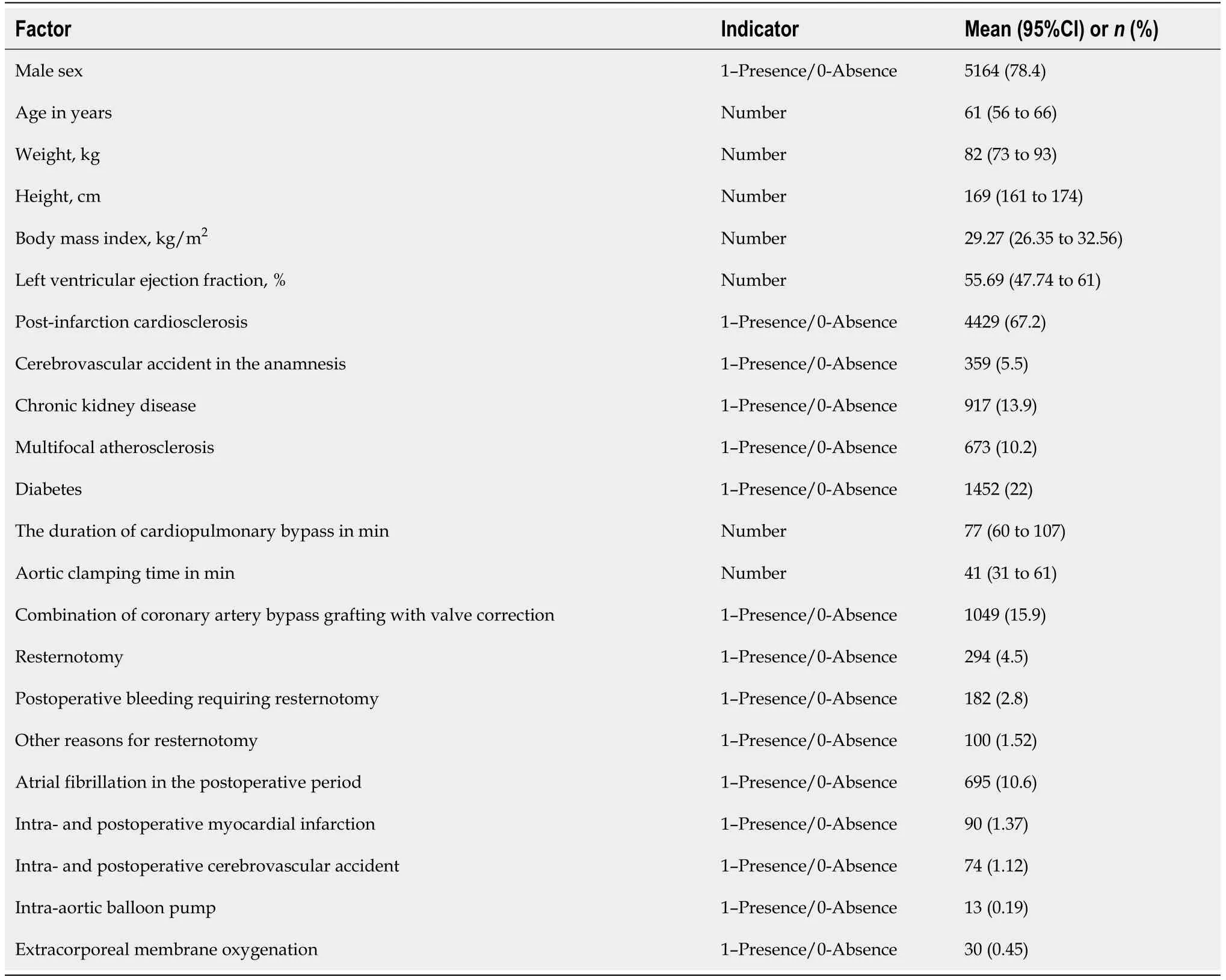
Table 1 Indicators for the evaluation of the risk factors for abdominal complications
It was found that the most significant independent risk factors were extracorporeal membrane oxygenation, intra-aortic balloon pump, and resternotomy in the postoperative period, followed by atrial fibrillation, perioperative acute myocardial infarction, and multifocal atherosclerosis.The average value of the predicted probability was 0.087 ± 0.015 in patients with early abdominal complications after CABG with CPB and 0.0094 ± 0.0003 in patients without these complications.The percentage of correct classification turned out to be 98.9%.
To facilitate the use of this model in practice, each factor was assigned a specific score reflecting its contribution to the total risk of early abdominal complications after CABG with CPB (Table 4).
To evaluate the probability of early abdominal complications for each patient, we calculated the exact predicted probability by using the created logistic regression model and the sum of scores.Next, both of them were compared by using a ROC analysis.The criterion “presence/absence” of complications was used as an outcome variable (Table 5 and Figure 1).
The data presented in Figure 1 indicates that the ROC-curve for the indicator “sum of scores” almost coincides with that for the predicted probability and has a good diagnostic value [area under the curve (referred to as the AUC) = 0.805 ± 0.033,P<0.001].
After the ROC curve analysis, we found it reasonable to divide the curve into four segments that would reflect the low, moderate, high, and very high risk (Table 6).
We also prospectively evaluated our scale in a group of patients who underwent CABG with CPB in 2018.The identification of a high and very high risk group for abdominal complications contributed to early diagnosis in 14 patients.The number of lethal cases was 20 (27.4%) for 2011-2017 and decreased to 2 (14.3%) cases in 2018 (P<0.05).Hence, the hospital mortality decreased to 52.2% in the group of patients with early abdominal complications.
The division of patients into risk groups according to the development of abdominal complications after CABG with CPB suggests a differentiated approach to their management in the postoperative period.Patients with a score of more than 7 according to our score require particular attention.
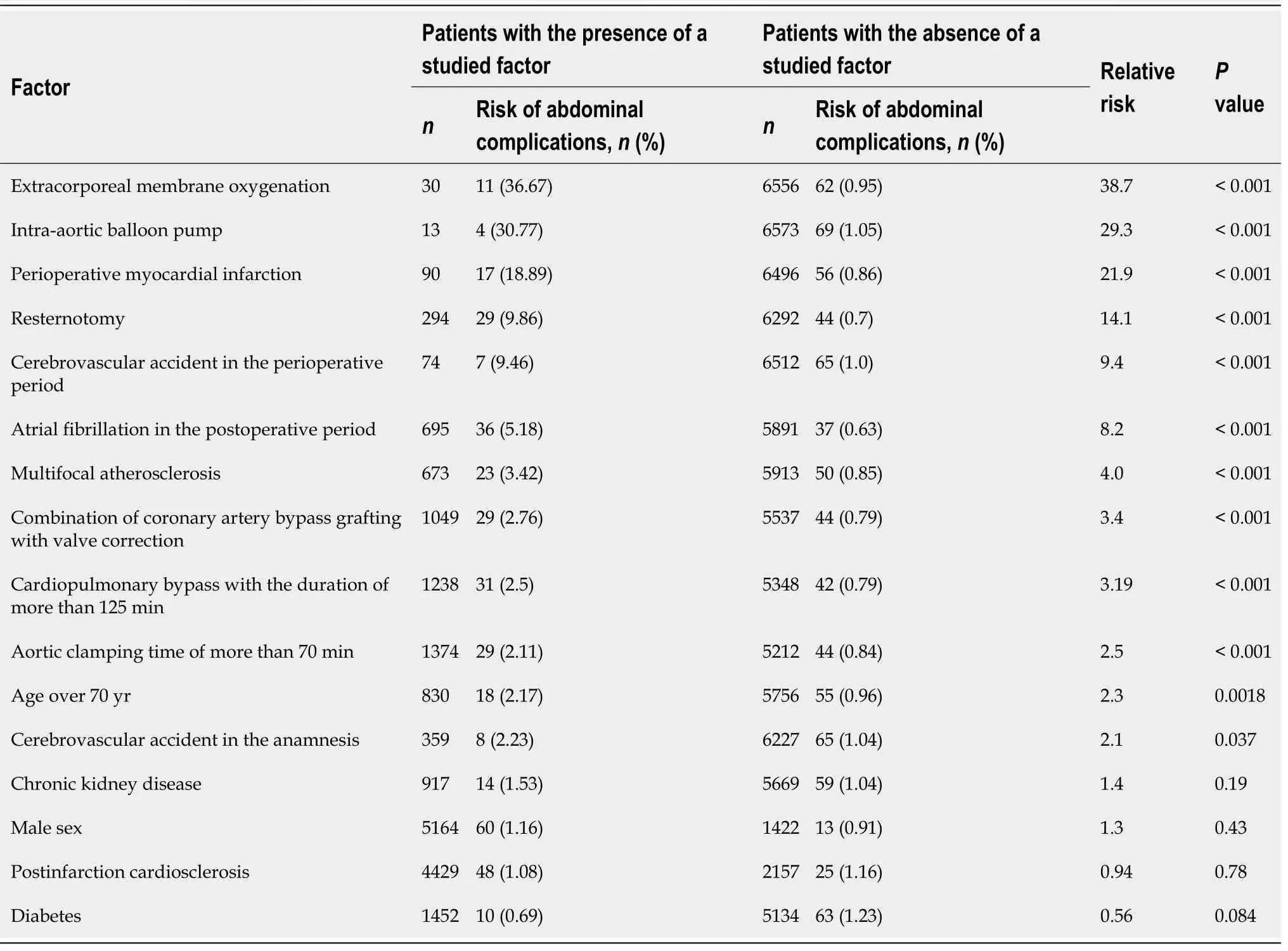
Table 2 Qualitative risk factors of abdominal complications and relative risk of abdominal complications
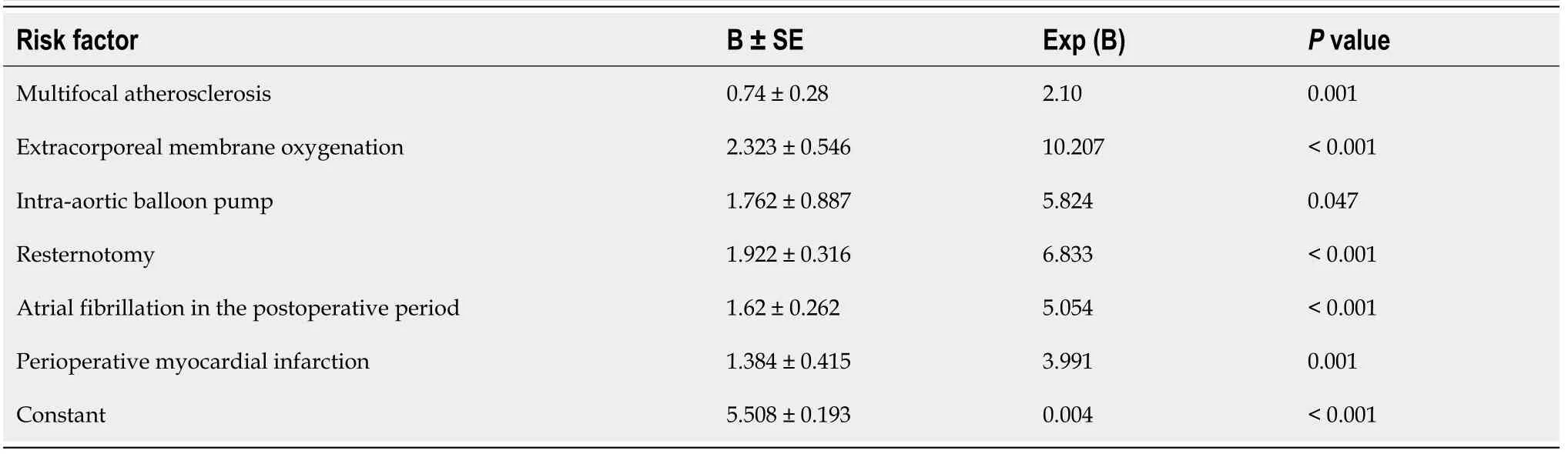
Table 3 Coefficients of the model of multivariate logistic regression (Nagelkerke R Square = 0.966, Р <0.0001)

Table 4 Distribution of scores assigned to the risk factors for abdominal complications

Table 5 Results of receiver operating characteristic curve analysis
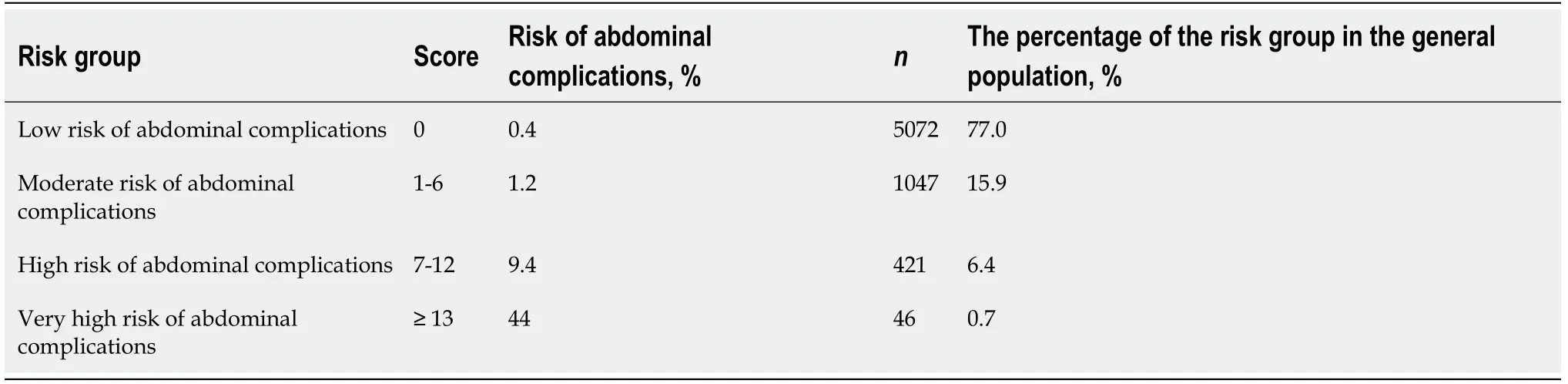
Table 6 Distribution of patients according to the risk groups of abdominal complications after coronary artery bypass grafting with cardiopulmonary bypass
DISCUSSION
Abdominal complications after CABG with CPB are found in 0.2%-5.5% of operated patients[6]and are accompanied by a mortality rate from 11% to 74%[7].Therefore, it is relevant to identify risk factors for predicting the development of abdominal complications.
Long-term CPB is accompanied by a wide range of pathophysiological disorders,which include non-pulsating blood flow, activation of hormonal immunity,anticoagulation, hypothermia, decreased organ perfusion, redistribution of blood flow,threat of embolism, and hyperkalemia[6].It is known that subphysiological blood flow,the release of endogenous vasoconstrictors, including angiotensin II, and the subsequent increase in systemic vascular resistance during CPB may lead to abdominal ischemia, especially if atherosclerotic lesions are present[8,9].
An increase in aortic clamping time may lead to low cardiac output and/or release of inflammatory mediators[10].In addition, if CABG is combined with valve surgery,the risk of mesenteric embolism increases[11].
In patients with postoperative bleeding that requires a resternotomy and in the case when a ventilation time is more than 24 h, there is a decrease in cardiac output and in mean arterial pressure and an increase in vascular resistance of internal organs, which induce temporary hypoperfusion[12].These disorders of splanchnic hemodynamics are exacerbated by the activation of the renin-angiotensin-aldosterone system and increased levels of catecholamines.
Severe acute perioperative myocardial infarction is accompanied by a decrease in cardiac output, systemic hypotension with the centralization of blood circulation, and a decrease in mesenteric perfusion[13,14].They are also facilitated by the following factors:(1) Vasopressors that are used to treat myocardial infarction[15];(2)Prolongation of CPB and mechanical ventilation[16];(3) Resternotomy for reshunting[6,8,17];(4) Extracorporeal membrane oxygenation[16,18];and (5) Intra-aortic balloon counterpulsation, when there is thromboembolism of visceral arteries or their obstruction due to incorrect positioning[17,19].
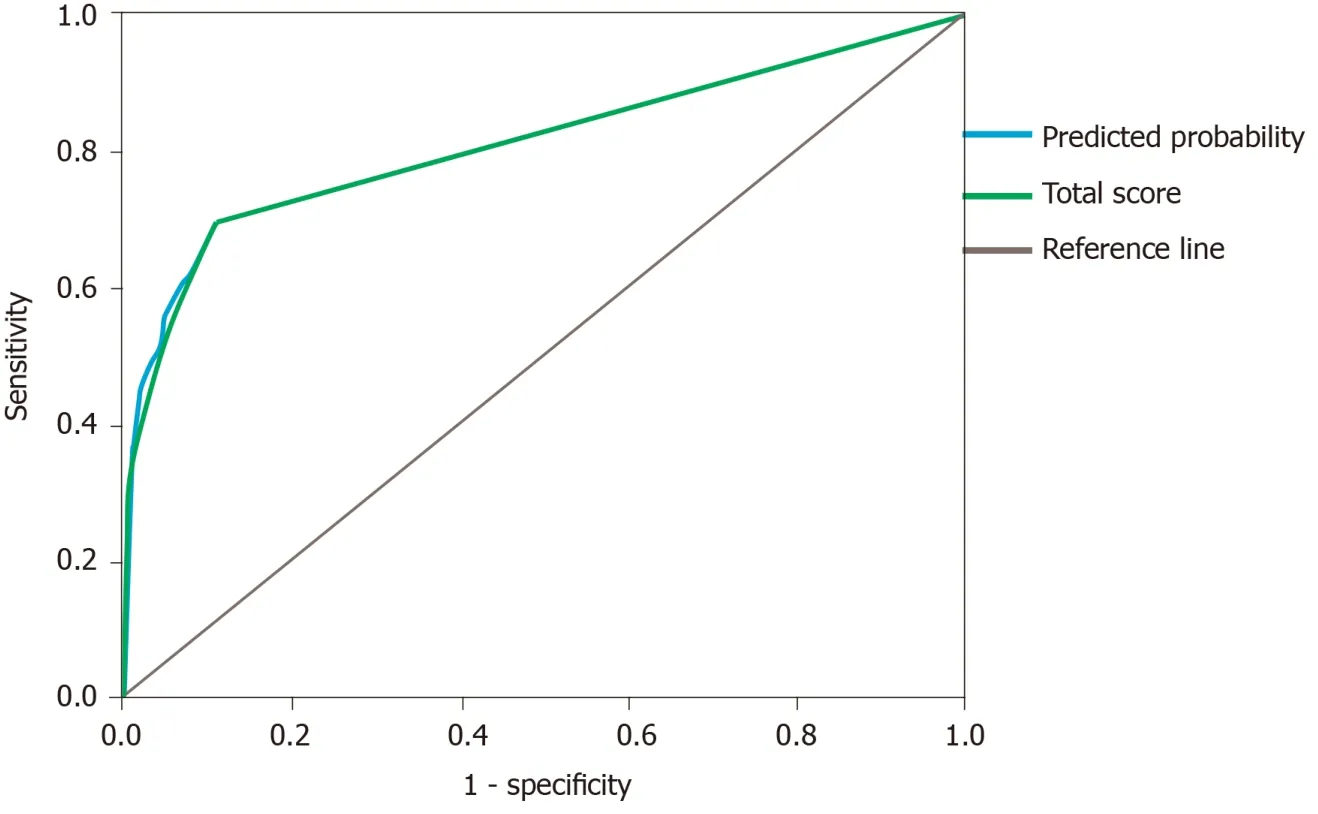
Figure 1 Receiver operating characteristic curve for the predicted probability and the sum of scores.
Atrial fibrillation in the postoperative period contributes to the embolism of the mesenteric vasculature[12], which is also possible during manipulations on the aorta in multifocal atherosclerosis[10].In the latter, hemodynamically insignificant stenoses in the superior mesenteric artery exacerbate the impairment of mesenteric perfusion caused by hypovolemia and hypotension.In addition, multifocal atherosclerosis may act as an independent risk factor of early abdominal complications in patients older than 70 years[18].
Comparing the literature data with the results of our own research, we identified the most significant risk factors and used them to develop a prognostic score, which had a good diagnostic value (AUC = 0.805 ± 0.033,P<0.001).This score allows us to stratify patients with the risk for early abdominal complications after CABG with CPB,which is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality[20].
CONCLUSION
In conclusion, the leading risk factors for early abdominal complications after CABG with CPB in our study were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, acute perioperative myocardial infarction, and the need for performing postoperative resternotomy.According to the developed score, patients with a score of 7 or more had the highest risk of abdominal complications.The score makes it possible to predict the risk of early abdominal complications after CABG with CPB and to stratify patients with the risk for their development, which is important for timely treatment and diagnosis and,ultimately, will help to reduce postoperative mortality.
ARTICLE HIGHLIGHTS
Research background
Abdominal complications in patients who underwent cardiac surgery are rare but the associated mortality varies from 11.0% to 74.0%, which makes the problem relevant.One reason for high mortality rates is late diagnosis.Certain difficulties in diagnosing these complications are associated with the peculiarities of postoperative management and unclear clinical picture due to sedation, analgesia, prolonged mechanical ventilation, and the use of extracorporeal membrane oxygenation.Determining the risk factors for abdominal complications and identifying high-risk groups is an urgent task that may help diagnose abdominal complications and reduce related mortality.
Research motivation
The topic of this study is the identification of leading risk factors for abdominal complications in patients after coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB) and the development of a prediction score based on perioperative predictors to reveal patients at a high risk of abdominal complications.
Research objectives
The objectives of this study were to identify risk factors for abdominal complications according to clinical, laboratory, and imaging findings, to determine their rank influence on the development of early abdominal complications after CABG with CPB,and to develop a risk prediction score.The risk score makes it possible to perform early screening and to develop an algorithm of therapeutic and diagnostic measures for the prevention, early diagnosis, and treatment of this pathology.
Research methods
The factors taken for evaluation were compared between patients with early abdominal complications (n= 73) and without them (n= 6513), and the relative risks were calculated.Statistical data processing was performed using Statistica 10.0(Statsoft, Tulsa, OK, United States) and SPSS 23.0 (IBM Corp., Armonk, NY, United States).In order to describe the risks, contingency tables were used to calculate the relative risk and the odds ratio.An integrated score for assessing the risk of early abdominal complications was created on the basis of the above-mentioned factors by using multivariate logistic regression analysis.The presence or absence of complications was a dependent variable, while the above-mentioned factors were independent variables.Then, the obtained risk score was evaluated by using a receiver operating characteristic curve analysis.The presence or absence of early abdominal complications was an outcome variable.The ordinate axis (sensitivity) corresponded to the true positive rate;the abscissa axis (1-specificity) corresponded to the false positive rate.It is generally supposed that the area under the receiver operating characteristic curve that is in the range of 0.9-1.0 should be considered as an indicator of the highest informativeness of the diagnostic method.The range of 0.8-0.9 is good,0.7-0.8 is acceptable, 0.6-0.7 is weak, and 0.5-0.6 is extremely weak.
Research results
The leading risk factors of the early abdominal complications after CABG with CPB were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, perioperative myocardial infarction, and need for resternotomy in the postoperative period.After calculating a score for each of the leading risk factors, we counted a total score for each particular patient.The highest risk was noted in patients with a total score of 7 or more.Further research may be devoted to a prospective assessment of the proposed scale for the prediction of the risk of abdominal complications and the development of an algorithm for the management of high-risk patients.
Research conclusions
The developed score predicts the risk of early abdominal complications after CABG with CPB and makes it possible to stratify patients by risk groups.It is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality in this group of patients.
Research perspectives
Future studies should prospectively assess the effectiveness of the proposed method,as well as to create a protocol for the prevention, early diagnosis, and treatment of abdominal complications in high-risk patients.
猜你喜欢
杂志排行
World Journal of Cardiology的其它文章
- Safety and efficacy of soluble guanylate cyclase stimulators in patients with heart failure:A systematic review and meta-analysis
- Electronic cigarettes—myocardial infarction, hemodynamic compromise during pregnancy, and systolic and diastolic dysfunction:Minireview
- Upper body peripherally inserted central catheter in pediatric single ventricle patients