The relationship between cellular immune level and diabetic foot in type 2 diabetic patients
2020-10-10RenYanHuangXiaoYangXiaoMingHuLiXiangWangShaoQingYanGuoBinLiu
Ren-Yan Huang, Xiao Yang, Xiao-Ming Hu, Li-Xiang Wang, Shao-Qing Yan, Guo-Bin Liu
Shuguang Hospital Affiliated to Shanghai University of traditional Chinese medicine, vascular surgery of traditional Chinese medicine, 201203
Keywords:Type 2 diabetes Cellular immunity Diabetic foot
ABSTRACT Objective: To to investigate the correlation between the level of immune function and diabetic foot in type 2 diabetic patients. Methods: 76 diabetic patients in our hospital from January 2017 to November 2019 were collected as the observation group (the observation group was divided into two subgroups: 38 cases in DM group and 38 cases in DM + DF group) and 76 healthy people in the same period as the healthy control group. The level of cellular immunity in serum of the observation group and the healthy control group were compared, and the relationship between cellular immunity and diabetic foot was further explored Department. Results: there were significant differences in glycosylated hemoglobin and fasting blood glucose between the two groups (P < 0.001); there were significant differences in CD8, CD25 and CD28 between the two groups (P < 0.001). There were statistical differences in the course and age of diabetes between the two subgroups in the observation group (P < 0.05); there were statistical differences in CD2, CD8, CD25 and CD28 between the two subgroups (P < 0.05). Logistic regression analysis showed that CD8 [or95% CI 0.920 (0.850,0.995)] and CD25 [or95% CI 0.764 (0.619,0.943) were independent influencing factors and risk factors of diabetic foot. Conclusion: the increased levels of CD8 and CD25 may increase the risk of diabetic foot.
1. Introduction
Diabetes is one of the four major chronic diseases with the greatest threat to human health. In its later stage, it often combines with vascular and neuropathy, involving multiple organs such as heart, brain, kidney, peripheral nerve, eyes and feet, which brings certain social and economic pressure to patients [1,2]. Diabetic foot (DF) is not only the second most expensive complication for diabetic patients, but also the main reason for amputation[3]. The incidence of diabetic foot in the late stage of diabetes mellitus patients over 50 years old in China is as high as 8.1%[4]. Epidemiological data show that 9.1 to 26.1 million diabetic patients suffer from foot ulcer every year in the world, with a global prevalence of 6.3% [5]. In recent years, the view that there is abnormal immune regulation in type 2 diabetic patients has been emerging, and it has been found that there is obvious abnormal T cell subsets in type 2 diabetic patients, suggesting that the cellular immune function may be disordered [6,7]. In order to provide reference for clinical diagnosis and treatment, this study aims to investigate the relationship between the level of cellular immunity and diabetic foot by observing the serum levels of healthy people, type 2 diabetic patients and type 2 diabetic foot patients.
2. Data and methods
2.1 Clinical data
From January 2017 to November 2019, patients with type 2 diabetes mellitus, type 2 diabetes mellitus complicated with diabetic foot and healthy physical examination at the same period were selected from the Department of vascular surgery and endocrinology of Shanghai University of traditional Chinese medicine. Excluding the missing data, 152 cases were included, including 38 cases of type 2 diabetes mellitus, 38 cases of type 2 diabetes mellitus with diabetic foot and 76 cases of health examination.
2.2 Diagnostic criteria
The diagnostic standard of diabetes mellitus refers to the diagnostic standard in Chinese diabetes prevention and control guide 2017 edition [8]: fasting blood glucose≥7.0mmol/l; plasma glucose≥ 11.1mmol/l at any time; blood glucose≥11.1mmol/l at 2h after glucose load.
Diagnostic standard of diabetic foot diagnostic standard of diabetic foot refer to Chinese guidelines for diagnosis and treatment of diabetic foot (2017 Diagnostic criteria in [9]: diagnosis basis of diabetic lower extremity angiopathy: (1) in line with the diagnosis of diabetes; (2) with clinical manifestations of lower extremity ischemia; (3) auxiliary detection suggests lower extremity angiopathy. ABI < 0.9 at rest, or ABI > 0.9 at rest, but there are symptoms of lower extremity discomfort during exercise. After treadmill test, ABI is reduced by 15% ~ 20% or imaging suggests that lower extremity exists in blood vessels. The diagnosis of diabetic peripheral neuropathy was based on: (1) abnormal temperature perception; (2) hypoesthesia or disappearance of foot by nylon wire examination; (3) abnormal vibration perception; (4) disappearance of ankle reflex; (5) two or more items of nerve conduction velocity decreased. 2 or more of the above 5 tests can be diagnosed.
2.3 Inclusion and exclusion criteria
Inclusion criteria: meet the diagnostic criteria; age > 18; volunteer to participate in the study and sign the informed consent.
Exclusion criteria: inconformity with inclusion criteria; type I diabetes mellitus; autoimmune disease; immunosuppressant taken within 3 months before blood sampling; serious cardiovascular, liver, kidney and nervous system diseases and psychosis, tumor patients; pregnant and lactating women.
2.4 Data collection
The subjects collected basic information after admission, including patients' gender, age, course of diabetes. Blood samples were collected on an empty stomach in the morning of the next day to detect the level of glucose metabolism (including fasting blood glucose, 2-hour postprandial blood glucose, glycosylated hemoglobin), cellular immune indexes, etc. All blood tests were carried out by the laboratory of Shuguang Hospital Affiliated to Shanghai University of traditional Chinese medicine.
2.5 Statistical analysis
All data are processed by statistical software SPSS 21.0, normal test and normal distribution of measurement data bank Data in (±s); non normal distribution data is represented by (median, interquartile distance), the difference between groups is compared, and the t-test is used for the group comparison when it is consistent with the normality and the variance is homogeneous; the rank sum test is used for the group comparison when it is not subject to the normal distribution; the chi square test is used for the count data; the rank sum test is used for the level data, and the binary logistic regression model is used for the analysis of the impact Factors, P < 0.05 showed statistical difference.
3. Results
3.1 Clinical data
As shown in Table 1, there was no significant difference in gender and age between the observation group and the control group (P > 0.05); there was significant difference in glycosylated hemoglobin and fasting blood glucose between the two groups (P < 0.001). As shown in Table 2, there was no statistical difference in fasting blood glucose, 2-hour postprandial blood glucose and glycosylated hemoglobin between the two subgroups of the observation group (P > 0.05); there was statistical difference in age and diabetes duration between the two subgroups (P < 0.05).
3.2 Comparison of cellular immunity
As shown in Table 3, there was statistical difference in CD8 between the observation group and the control group (P < 0.05), in CD25 and CD28 (P < 0.01); there was no statistical difference in CD3, CD4, CD2, CD19, CD38, CD3 / HLA-DR and CD56 + 16nk between the two groups (P > 0.05). There were significant differences in CD2, CD25, CD8 and CD28 between the two subgroups of the observation group (P < 0.05), but no significant differences in CD3, CD4, CD19, CD38, CD3 / HLA-DR and CD56 + 16NK (P > 0.05).
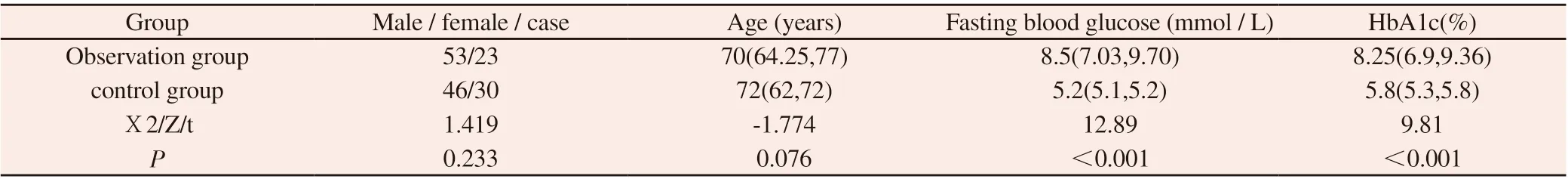
Table 1 Comparison of basic data between the two groups (median, interquartile distance)
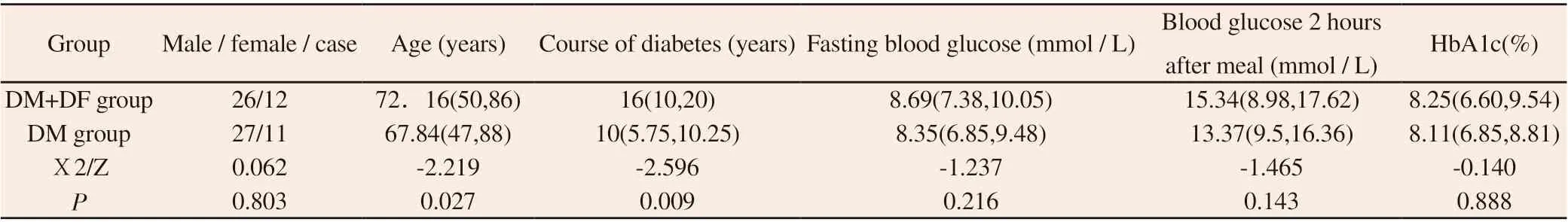
Table 2 Comparison of basic data of patients in observation group (median, interquartile distance)

Table 3 Comparison of serum cellular immune level in each group (median, interquartile distance)
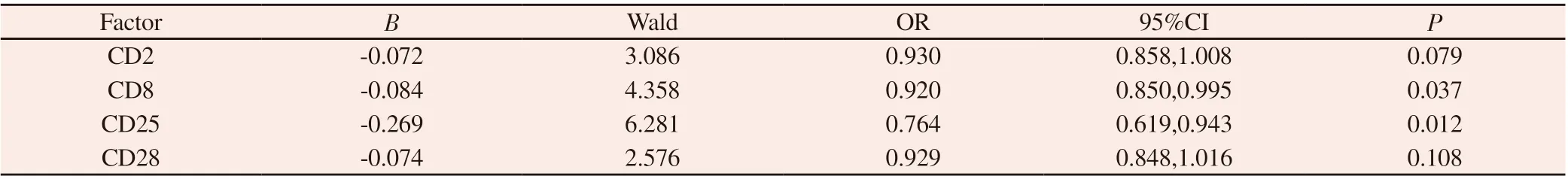
Table 4 logistic regression analysis of influencing factors of diabetic foot
3.3 Risk factors of diabetic foot
The effect of CD2, CD8, CD25 and CD28 on diabetic foot was evaluated by binary logistic regression. Finally, the obtained logistic model is statistically significant, which can correctly classify 71.1% of the subjects. CD8, CD25 were statistically significant (P < 0.05), CD28, CD2 were not statistically significant (P > 0.05), CD8 [or95% CI 0.920 (0.850, 0.995)], CD25 [or95% CI 0.764 (0.619, 0.943) were independent influencing factors of diabetic foot.
4. Discussion
Diabetic foot is a common complication in the later stage of diabetic patients. About 15% ~ 25% of diabetic patients will be complicated with diabetic foot in the later stage. Diabetic foot ulcer (DFU) is more common in the later stage of diabetic foot, which is often hard to heal [10]. Once diabetic foot occurs, it will bring great economic and social burden to patients [11]. According to the relevant research, the medical expenses in the United States for diabetic foot related treatment plan cost up to 18.7 billion US dollars, and the hospitalization expenses for diabetic foot ulcer treatment up to 1.4 billion US dollars [12, 13]. The cost of diabetic foot treatment in South Korea increased from 296 million dollars in 2011 to 441 million dollars in 2016, indicating a significant increase in South Korea's investment in diabetic foot treatment [14]. In a survey on the cost of diabetic foot patients in New Zealand, it was found that the total cost of a diabetic foot rupture can reach more than 10000 US dollars [15]. The average hospitalization cost of diabetic foot patients in China is about 15000 yuan [16]. In addition, diabetic foot is also the main cause of non-traumatic amputation [17]. Diabetic foot accounts for 40% ~ 60% of all non-traumatic low amputation operations [18]. Therefore, if the early intervention can reduce the risk of diabetic foot, it can effectively avoid high medical costs, amputation and even death for diabetic patients.
In recent years, the view that type 2 diabetes may also be an autoimmune disease and the occurrence of diabetic foot may be related to immunity has gradually arisen [19]. It was found that the C-reactive protein was negatively correlated with CD3 +, CD3 + CD4 +, CD3 + CD4 + / D3 + CD8 + and positively correlated with CD3 + CD8 + in diabetic patients with infection, and it was speculated that there was inflammatory reaction in diabetic patients with infection, which also affected the activation of T cells and the activation of T suppressor cells [20]. Li Haiyan[21] found that the levels of CD3 + cells, CD4 + cells and CD4 + / CD8 + cells in patients with diabetic foot complicated with deep infection were lower than those in patients with shallow infection, suggesting that the immune function of patients with diabetic foot infection was related to pathogenic bacteria and infection degree. Zhang lanrong [22] found that diabetic foot is closely related to immune factors such as IgM, IgG, C3 and C4. Jiang chunhuan [23] observed 20 diabetic foot patients and found that the serum IgG, IgM, IgE and IgA of diabetic foot patients were significantly higher than those of normal people, suggesting that there were blood and immunological abnormalities in type 2 diabetic foot patients. Li Fei et al [24] pointed out that diabetic foot ulcer is not only closely related to blood vessels, nerves and other diseases, but also closely related to immune disorders of the body. Immune regulation may become a new direction of diabetic foot treatment. Therefore, this study is based on the cellular immune level in serum to observe whether there is any difference in immune level between healthy people and diabetic patients, and between diabetic patients and patients with diabetic foot.
The results show that there are some differences between diabetic patients and diabetic patients in age and course of diabetes, suggesting that age and course of diabetes may be risk factors for diabetic patients complicated with diabetic foot, which is consistent with our previous research results [25]. It can be seen from the cellular immune level that compared with the healthy people, the level of CD8, CD25 and CD28 in diabetic patients increased. Compared with diabetic patients, the level of CD2, CD8, CD25 and CD28 in diabetic foot patients increased. From the analysis of risk factors, it can be seen that the above CD8 and CD25 indexes are independent influencing factors of diabetic foot, and are negatively correlated with the occurrence of diabetic foot.
In conclusion, the levels of CD8 and CD25 in cellular immunity may be used to predict the risk of diabetic foot in patients with type 2 diabetes. The increase of CD8 and CD25 may be an independent risk factor for diabetic foot. There are some limitations in this study. Only the cases of diabetic foot in diabetic patients are counted, and no specific pathological changes are classified. For example, whether there are vascular diseases and neuropathy, whether the above pathological changes are related to the level of cellular immunity in serum will be our next research direction.
杂志排行
Journal of Hainan Medical College的其它文章
- Mechanism of Ganlu Xiaodu MicroPill against COVID-19 based on network pharmacology and molecular docking method
- Toxicity effects of paclitaxel exposure on Caenorhabditis elegans
- Clinical significance of TnI, hs-CRP and NT-proBNP in the diagnosis of myocardial damage in uremia patients
- Comparative study of 99Tc-MDP and zoledronic acid in the treatment of osteoporosis
- Clinical study on the treatment of bronchiectasis in remission period by embedding thread combined with Jianpi Qushi Huayu plaster
- Research on the rules of Professor Dai Xiaohua's medication for coronary heart disease and chronic heart failure based on data mining
