Risk factors for parastomal hernia in patients with colostomy:a scope overview
2020-08-27LyuChengWenJiaoLiHanWangYunNingChangDeJin
Lyu Cheng,Wen-Jiao Li,Han Wang,Yun Ning,Chang-De Jin
1 Graduate College,Tianjin University of Traditional Chinese Medicine,Tianjin 301608,China.2 School of Nursing,Tianjin University of Traditional Chinese Medicine,Tianjin 301608,China.
Abstract Objective:To investigate the risk factors of parastomal hernia in patients with a colostomy. Methods:The related studies published in Embase,PubMed,CNKI,and other databases were searched.The search time limit was from the establishment of the database to March 2020.After the literature screening,data extraction and cross-checking were carried out independently by two researchers,the qualitative research method was used to summarize.Results:After screening,6 articles were included.The results of qualitative analysis showed that a total of 10 risk factors of parastomal hernia were concluded which could be classified into personal and colostomy factors.Conclusion:The current evidence showed that 10 risk factors such as age,Body Mass Index and colostomy were related to the occurrence of parastomal hernia in patients with a colostomy.Limited by the type and quantity of research,the above conclusions need to be verified by more high-quality research.
Keywords:Colostomy,Parastomal hernia,Risk-factors,Scope review
Background
Colorectal cancer is one of the most common malignant tumors of the digestive tract and ranks third in the global ranking of malignant tumors[1].In China,the morbidity and mortality of colorectal cancer ranks fifth among malignant tumors,and shows an upward trend year by year [2].A permanent colostomy is one of the most commonly used surgical methods for colorectal cancer [3].Therefore,most patients with colorectal cancer have enterostomy.Colostomy patients in developed countries account for 1% of the population [4].The number of new colostomy patients in China is about 100000 every year,which is now more than 1 million,and there is still an increasing trend[5].Parastomal hernia is a common complication after colostomy,with an incidence of up to 30%,50%,[6,7].The incidence of colostomy hernia is as high as 48% [7].Parastomal hernia has a high incidence and recurrence rate [8].Once the occurrence of para-colostomy hernia in patients with a colostomy will bring skin ulceration,intestinal obstruction and other problems,which will affect their quality of life,and in serious cases,the life safety of patients will be affected [9].Therefore,it was important to prevent parastomal hernia.This article systematically reviewed the risk factors of patients with parastomal hernia in order to provide a reference for clinical health education to prevent parastomal hernia.
Materials and methods
Inclusion and exclusion criteria
Inclusion criteria.(1) Case-control study on the risk factors of parastomal hernia;(2) patients with parastomal hernia diagnosed by the diagnostic criteria for parastomal hernia recommended by the European Hernia Society in 2013,B-ultrasound or CT examination revealed that the contents of the abdominal cavity were protruded to the side of the stoma to extra-abdominal or found a defect in the abdominal wall next to the stoma [10];(3) whether or not a parastomal hernia occurs as an ending event;(4)the language was limited to Chinese and English.
Exclusion criteria.(1) Repeated publication;(2) lack of access to full text and missing data;(3)case reports,conference papers and other documents.
Searching strategies
Embase,PubMed,Cochrane Library,CNKI,VIP,CBM,Wanfang Databases were searched.The search time limit was from the establishment of the database to March 2020.The search adopted the combination of subject words and free words,and the search words included:parastomal hernia,peristomal hernia,influencing factors,risk factors,related factors,case-control and so on.The retrieval languages were limited to Chinese and English.Taking PubMed database as an example,the search strategy was listed in Table 1.At the same time,manual retrieval and traceability of relevant references were used to ensure the comprehensiveness of the retrieval.
Literature screening and data extraction
Literature retrieval,screening and data extraction are independently completed and cross-checked by two researchers when the two results are inconsistent,a third party will make a ruling to ensure the scientific rigor of the research process.The contents of data extraction include:author,year of publication,research country,fund funding,research type,sample size,risk factors and so on.
Methodological quality assessment
The Newcastle-Ottawa Scale (NOS) recommended by the Agency for Healthcare Research and Quality(AHRQ)was used to evaluate the inclusion study[11].The scale consists of 3 sections and 8 items,including the selection of the study population (4 items),comparability (1 item) and the measurement of exposure factors(3 items).The total score of NOS was 9,with a score of 7-9 for high-quality research,4-6 for medium-quality research and 0-3 for low-quality research.Each included literature was independently evaluated and cross-checked by two researchers,and when there was a disagreement,it was decided by the third party.
Analytical method
This study used the method of qualitative analysis to systematically summarize and analyze the basic characteristics and research results were included in the literature.
Results
Study selection
515 articles were obtained by preliminary search,and 398 articles were obtained after duplication was removed by EndNote X9 software.Topics and abstracts were screened strictly according to the inclusion and exclusion criteria,and 15 articles were included in the preliminary screening.After reading the full text,deleted 9 articles (no parastomal hernia for 1 article,non-case control study for 6 articles,incomplete data for 2 articles).6 articles that meet the requirements were finally included.As shown in Figure 1.
Inclusion of literature characteristics and quality evaluation
A total of 583 subjects were included in the study,including 148 in the case group and 435 in the control group.The research data mainly came from three countries:China,Japan and Belgium.All the included studies were case-control studies.NOS scale was used to evaluate the quality of population selection,comparability and the measurement of exposure factors.A total of 3 articles [12-14]were high-quality studies and 3 [15-17]were medium-quality studies.The methodological quality evaluation and evidence classification results of the included literature in the study were shown in Table 2.
Risk factors in patients with para-colostomy hernia
After summarized the included researches,a total of 10 risk factors of parastomal hernia were concluded which could be classified into personal and colostomy (Table 3).
Personal factors
The Personal factors related to colostomy include age,Body Mass Index (BMI),abdominal circumference,subcutaneous fat thickness and increased abdominal pressure.2 studies [14,15]show that age was related to the occurrence of parastomal hernia (odds ratio(OR):1.403-11.643).Parastomal hernia was more likely to occur in elderly patients,especially in patients older than 60 years old [15](OR=1.043).It may be related to the further decline of abdominal wall muscle thickness and strength with age[19].
Five studies [12,14-17]had shown that BMI was associated with the risk factors of parastomal hernia(OR/risk ratio (RR):0.39-7).As Asians and Europeans and Americans belong to different races,the criteria for the classification of BMI were also different.In Japan,the Japan Society for the Study of Obesity criteria defined a BMI of 25 kg/m2as being obese [12].Kojima’s study [12]suggested that BMI ≥25 kg/m2was an independent risk factor for a parastomal hernia.In China,people with BMI ≥ 25 kg/m2were overweight.The results of Zhu’s study [15]showed that overweight and obese patients with BMI ≥25 kg/m2were more likely to develop a parastomal hernia.Wu’s study [16]suggested that parastomal hernias were more likely to occur when BMI ≥26 kg/m2.Regardless of the criteria,when the patient was overweight or obese,the risk of developing adjacent to the colostomy increases.Most of the overweight and obese patients were abdominal obesity,the thickness of abdominal subcutaneous fat was increased,the abdominal muscle was weak,the abdominal pressure was increased,and the abdominal contents were easy to protrude outward through the abdominal defect.
The study of Jan [17]showed that when the waist circumference was larger than 100 cm,there was a 75% chance of developing parastomal hernia in colostomy patients.The cause may be related to abdominal obesity,so we should actively control the waistline of colostomy patients and accept lifestyle health guidance.
The study of Zhu [15]confirmed that the thickness of abdominal subcutaneous fat was related to the peristomal hernia (OR=1.061).The waistline was considered to be an indicator of abdominal obesity.The study of Kanehisa et al.[20]suggested that abdominal subcutaneous fat was a better indicator of abdominal obesity than waist circumference.Therefore,Zhu’s study [15]included a new index of abdominal subcutaneous fat thickness.BMI,waist circumference and abdominal subcutaneous fat was all related to abdominal obesity,which also suggests that colostomy patients should pay attention to their own obesity and do a good job in the prevention of parastomal hernia.
The results of Wu [16]showed that increased abdominal pressure was one of the risk factors for the occurrence of parastomal hernia (RR=8.88).Parastomal hernias were more likely to occur in patients with ostomy with higher abdominal pressure.Increased abdominal pressure was often closely related to constipation and long-term cough.Therefore,medical staff should actively eliminate constipation,cough and other symptoms of ostomy patients.Before ostomy surgery,medical staff should do condition assessment.After surgery,medical staff should actively deal with complications and treat chronic diseases in order to achieve the purpose of controlling abdominal pressure.Not only medical personnel should pay more attention to abdominal pressure,patients and their families should also actively learn related health information,and strengthen the importance of parastomal hernia.
Factors related to colostomy
The factors related to colostomy include the way of colostomy,the location of colostomy,the mode of operation,the size of colostomy and the location of colostomy before the operation.
Three studies [13-15]had shown that there was a correlation between the approach of colostomy and parastomal hernia (OR:3.964-15.156).There were two ways of colostomy:extraperitoneal colostomy and peritoneal colostomy.Extraperitoneal colostomy was first proposed by Amussant [21].Many studies had confirmed that the incidence of parastomal hernia inpatients with an extraperitoneal stoma was lower than that in patients with an extraperitoneal stoma.The extraperitoneal colostomy made the enter-ostomy tube pull out of the abdominal wall through the extraperitoneal tunnel,which was completely covered by a layer of peritoneum,which eliminated the para-colonic sulcus and eliminated the potential danger of small intestinal entrapment.On the one hand,it effectively strengthened the fixation of the intestinal fistula,avoided the excessive dissociation of the proximal intestinal segment of the intraperitoneal stoma,and on the other hand,reduced the direct effect of intraperitoneal pressure on the colostomy.Therefore,the incidence of colostomy complications was low[22].
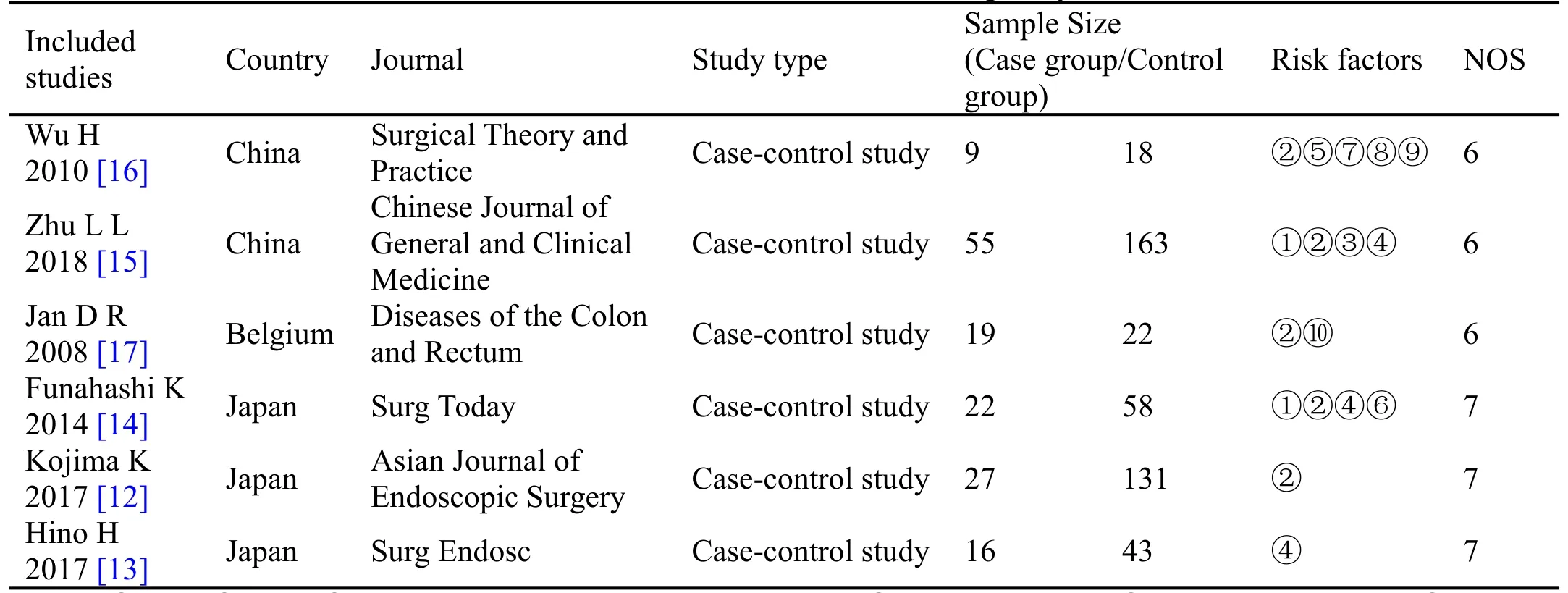
Table 2 Basic characteristics of researches and quality assessment
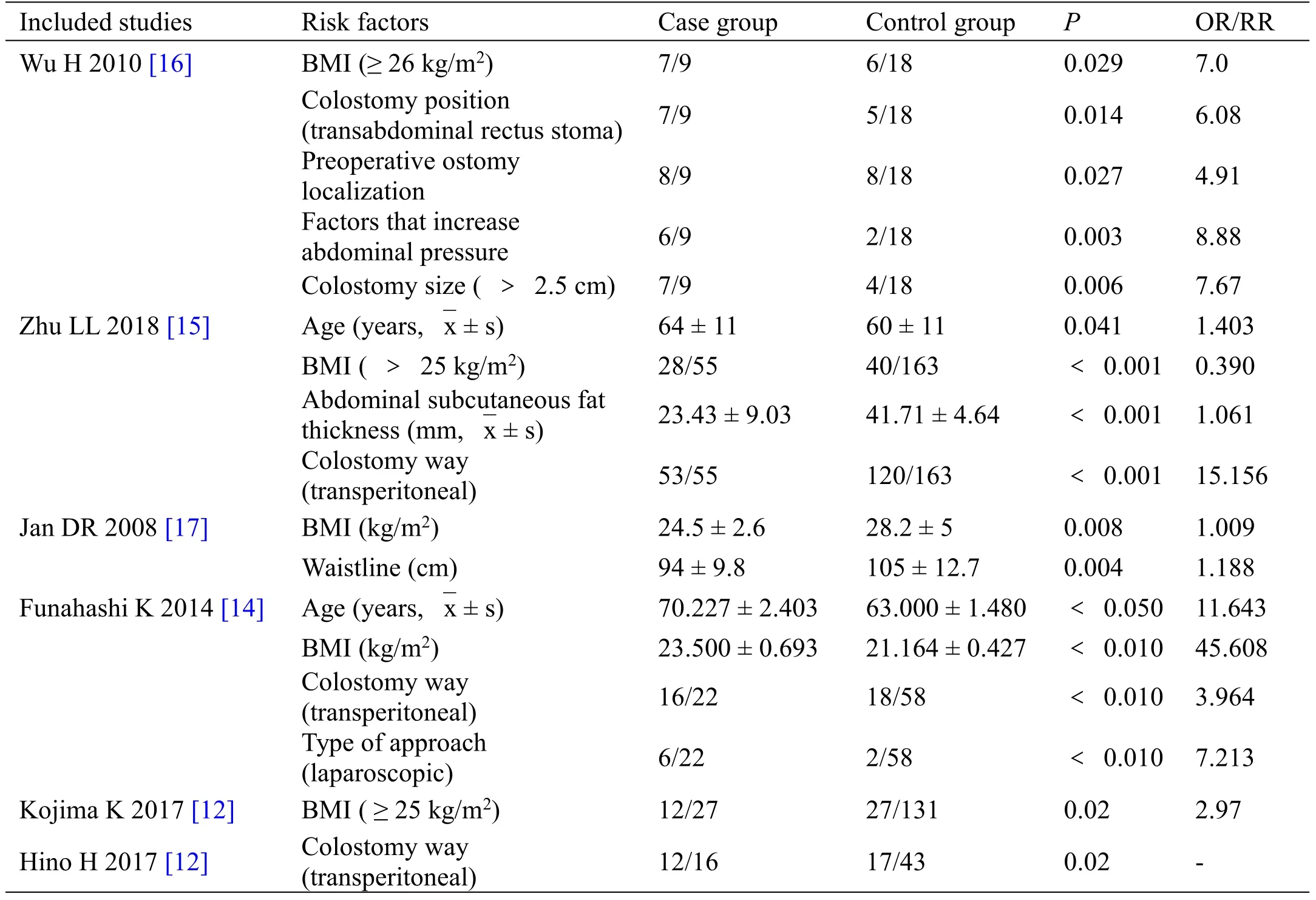
Table 3 The related risk factors from included researches
One study [16]showed that the location of a stoma was also related to the parastomal hernia (RR=6.08).The position of colostomy can be divided into rectus abdominis and para-rectus abdomen ostomy.Rectus abdominis muscle and its deep abdominal medial,external oblique muscle and abdominal transverse muscle constituted the ventral anterolateral muscle group.Rectus abdominis muscle can protect abdominal organs and maintain the stability of organs.Transrectus abdominis ostomy can significantly reduce the incidence of parastomal hernia.The abdominal wall on the side of the rectus abdominis was weaker than the medial,where the complications of the stoma were significantly increased.
One study [14]showed that different surgical methods can affect the occurrence of parastomal hernia(OR=7.213).There were two surgical methods:laparoscopy and laparotomy.Although Funahashi’s study [14]had shown that laparoscopic surgery was more likely to develop parastomal hernia than laparotomy,many recent studies on laparoscopic versus open randomized controlled trials (RCTs) for colorectal cancer had shown that laparoscopic colostomy was superior to laparotomy in terms of colostomy complications[23-25].Therefore,the mode of operation as a risk factor needed to be further confirmed by more high-quality evidence.
One study [16]showed that parastomal hernia was easily induced when the diameter of stoma was larger than 2.5 cm(RR=7.67).The size of stoma was related to the size of parastomal hernia.According to the observation of Zhu et al.[15],the diameter of skin incision of colostomy was generally 2 cm.After the operation,due to skin contraction,the diameter of colostomy will be enlarged by 0.5 cm,and then reach the appropriate size of 2.5 cm.
One study [16]showed that the location of preoperative colostomy was related to the occurrence of parastomal hernia (RR=4.91).Patients with preoperative localization were less likely to have parastomal hernia than patients without location.The preoperative colostomy location was that the colostomy therapist choose a suitable colostomy position in the patient’s abdomen one day before the operation,combined with the patient’s physical condition and living habits.When positioning,you will try to avoid uneven,wrinkled skin and scars.Therefore,the location of preoperative colostomy was more reasonable and efficient.
Discussion
This article summarized a total of 10 risk factors for parastomal hernia,which are divided into two aspects:patient and stoma.From the perspective of the patient,when the patient is older than 60 years old,attention should be paid to the prevention of parastomal hernia.For obese patients,weight loss should be encouraged,and BMI and waist size should be controlled to achieve the purpose of prevention.For patients with long-term constipation and cough,active and targeted measures should be given to avoid increased abdominal pressure.From the perspective of ostomy,on the one hand,the medical staff should choose the appropriate ostomy position before surgery,and actively do the pre-operative positioning of the ostomy.On the other hand,they should pay attention to factors such as the ostomy route,surgical method,and the size of the ostomy.Medical staff should try to choose the best plan to prevent parastomal hernia.Medical staff should strengthen the protection of high-risk patients with the above risk factors to reduce the incidence of parastomal hernia and improve the clinical outcome of patients.
Based on current evidence,this article found 10 risk factors for parastomal hernia:age,BMI,abdominal subcutaneous fat thickness,colostomy way,colostomy position,type of approach,preoperative ostomy localization,factors that increase abdominal pressure,colostomy size,waistline.Clinical nurses should pay enough attention to patients with ostomy,strengthen the identification of risk factors and screening for parastomal hernia,carry out early health education and intervention measures,and prevent its progress into parastomal hernia.Similarly,ostomy patients and their families should also strengthen the control of risk factors,such as controlling BMI through weight control.
This study was carried out in strict accordance with the process of the systematic review,the quality of this study was good,and came from three different countries,which had certain reference value for clinical practice.However,because the included studies were all case-control studies,the number of included studies was small and the data can’t be analyzed by meta-analysis,so it will affect the accuracy to a certain extent.Therefore,the research results of this paper had certain limitations.A more rigorous RCT was necessary.It was recommended to conduct high-quality large-sample multi-center studies in the future to further explore the risk factors for parastomal hernia.
杂志排行
Clinical Research Communications的其它文章
- Screening and bioinformatics analysis of thyroid cancer-related hub genes
- Clinical observation of 36 patients with chronic nephritis proteinuria treated with Zhuangshen Gujing decoction
- Bibliometric analysis of nursing studies on Corona Virus Disease 2019 in China
- Influence of overweight in pregnancy on the intestinal flora as well as maternal and infant outcome