Autoimmune hepatitis in a patient with immunoglobulin A nephropathy:A case report
2020-09-18YouHyunJeonDaWoonKimSoJeongLeeYoungJooParkHyoJinKimMiyeunHanIlYoungKimDongWonLeeSangHeonSongSooBongLeeEunYoungSeong
You Hyun Jeon,Da Woon Kim,So Jeong Lee,Young Joo Park,Hyo Jin Kim,Miyeun Han,Il Young Kim,Dong Won Lee,Sang Heon Song,Soo Bong Lee,Eun Young Seong
You Hyun Jeon,Da Woon Kim,Department of Internal Medicine,Pusan National University School of Medicine,Busan 49241,South Korea
So Jeong Lee,Department of Pathology,Pusan National University Hospital,Busan 49241,South Korea
Young Joo Park,Division of Gastroenterology,Department of Internal Medicine,Biomedical Research Institute,Pusan National University Hospital,Busan 49241,South Korea
Hyo Jin Kim,Miyeun Han,Sang Heon Song,Eun Young Seong,Division of Nephrology,Department of Internal Medicine,Biomedical Research Institute,Pusan National University Hospital,Busan 49241,South Korea
Il Young Kim,Dong Won Lee,Soo Bong Lee,Division of Nephrology,Department of Internal Medicine,Pusan National University Yangsan Hospital,Yangsan 626-770,South Korea
Abstract
Key words:Immunoglobulin A nephropathy;Secondary immunoglobulin A nephropathy;Autoimmune hepatitis;Liver transplantation;Case report
INTRODUCTION
Immunoglobulin A nephropathy (IgAN) is the most prevalent glomerular disease worldwide and is an important cause of end-stage kidney disease.IgAN is an autoimmune disorder characterized by diffuse mesangial deposition of immunoglobulin A (IgA)[1].The accumulation of mesangial IgA associated with chronic liver disease,such as alcoholic liver cirrhosis and chronic viral hepatitis,is the most common form of secondary IgAN[2].Secondary IgAN is usually clinically silent,and the most common symptom is microscopic hematuria.IgAN has also been reported to be associated with other autoimmune conditions,including ankylosing spondylitis,psoriasis,inflammatory bowel disease and Hashimoto’s thyroiditis[2,3].However,few cases have been reported in the literature of IgAN associated with autoimmune hepatitis (AIH).
CASE PRESENTATION
Chief complaints
A 63-year-old woman presented with right upper quadrant abdominal discomfort.
History of present illness
The patient’s symptoms developed insidiously over 3 d.She did not show any symptoms related to portal hypertension.
History of past illness
Two weeks ago,she presented to our hospital with proteinuria of approximately 1350 mg/d and hematuria and was diagnosed with IgAN.Light microscopic findings of kidney biopsy showed a moderate increase in mesangial matrix and mesangial cellularity (Figure 1A) with focal severe tubular atrophy and interstitial infiltration of mononuclear cells.Out of 37 glomeruli,2 glomeruli (5%) showed global sclerosis.Immunofluorescence microscopy showed predominant mesangial IgA staining(Figure 1B) and C3 staining (Figure 1C).Electron microscopy revealed mesangial electron-dense deposits and focal effacement of the epithelial cell foot processes(Figure 1D).Laboratory findings were as follows:aspartate aminotransferase (AST),20 IU/L;alanine aminotransferase (ALT),8 IU/L;and serum creatinine,1.21 mg/dL.She was not taking any other medications except an angiotensin II receptor blocker.
锥形瓶不能直接加热,采用试管可避免锥形瓶直接炸裂,发生意外,还可以减少能量损耗。一般情况下,一粒种子燃烧一分钟就能将10 mL水煮沸。若容积过大,不仅温度变化不明显,而且需要使用较大口径的试管,从而还需要对易拉罐拉环口进一步裁剪,所以量取容积为15 mL的水。

Figure 1 Kidney histopathology.A:Light microscopy,mesangial hypercellularity in a glomerulus;B:Immunofluorescence microscopy,the staining of immunoglobulin A (3+);C:Immunofluorescence microscopy;the staining of C3 (1+);D:Electron microscopy,mesangial electron- dense deposits.
Physical examination
On admission,she had a height of 155.5 cm,a weight of 53.7 kg,a blood pressure of 120/70 mmHg,a regular heart rate of 64 bpm,and a temperature of 36.1 °C.The patient had mild right upper quadrant pain and tenderness and icteric sclera.She denied taking any new medication or alcohol consumption.
Laboratory examinations
Laboratory findings were as follows:white blood cell count,4090/µL;hemoglobin,10.6 g/dL;platelet count,99 × 10³/µL;AST,771 IU/L;ALT,488 IU/L;alkaline phosphatase,92 IU/L;total bilirubin,3.04 mg/dL;direct bilirubin,1.86 mg/dL;total protein,6.89 g/dL;albumin,3.13 g/dL;and prothrombin international normalized ratio,1.57.Serum creatinine and estimated glomerular filtration rate were 1.26 mg/dL and 45.6 mL/min per 1.73 m²,respectively,similar to the values 2 wk prior.She was negative for anti-hepatitis B surface antigen,anti-hepatitis B core antibody,antihepatitis C virus antibody and anti-hepatitis A virus IgM.The results of immunological studies and serum iron and copper studies are shown in Tables 1 and 2.
Imaging examinations
A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a distal common bile duct (CBD) stone with mild upstream bile duct dilatation and an intrahepatic portosystemic shunt in the left lobe of the liver.There was not any evidence of chronic liver injury or portal hypertension such as esophageal varix,splenomegaly and ascites.Endoscopic retrograde cholangiopancreatography showed CBD stone without bile duct narrowing.

Table 1 The results of immunological studies
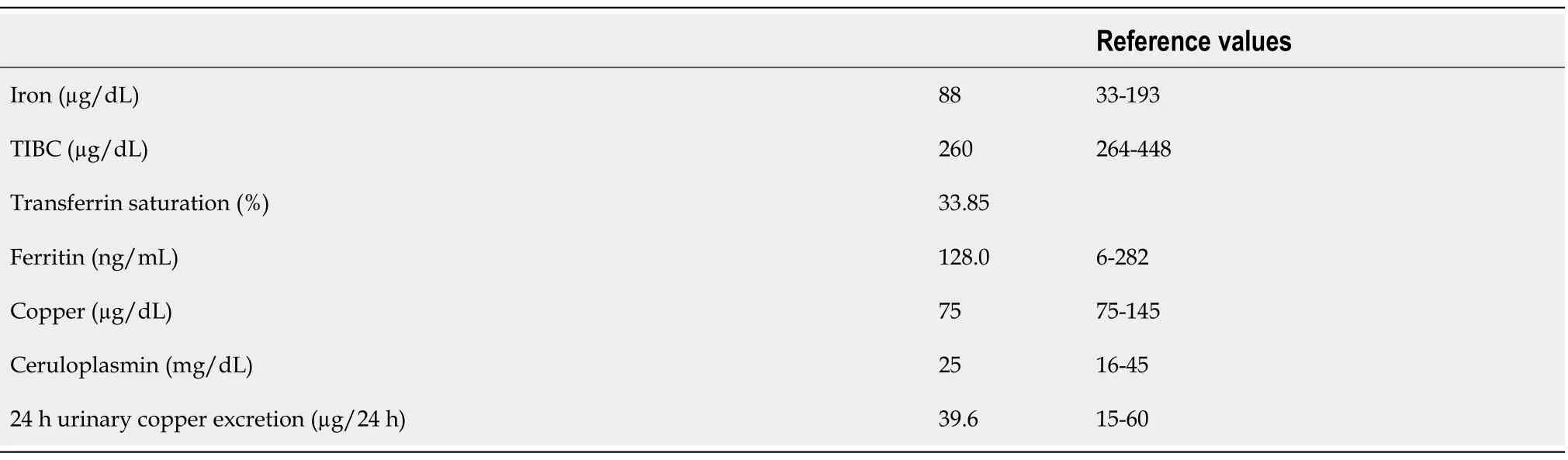
Table 2 The results of serum iron and copper studies
FINAL DIAGNOSIS
After endoscopic removal of CBD stones,liver enzyme levels started to decrease.On the fourth day,AST,ALT and total bilirubin gradually increased to 896 IU/L,579 IU/L,and 5.05 mg/dL,respectively.Symptoms related to portal hypertension,including ascites and peripheral edema,occurred.Based on the abovementioned findings,the diagnosis of AIH was made according to the simplified scoring system of the International Autoimmune Hepatitis Group[4].The score prior to steroid therapy was 6 points:Antinuclear antibodies (2),IgG (2) and absence of viral hepatitis (2).
TREATMENT
She was treated with prednisolone 0.5 mg/kg in combination with azathioprine for 2 wk.Despite the treatment,liver function rapidly deteriorated,and hepatorenal syndrome requiring renal replacement therapy developed subsequently.The patient was not exposed to the nephrotoxic agents and had no episode of bleeding or septic shock.The model for end-stage liver disease score was 37 points at the time of waiting list registration for liver transplantation.Approximately two months after hospitalization,she underwent living-donor liver transplantation from her son.Hepatectomy specimens showed submassive necrosis.Prominent necrosis involved entire lobules in most of the liver parenchyma (Figure 2A),and the remaining parenchyma showed canalicular type cholestasis (Figure 2B).
OUTCOME AND FOLLOW-UP
After having a well-functioning allograft,the general condition and laboratory findings improved.Immunosuppressive drugs,including corticosteroids,tacrolimus and mycophenolate,were used.Three weeks after surgery,hemodialysis was stopped because of improving renal function.Two months later,the serum creatinine level was 1.5 mg/dL,and the spot urine protein/creatinine ratio was 193.3 mg/g.
DISCUSSION
IgAN associated with chronic liver disease is the most prevalent pattern of secondary IgAN.Mesangial IgA deposition is frequently found in autopsy specimens in the general population without medical illness[5].IgAN has been found in 25% of kidney biopsy specimens from 60 patients with end-stage liver disease[6].Serum IgA levels are frequently elevated in patients with alcoholic liver cirrhosis.In anex-vivostudy,peripheral blood mononuclear cells of alcoholic liver cirrhosis patients secreted more IgA than those of healthy controls[7].The accumulation of IgA is thought to result from decreased clearance of IgA,which can be explained in two ways.As cirrhosis progresses,the number of hepatocytes and Kupffer cells,which express the asialoglycoprotein receptor and Fc receptors that bind galactose residues of IgA and remove it from circulation,also decreases[8,9].Portal hypertension may play a role in hyperimmunoglobulinemia because of the portal venous flow directly from the portal vein to the systemic circulation.Our patient had no clinical evidence of portal hypertension before fulminant hepatic failure,though she did have a portosystemic shunt on CT scan at the time of diagnosis of IgAN.A portosystemic shunt is a communication between the portal vein and the systemic vein,and it is caused by a congenital malformation,liver cirrhosis or trauma.Portosystemic shunts can be found incidentally in the absence of other signs of portal hypertension[10,11].
Secondary IgAN associated with autoimmune disorders,including Sjogren’s disease,ankylosing spondylitis and coeliac disease,has been reported in the literature[2,12,13].However,IgAN with AIH has been reported in only a limited number of patients,and most of them had other autoimmune diseases such as Sjogren’s disease which is often reported to be associated with IgAN[14,15].In our case,two different diseases that do not share a common pathogenesis were diagnosed sequentially.AIH is a chronic inflammatory liver disease and that may progress to liver cirrhosis or fulminant hepatitis[4].The pathogenesis of AIH is not fully understood.The destruction of self-tolerance to hepatocyte antigen may play a key role in the pathogenesis of AIH.Autoimmune liver injury is characterized by autoreactive CD4 and CD8 T cells via cellular immune mechanisms.Currently,regulatory T cells that suppress excessive immune reactions are considered important mediator cells in the immunopathology of AIH[16].
Since there are a limited number of cases,the renal outcome of patients with secondary IgAN receiving liver transplantation is not clear.A retrograde observational study suggested that kidney function tends to be relatively favorable after liver transplantation.Among 7 patients who underwent liver transplantation,only one progressed to end-stage kidney disease during the 5 years follow-up period[17].In this report,liver transplantation did not affect the disease progression of IgAN.
There is neither a clear definition of secondary IgAN,which is recognized when IgAN coexists with other conditions,nor a histopathological feature to distinguish primary IgAN from secondary IgAN[18].Moreover,reported cases of IgAN concurrentwith AIH are sparse,and the pathophysiological relationship between the two diseases has not been well established.In our patient,the clinical activity of IgAN did not correlate with the acute onset of AIH,which indicates that the possibility of the coexistence of primary IgAN with AIH cannot be excluded.Therefore,the analysis of additional cases is required in the future.Additional case reports are necessary to promote studies on the relevance of IgAN and AIH.
CONCLUSION
We report a rare case of IgAN associated with AIH presenting as fulminant hepatic failure treated with liver transplantation.Both diseases were diagnosed simultaneously,even though they were thought to have different pathogeneses.Whether the secondary IgAN was related to AIH or the two diseases coincidentally occurred remains uncertain.Further case reports and analyses of IgAN concurrent with other diseases,which is known to be rare,are needed to determine potential pathophysiological relationships.
猜你喜欢
杂志排行
World Journal of Clinical Cases的其它文章
- Diagnosis and treatment of an elderly patient with 2019-nCoV pneumonia and acute exacerbation of chronic obstructive pulmonary disease in Gansu Province:A case report
- Active surveillance in metastatic pancreatic neuroendocrine tumors:A 20-year single-institutional experience
- Shear wave elastography may be sensitive and more precise than transient elastography in predicting significant fibrosis
- Diagnosis and treatment of mixed infection of hepatic cystic and alveolar echinococcosis:Four case reports
- Surgical strategy used in multilevel cervical disc replacement and cervical hybrid surgery:Four case reports
- Gallbladder sarcomatoid carcinoma:Seven case reports