Current status of Helicobacter pylori eradication and risk factors for eradication failure
2020-09-23TianLianYanJianGuoGaoJingHuaWangDanChenChaoLuChengFuXu
Tian-Lian Yan, Jian-Guo Gao, Jing-Hua Wang, Dan Chen, Chao Lu, Cheng-Fu Xu
Abstract
Key words: Helicobacter pylori; Eradication; Quadruple therapy; Proton pump inhibitor; Retrospective study
INTRODUCTION
Helicobacter pylori(H. pylori) is a widespread bacterium that typically infects the human gastric mucosa. The infection may induce numerous gastrointestinal diseases, including gastritis, peptic ulcer, gastric carcinoma, and gastric lymphoma[1-3], and it is also associated with significant extragastric diseases, such as idiopathic thrombocytopenic purpura, idiopathic iron deficiency anemia, and vitamin B12 deficiency[4]. Epidemical studies reported thatH. pyloriaffects 24%-50% of people in industrialized nations and up to 79% of those in less-developed countries.H. pyloriinfection is a worldwide threat to public health[5].
Currently,H. pyloriinfection is considered the most important (yet controllable) risk factor for intestinal gastric cancer, as it accounts for the vast majority of cases of gastric cancer, which generally develops from a normal gastric mucosa to superficial gastritis and pre-neoplastic lesions[6]. A large number of studies have confirmed thatH. pyloriscreening and treatment strategies could prevent gastric cancer in a cost-effective way, especially before the appearance of pre-neoplastic lesions and in high-risk areas[7-9]. In recent decades, the urea breath test has been widely used to detectH. pyloriinfection not only in specialized hospitals but also in physical examination centers and community hospitals in China. This has led to large numbers of asymptomatic patients being referred to specialized clinics for treatment[10].
However,H. pylorieradication therapies are facing decreasing eradication rates, mainly owing to antimicrobial resistance, and are partially influenced by the efficacy of acid-suppressive drugs[11]. Recent guidelines recommend 14-d combination therapies with two types of antibiotics, a proton pump inhibitor (PPI) and bismuth[12,13]. Studies using susceptibility tests based onH. pyloristrains culturedin vitroand prospective studies with relatively small sample sizes reported increasing resistance rates to clarithromycin, metronidazole, and levofloxacin, while resistance rates to amoxicillin, tetracycline, and furazolidone were low[14,15]. However, there is a scarcity of eradication data from large-sample size studies of real-world practice, which are important for formulating future guidelines and conducting clinical work in China. Moreover, it remains uncertain whether the acidic environment in the stomach during therapy, prior therapy, and demographic characteristics are related to eradication failure.
In this study, we reviewed the medical records of a large series ofH. pylori-positive patients from the First Affiliated Hospital, Zhejiang University School of Medicine. We evaluated theH. pylorieradication status in the local population of Eastern China in real clinical practice and explored factors related to therapy failure.
MATERIALS AND METHODS
Study design and research subjects
All of the patients diagnosed withH. pyloriinfection in the electronic medical records obtained from the First Affiliated Hospital, Zhejiang University School of Medicine (Hangzhou, China) between June 2018 and May 2019 were included. In addition, separate databases of laboratory test, endoscopy, and pathology results were searched. Anonymized information of each patient was linked to a unique identification number. Two clinicians checked the therapy regimens independently.
The inclusion criteria were the following: (1) The general and clinical information and the prescription records were complete and available; (2) TheH. pyloriinfection status before treatment was directly determined by one or more of the standard detection methods (urea breath test, histologic staining, and/or bacterial culture); (3) Patients received quadruple therapy forH. pyloriinfection according to the standard antibiotic combinations and dosages of the “Fifth Chinese National Consensus Report on the management ofH. pyloriinfection,” which highlights bismuth-containing quadruple therapy (PPI, bismuth, and two antibiotics) as the main empirical therapy forH. pylorieradication[12]; (4) The treatment lasted 14 d; and (5) Test of cure: TheH. pyloristatus was confirmed by urea breath test 4-8 wk after the end of treatment.
The exclusion criteria were the following: (1) Patients who were lost to follow-up or changed the therapy regimen; and (2) Therapies that included other drugs, such as probiotics and/or Chinese traditional medicines.
The study protocol was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine.
Statistical analysis
Statistical analyses were performed using SPSS version 22.0 (IBM SPSS Statistics, IBM Corporation, Armonk, NY, USA). Categorical variables are displayed as frequencies and proportions (%). Continuous variables are presented as the mean and standard deviation (SD) unless otherwise stated. Continuous variables were compared by Student’st-test or one-way ANOVA. Categorical variables were compared using theχ2test. The Cochran-Armitage trend test was used to analyzeH. pylorieradication rates in the different age groups. A stepwise logistic regression analysis was performed to examine the relationship betweenH. pylorieradication failure and risk factors (probability to enter = 0.05 and probability to remove = 0.10). Two-tailedPvalues < 0.05 were considered to indicate statistical significance.
RESULTS
Patient selection and clinical characteristics
A total of 2652H. pylori-positive patients received 14-d quadruple therapy between June 2018 and May 2019 and took the urea breath test 4-8 wk later. We excluded 34 patients because the therapy regimens were changed due to drug intolerance. We also excluded another five patients who received amoxicillin plus metronidazole-based therapy and three patients who received levofloxacin plus metronidazole-based therapy owing to the small sample sizes. Finally, 2610 patients (1088 men and 1522 women) with a mean age of 44.53 ± 14.43 years were included in the analyses (Figure 1).
Of the 2610 patients, 373 (14.3%) had a prior history ofH. pyloritreatment, and 2237 (85.7%) did not (Table 1). One or more symptoms were observed in 1301 (49.8%) patients, including upper abdominal pain (15.6%), abdominal distension (24.6%), nausea (5.3%), acid regurgitation or heartburn (9.6%), bitter taste in the mouth (6.0%), belching (8.6%), increased stool frequency (5.5%), and others (5.8%). A total of 1390 (53.3%) patients underwent gastroscopy before or after therapy, 244 had at least one peptic ulcer, 416 had atrophy, intestinal metaplasia, or dysplasia, as determined by biopsy histology, and 17 were diagnosed with MALT lymphoma or gastric cancer (Table 1).

Table 1 Demographic and clinical characteristics of patients with Helicobacter pylori infection
Helicobacter pylori eradication rates
Of the 2610 patients, eradication was successful in 1999 (76.6%) patients. The eradication rate of each antibiotic combination is illustrated in Figure 2. Amoxicillinbased therapy showed a significantly higher eradication rate than other regimens (83.0%vs69.0%,P< 0.001). Therapy consisting of amoxicillin plus clarithromycin achieved the highest eradication rate (83.5%; 95%CI: 81.4%-85.5%), followed by therapy that consisted of amoxicillin plus furazolidone (79.4%; 95%CI: 69.4%-89.4%), amoxicillin plus levofloxacin (78.9%; 95%CI: 69.8%-88.1%), clarithromycin plus levofloxacin (72.1%; 95%CI: 69.3%-74.9%), levofloxacin plus furazolidone (63.2%; 95%CI: 41.5%-84.8%), clarithromycin plus metronidazole (54.7%; 95%CI: 46.7%-62.7%), and clarithromycin plus furazolidone (44.1%; 95%CI: 27.4%-60.8%). The eradication rate was not significantly different among the three different amoxicillin-based therapies (Figure 2).
We also found that the choice of PPI is a factor that influenced the eradication rate (Table 2). Therapy with esomeprazole achieved the highest eradication rate (81.8%; 95%CI: 78.2%-84.0%), followed by therapies with rabeprazole (78.6%; 95%CI: 75.8%-81.4%), lansoprazole (78.2%; 95%CI: 67.3%-89.1%), pantoprazole (74.0%; 95%CI: 70.5%-77.5%), and omeprazole (68.6%; 95%CI: 64.1%-73.1%). Eradication rates of therapieswith omeprazole and pantoprazole were significantly lower than that of therapy with esomeprazole (P< 0.005). Eradication rates of therapies with rabeprazole and lansoprazole were lower than that of therapy with esomeprazole, but the difference was not statistically significant. Therapies with esomeprazole showed a significantly higher overall eradication rate than those with other PPIs (81.8%vs74.9%,χ2= 10.755,P= 0.001).

Table 2 Eradication rates of specific Helicobacter pylori regimens classified by proton pump inhibitor

Figure 1 Study flowchart.
In addition, we found that the eradication rate showed a significant decreasing trend with increase in age (Figure 3). The eradication rates were 84.0%, 79.3%, 74.5%, 70.8%, and 72.4% in patients aged < 30, 30-39, 40-49, 50-59, and ≥ 60 years, respectively (Pfor trend < 0.001).
Subgroup analysis
The eradication rates for primary and rescue therapies were 78.3% (95%CI: 76.6%-80.0%) and 66.5% (95%CI: 61.7%-71.3%), respectively. Primary therapy showed a higher eradication rate than rescue therapy (P< 0.001). The amoxicillin-containing regimens showed superiority in primary therapy, and amoxicillin- and furazolidonecontaining regimens achieved the highest eradication rate (80.8%; 95%CI: 70.1%-91.5%) in rescue therapy, followed by amoxicillin- and clarithromycin-containing regimens (77.1%; 95%CI: 69.1%-85.2%).
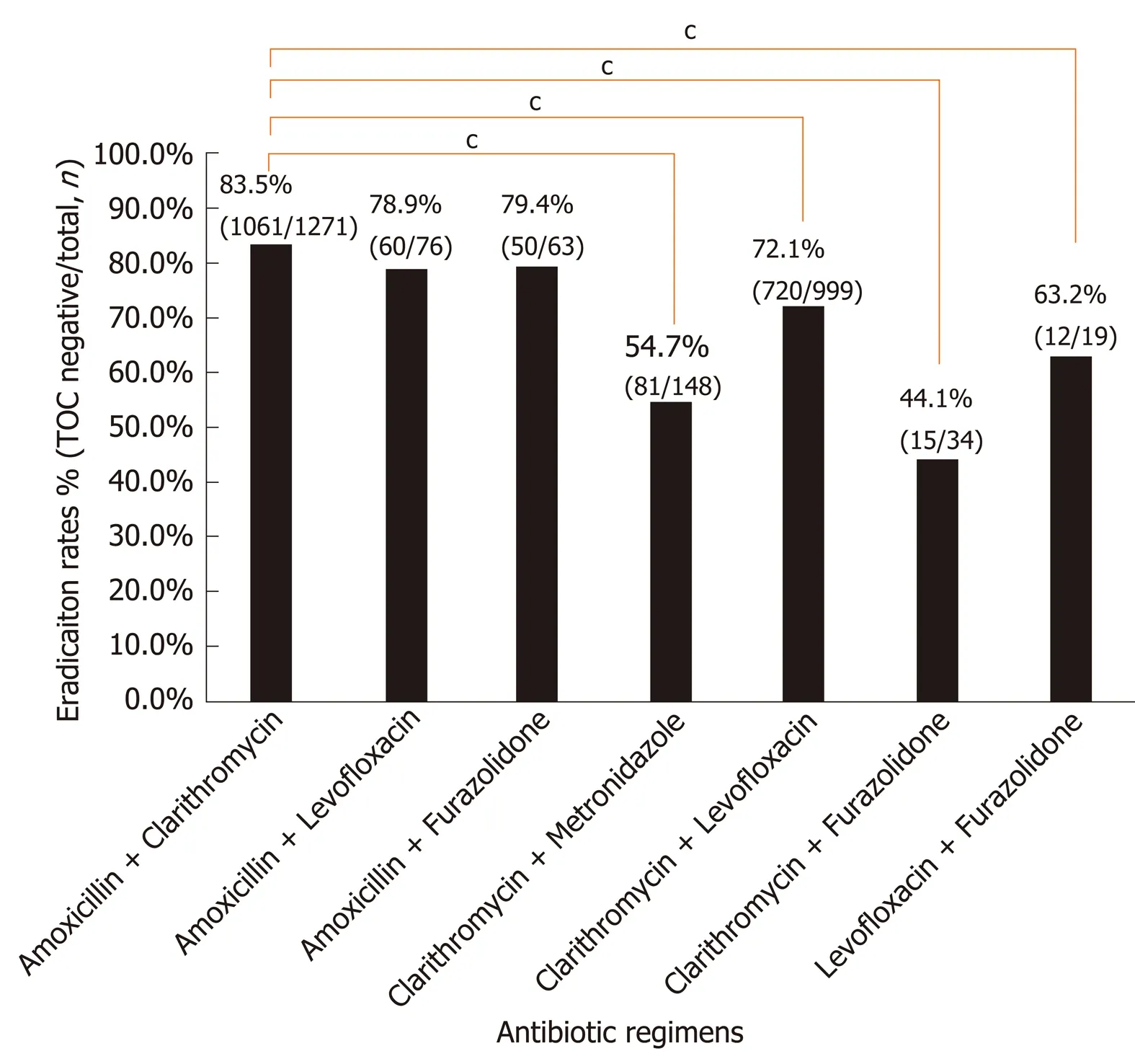
Figure 2 Eradication rates of Helicobacter pylori treatment regimens classified by antibiotic combination. cP < 0.001 compared with the regimen containing amoxicillin plus clarithromycin.
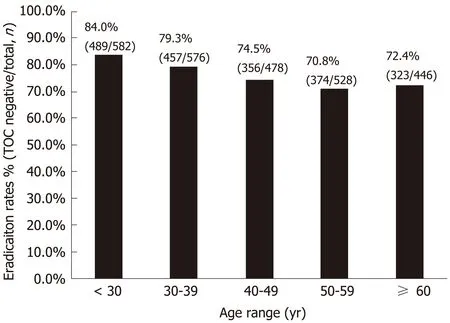
Figure 3 Eradication rates in specific patient age ranges.
The regimens containing amoxicillin plus levofloxacin, clarithromycin plus levofloxacin, and clarithromycin plus metronidazole showed lower eradication rates in rescue therapy than in primary therapy (P< 0.05). The regimens containing amoxicillin plus clarithromycin, amoxicillin plus furazolidone, clarithromycin plus furazolidone, and levofloxacin plus furazolidone showed no significant difference in eradication rates between primary and rescue therapy (Table 3).
Risk factors for eradication failure
We performed stepwise logistic regression analyses to explore factors associated with eradication failure. The univariate analysis showed that age, prior therapy, antibiotic regimen, and choice of PPI were significantly associated with the risk of eradication failure, while gender and chief complaint were not. The multivariate logistic regression analysis confirmed that older age and prior therapy were significantly associated with an increased risk of eradication failure (P< 0.001). Setting the regimen containing amoxicillin plus clarithromycin as the reference group, regimens containing clarithromycin plus levofloxacin, clarithromycin plus metronidazole, and clarithromycin plus furazolidone all showed a higher odds of eradication failure (P<0.001). Other regimens were not significantly associated with eradication failure. Setting regimens containing esomeprazole as the reference group, the regimens containing omeprazole and pantoprazole showed a significantly higher risk of eradication failure (P< 0.05), whereas rabeprazole and lansoprazole were not significantly associated with eradication failure (Table 4).

Table 3 Subgroup comparison of eradication rates
DISCUSSION
In this large-sized retrospective study, we evaluated the efficiency of various standard 14-d quadruple regimens recommended forH. pyloritreatment. We found that amoxicillin-based quadruple therapy was superior, and amoxicillin- and furazolidonebased therapy showed a high eradication rate in rescue therapy. Our multivariate analysis showed that older age, prior therapy, and application of omeprazole or pantoprazole increased the risk of eradication failure.
This study reports an unsatisfactory eradication rate of 76.6%, even though prescription was in strict accordance with guidelines. In a single-center retrospective study performed by another hospital in Eastern China, 992 patients received 10 to 14 d of quadruple therapy forH. pyloriinfection based on furazolidone and amoxicillin between January and December 2015. The eradication rate of rescue therapy was 91.3%[16]. However, in our study, the eradication rate of 14-d quadruple rescue therapy based on amoxicillin and furazolidone was only 80.8%. One possible reason for this discrepancy is thatH. pyloriresistance rates to antibiotics have increased during the past years. However, antibiotic resistance ofH. pyloricultures was not investigated for all of the enrolled patients. Because of its cost and relatively low sensitivity,H. pyloriculture is not recommended for routine diagnosis ofH. pyloriinfection[17]. Another reason might be the lack of tetracycline-containing regimens and the low proportion of furazolidone-containing regimens, the resistance rates of which are relatively low in China[18]. Unfortunately, most hospitals in China are facing shortages of tetracycline, which yielded effective anti-H. pyloriresults in the USA[19]. Moreover, the potentially severe side effects of furazolidone limit its widespread application in initial empirictherapy. Therefore, furazolidone-containing regimens are more frequently used for patients with refractoryH. pyloriinfection[20].

Table 4 Univariate and multivariate analyses of risk factors for eradication failure
In this study, we also observed that only half of the patients had symptoms, and the other half were asymptomatic. As more asymptomatic patients are referred to the hospital forH. pyloritherapy, we predict that antibiotic resistance ofH. pyloriwill increase in the near future. It is, therefore, worthwhile to explore methods to improve the eradication rate. A previous study reported that patient compliance is an indispensable factor influencing treatment results[21]. In addition, high-dose PPI and amoxicillin dual therapy could decrease the use of unnecessary antibiotics, which is a promising alternative approach[22,23]. Adjuvant therapy, including specific probiotics or vitamins, also showed good results, although more evidence will be needed[24].
Consistent with previous studies, our results also suggest that acid-suppressive drugs play an important role in eradication therapy. A previous meta-analysis reported that regimens containing new-generation PPIs (esomeprazole or rabeprazole) showed a significantly higher eradication rate than those containing first-generation PPIs (omeprazole, lansoprazole, or pantoprazole)[25]. In this study, we also found a significantly lower eradication rate for omeprazole- or pantoprazole-containing regimens than for those containing new-generation PPIs. However, the difference in eradication rates between regimens containing lansoprazole and new-generation PPIs was not significant. Due to the relatively small size of the lansoprazole group, this result needs to be confirmed in future studies. The main role of PPIs in the treatment ofH. pyloriinfections is to elevate the gastric pH, leading to an increase in the population of dividingH. pylori. Subsequently, the bacteria become more susceptible to antibiotics, such as amoxicillin and clarithromycin[26]. Selecting a PPI with a stable effect and high efficacy that is weakly influenced by CYP2C19 genotypes can improve the eradication rate[12]. In addition to the modification of dual therapy by high-dose PPI mentioned above, vonoprazan, a first-in-class potassium-competitive acid blocker, was recently reported to be an independent factor for successfulH. pylorieradication in both primary and rescue therapy[27].
In this study, a significant trend of decreasing eradication rates was observed with increasing age, which is consistent with previous reports[27,28]. Possible reasons include lower tolerance to and compliance with therapy, more potential complications, increased risks of drug side effects, and increased antibiotic resistance because of higher accumulated antibiotic consumption[29]. In contrast, no significant difference in the eradication rate or frequency of adverse effects between the elderly group and the younger group was found in other studies[30,31].
Several limitations should be considered when explaining the results of this study. First, because of its retrospective nature, the classification of primary or rescue therapy was completely dependent on the electronic medical records. The percentage of rescue therapy might be underestimated if the patients’ medical histories were not fully recorded, and some rescue therapy cases might be misclassified as primary therapy, resulting in a relatively low eradication rate in the primary therapy group. Second, patient compliance was not analyzed in this study. However, all of the patients enrolled in this study completed the urea breath test 4-8 wk after finishing treatment, indicating a relatively high compliance. Third, similar to previous reports ofH. pylorieradication, the data used in this study were extracted from a single center. The results may not be extrapolated to other areas, especially if resistance rates vary geographically. In addition, the small sample sizes of some regimens, such as the furazolidone-containing regimens in subgroup analysis of primary therapy and lansoprazole-containing regimens, limit the reliability of the corresponding results.
In conclusion, this study revealed an unsatisfactoryH. pylorieradication rate of 76.6% in Eastern China. Amoxicillin-containing 14-d quadruple regimens have the highest eradication rate in primary therapy, and amoxicillin- and furazolidonecontaining regimens show superiority in rescue therapy. An inferiority of omeprazole and pantoprazole is also observed. These findings may be helpful to improve the eradication rate of anti-H. pyloritherapy.
ARTICLE HIGHLIGHTS

Research conclusions
This study confirmed that the total eradication rate is 76.6% in eastern China. Amoxicillin-containing regimens are superior to other regimens. Age, prior therapy, and use of omeprazole or pantoprazole are independent risk factors for eradication failure.
Research perspectives
This study can improve the choice of antibiotics and proton pump inhibitors and indicates that in clinical practice, attention should be paid to elderly patients and rescue therapy. Further prospective research focusing on optimizing the treatment strategies considering these factors is required.
杂志排行
World Journal of Gastroenterology的其它文章
- Association between human leukocyte antigen gene polymorphisms and multiple EPIYA-C repeats in gastrointestinal disorders
- Promising xenograft animal model recapitulating the features of human pancreatic cancer
- Immune and microRNA responses to Helicobacter muridarum infection and indole-3-carbinol during colitis
- Etiology and management of liver injury in patients with COVID-19
- Novel virulence factor dupA of Helicobacter pylori as an important risk determinant for disease manifestation: An overview
- Inactive matrix Gla protein is elevated in patients with inflammatory bowel disease
