Acute esophageal obstruction caused by reverse migration of gastric bezoars:A case report
2020-09-14
Fu-Hua Zhang,Yong-Ning Zhou,Department of Gastroenterology,The First Hospital of Lanzhou University,Lanzhou 730000,Gansu Province,China
Fu-Hua Zhang,Yong-Ning Zhou,Key Laboratory for Gastrointestinal Diseases,The First Hospital of Lanzhou University,Lanzhou 730000,Gansu Province,China
Fu-Hua Zhang,Xiang-Ping Ding,Jin-Hua Zhang,Lian-Sheng Miao,Ling-Yu Bai,Department of Gastroenterology,Affiliated Hospital of Northwest Minzu University,Lanzhou 730000,Gansu Province,China
Hai-Lan Ge,Department of Radiology,Affiliated Hospital of Northwest Minzu University,Lanzhou 730000,Gansu Province,China
Abstract
BACKGROUND
Bezoars can be found anywhere in the gastrointestinal tract.Esophageal bezoars are rare.Esophageal bezoars are classified as either primary or secondary.It is rarely reported that secondary esophageal bezoars caused by reverse migration from the stomach lead to acute esophageal obstruction.Guidelines recommend urgent upper endoscopy (within 24 h) for these impactions without complete esophageal obstruction and emergency endoscopy (within 6 h) for those with complete esophageal obstruction.Gastroscopy is regarded as the mainstay for the diagnosis and treatment of esophageal bezoars.
CASE SUMMARY
A 59-year-old man was hospitalized due to nausea,vomiting and diarrhea for 2 d and sudden retrosternal pain and dysphagia for 10 h.He had a history of type 2 diabetes mellitus for 9 years.Computed tomography revealed dilated lower esophagus,thickening of the esophageal wall,a mass-like lesion with a flocculent high-density shadow and gas bubbles in the esophageal lumen.On gastroscopy,immovable brown bezoars were found in the lower esophagus,which led to esophageal obstruction.Endoscopic fragmentation was successful,and there were no complications.The symptoms of retrosternal pain and dysphagia disappeared after treatment.Mucosal superficial ulcers were observed in the lower esophagus.Multiple biopsy specimens from the lower esophagus revealed nonspecific findings.The patient remained asymptomatic,and follow-up gastroscopy 1 wk after endoscopic fragmentation showed no evidence of bezoars in the esophagus or the stomach.
CONCLUSION
Acute esophageal obstruction caused by bezoars reversed migration from the stomach is rare.Endoscopic fragmentation is safe,effective and minimally invasive and should be considered as the first-line therapeutic modality.
Key words:Esophageal bezoars;Esophageal obstruction;Acute;Endoscopic fragmentation;Case report
INTRODUCTION
Esophageal obstruction is often caused by tumors,severe inflammation,cysts and malformations,which manifests as slow and progressive clinical symptoms.Acute esophageal obstruction is frequently caused by food impaction or other foreign bodies eaten by mistake and are rarely caused by retrograde migration of secondary foreign bodies from stomach[1].Bezoars are commonly seen in the stomach but can be found anywhere in the gastrointestinal tract.Compared with gastric bezoars,esophageal bezoars are more likely to cause symptoms of gastrointestinal obstruction[2,3].The reverse migration of gastric bezoars to the esophagus leading to acute obstruction is rare with only a few reports in the literature[4,5].Here we report a case of acute esophageal obstruction caused by the reverse migration of gastric bezoars after an episode of retching,and we review the literature on esophageal bezoars.
CASE PRESENTATION
Chief complaints
A 59-year-old man presented to our hospital complaining of nausea,vomiting and diarrhea for 2 d and both retrosternal pain and dysphagia for 10 h.
History of present illness
The patient developed nausea and vomiting after eating overnight food 2 d previously with vomiting and retching more than 10 times/d.Vomitus consisted of intragastric mucus accompanied by intermittent abdominal pain and diarrhea with yellow watery stool approximately 10 times/d.The patient received a proton pump inhibitor and intravenous fluid rehydration in the outpatient clinic.His symptoms of diarrhea were relieved,but there was still nausea.The patient developed sudden retrosternal pain,dysphagia and salivation 10 h previously after severe retching.His symptoms persisted,and he was admitted to the Department of Digestive Internal Medicine in our hospital.
History of past illness
The patient had a history of type 2 diabetes mellitus for 9 years and was treated with an injection of NovoMix30;however,his blood glucose was poorly controlled.He liked to eat persimmon.He had no history of gastric surgery.
Personal and family history
The patient had no pertinent family history.
Physical examination upon admission
The patient’s vital signs were stable.He had epigastric tenderness and excessive salivation.
Laboratory examinations
Blood analysis revealed normal white blood cell count,elevated neutrophils(90.0%),and normal hematocrit and platelet count.Serum C-reactive protein was increased at 22.0 mg/dL (normal range <0.83 mg/dL).The plasma levels of myocardial enzyme were normal.Other blood biochemistries were normal with the exception of fasting blood glucose,which was 7.82 mmol/L (normal range 3.2-6.2 mmol/L).Electrocardiogram was also normal.
Imaging examinations
Computed tomography (CT) scan revealed dilated lower esophagus,thickening of the esophageal wall,a mass-like lesion with a flocculent high-density shadow and gas bubbles in the esophageal lumen (5 cm long and 4.2 cm in diameter).The CT value was 106-53 HU (Figure 1A and B).
Further diagnostic work-up
The patient underwent upper gastrointestinal endoscopy,which showed large immovable brown bezoars in the lower esophagus,which led to esophageal obstruction (Figure 2A).The endoscope was unable to pass the bezoars to enter the stomach.The patient was treated with endoscopic fragmentation,and multiple mucosal edema,erosions and superficial ulcers were observed in the lower esophagus during the treatment (Figure 2B).Multiple biopsy specimens were obtained from these sites,and examination of these specimens revealed nonspecific findings.
FINAL DIAGNOSIS
The final diagnosis was secondary esophageal bezoars.
TREATMENT
Despite difficulties,we attempted endoscopic esophageal bezoar fragmentation.After installing a hard transparent cap on the head of the endoscope,the bezoars were endoscopically fragmented using a mouse-tooth clamp and snare.The esophageal bezoars were fragmented step by step,and then fragments were removed using a basket.When the bezoars could move freely in the esophagus,they were pushed into the stomach.The bezoars were fragmented again and removed using a basket(Figure 2C).Some small fragments remained in the stomach.Coca-Cola was given to the patient in an attempt to dissolve the remaining bezoar fragments in the stomach and to prevent formation of large bezoars again[6].
OUTCOME AND FOLLOW-UP
Following endoscopic fragmentation,retrosternal pain and dysphagia disappeared.The patient had no obvious symptoms of small intestinal obstruction such as abdominal distension and abdominal pain.Follow-up endoscopy 1 wk later,showed no evidence of foreign bodies in the esophagus or the stomach.The patient was advised not to eat persimmons and control his blood sugar.
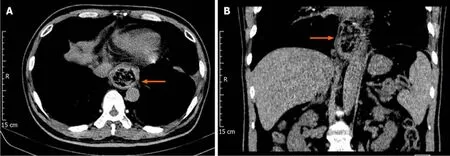
Figure1 Computed tomography findings.

Figure2 Gastroscope images.
DISCUSSION
Bezoars,which are accumulations of foreign material in the gastrointestinal tract,can be divided according to their composition into four types:Phytobezoar,trichobezoar,pharmacobezoar and lactobezoar.Phytobezoar is the most common type[7].Phytobezoars are composed of indigestible fibers (cellulose,hemicellulose,tannin and lignin) from vegetables and fruits[8].
Bezoars are more commonly seen in the stomach,and esophageal bezoars are a rare but distinct clinical entity.Under normal circumstances,with esophageal selfclearance mechanisms,such as esophageal peristalsis,saliva,and erect posture,food passes through the esophagus quickly and does not usually remain in the esophagus.This prevents the formation of bezoars.Esophageal bezoars are classified as either primary or secondary.Primary esophageal bezoars are mainly found in patients with structural or functional abnormalities of the esophagus,including achalasia,progressive systemic sclerosis,diffuse esophageal spasm,myasthenia gravis and Guillain Barre syndrome[9],especially if they are accompanied by critical illnesses that require nasal feeding or patients with mental disorders[5,10,11].Secondary bezoars originate in the stomach and are regurgitated into the esophagus when severe nausea or retching occur and become lodged in the esophagus causing acute esophageal obstruction[4],which was the most likely cause in our patient.
Before developing sudden retrosternal pain and dysphagia,our patient had no difficulty in swallowing with only occasional slight bloating.Due to his long history of diabetes,he usually eats vegetables and low-sugar fruits in order to control his blood sugar,and he especially likes to eat persimmons,which may have been the major risk factor for the formation of bezoars in this patient.Persimmon,a fleshy fibrous fruit,and dried persimmon are consumed more frequently in the north of China.The watersoluble tannin shibutol (a phlobotannin) is produced by certain cells in the skin of the persimmon and is composed of phloroglucin and gallic acid,which can generate phytobezoars especially in an empty stomach[12].
Diabetes mellitus was reported to be a predisposing factor in phytobezoar formation due to delayed gastric emptying[13].Up to 50% of patients with diabetes mellitus have delayed gastric emptying and associated gastropathy[13].Indigestible cellulose,such as the skin and seeds of fruits and vegetables may remain longer and easily form bezoars in the acidic environment of the stomach.
CT scanning and gastroscopy may be used as the main methods in diagnostic workup.CT is a reliable and accurate method for diagnosing gastrointestinal bezoars and exhibits characteristic images[14].Gastroscopy is the main tool for the confirmation of the presence and location of bezoars.The treatment options for upper gastrointestinal bezoars include endoscopic fragmentation,dissolution therapy,surgical exploration and removal of the bezoars[5].Various chemical compounds have been used to dissolve bezoars including carbonated drinks,acetylcysteine and enzymatic compounds such as pancreatic enzyme[15,16].However,this non-invasive treatment option does not seem to be appropriate for esophageal bezoars,presenting as a case of acute obstruction,such as in our patient.Surgical treatment can completely remove bezoars and relieve the obstruction;however,surgery is associated with a high risk of trauma,patients recover slowly and it is only recommended in complicated cases that cannot be resolved endoscopically or after unsuccessful attempts at endoscopic recovery[17].Thus,upper gastrointestinal endoscopy is regarded as the mainstay for the treatment of esophageal bezoars as it is safe,highly efficacious and minimally invasive[5].Although endoscopic treatment of bezoars is safe,complications may occur,and the incidence of complications is increased due to the relative pressure in the narrow esophageal space.To obtain an optimal effect,the choice of a specific treatment method depends on the morphologic characteristics of the bezoar as well as the patient’s clinical condition.Based on our patient’s medical history,symptoms and examination results,endoscopic fragmentation was performed cautiously.Mouse-tooth clamp,polypectomy snares and a basket were used to fragment and evacuate the bezoars.The endoscopic fragmentation was successful with no complications.No other lesions in the esophagus were found on esophageal biopsy and follow-up endoscopy.
Acute secondary esophageal bezoars like this case occur suddenly,together with obvious painful symptoms and requires diagnosis and treatment as soon as possible.Current guidelines recommend urgent upper endoscopy (within 24 h) for food impactions without complete esophageal obstruction and emergency endoscopy(within 6 h) for those with complete esophageal obstruction[17,18].This patient underwent endoscopic fragmentation immediately after definite diagnosis,which relieved the patient’s pain and avoided further esophageal injury.
CONCLUSION
Acute esophageal obstruction caused by bezoars reversed migration from the stomach is rare.Secondary esophageal bezoars cause acute esophageal obstruction and should be suspected when patients present with sudden retrosternal pain,dysphagia and salivation after retching.Patients with this condition require urgent treatment,and endoscopic therapy should be the first-line therapeutic modality.
杂志排行
World Journal of Clinical Cases的其它文章
- Effect of chidamide on treating hepatosplenic T-cell lymphoma:A case report
- Dental focal infection-induced ventricular and spinal canal empyema:A case report
- Multiple recurrent cystic echinococcosis with abdominal aortic involvement:A case report
- Intra-abdominal inflammatory pseudotumor-like follicular dendritic cell sarcoma associated with paraneoplastic pemphigus:A case report and review of the literature
- Mucoepidermoid carcinoma in the infratemporal fossa:A case report
- Pulmonary benign metastasizing leiomyoma:A case report and review of the literature