Outcomes in obese patients undergoing direct anterior hip replacement: a nonrandomized study
2020-08-03SophiaStasiDimitriosTzefronisGeorgePapathanasiouMichailSarantisGeorgeMacheras
Sophia Stasi , Dimitrios Tzefronis, George Papathanasiou Michail Sarantis, George A. Macheras
1 Laboratory of Neuromuscular and Cardiovascular Study of Motion, Physiotherapy Department, Faculty of Health and Care Sciences, University of West Attica, Attica, Greece
2 4th Orthopaedic Department, “KAT” General Hospital of Attica, Athens, Greece
Abstract
Key words: total hip arthroplasty; obesity; functionality; quality-of-life; Timed Up & Go test; modified Harris Hip Score; 12-item International Hip Outcome Tool
INTRODUCTION
Obesity and osteoarthritis (OA) are two interconnected worldwide health care problems that are highly prevalent among the adult population.1Obesity—defined as body mass index (BMI) ≥ 30 kg/m2—is a well-recognized global epidemic. According to data from the World Health Organization, the obesity epidemic affected 11% of men and 15% of women globally in 2014, representing more than half a billion adults and nearly twice as many as in 1980.2Obesity increases the risk of many chronic diseases, including OA. Weight-bearing joints (e.g. hip, knee) are often involved in the OA process, because of the greater mechanical forces exerted on the joints as a result of obesity. In an aging and heavier population, OA has become one of the leading causes of disability, as it places a major burden on the musculoskeletal system.3,4
BMI has a significant positive association with hip OA. A 5-unit increase in BMI was related to an increased risk of hip OA (relative risk [RR]: 1.11; 95% confidence interval [CI]: 1.07-1.16) in both women and men.5Several studies have examined the relationship between BMI and the risk for total hip arthroplasty (THA). Data from a prospective cohort study indicated that increasing BMI was associated with an increased relative risk for THA (RR: 2.47) when the obese group was compared to those with the lowest BMI.6In another large population-based prospective cohort study, BMI was significantly associated with the incidence of THA (RR: 2.6), with a continuous dose-response relationship between BMI and arthroplasty risk.7
In recent years, there has been growing interest in the minimally invasive surgical techniques that are used for the performance of THA. The advantages of these techniques include less soft tissue trauma, a smaller amount of blood loss, less postoperative pain, shorter hospital stay, better esthetic appearance of the incision, and faster recovery time.8,9Over the last decade, the technique of direct anterior approach-minimally invasive surgery (DAA-MIS) has generated scientific interest because of its soft-tissue-preserving nature (intramuscular and interneural technique), combined with the relatively low risk of dislocation.10
Some studies indicate that obesity is associated with a higher complication rate after THA and with poorer clinical functional outcomes.11,12Other studies have shown that obese patients do not differ from the nonobese in this respect.13-15Obese patients are a challenging cohort of patients because of their large body habitus, but the advantage of the DAA-MIS technique is that many obese patients have a relatively small amount of subcutaneous adipose tissue along the anterior aspect of the thigh, which allows for a relatively routine operative procedure.13-15
Nevertheless, the data are controversial and further studies need to be performed with comparisons between nonobese and obese patients, in relation to minimally invasive techniques such as DAA-MIS. The aim of this trial was to examine the impact of obesity in hip OA patients who underwent primary THA via DAA-MIS, with regard to postoperative pain levels, functional status and quality of life.
SUBJECTS AND METHODS
Study design
This nonrandomized study analyzed a subset of the data collected for an ongoing larger trial (Clinical Trial Identifier: ISRCTN15066737). The protocol of this study was approved by both the Ethics Committee and Scientific Research Council of the “KAT” General Hospital of Attica, Athens, Greece (ref: ΔΣ234/12-03-2019) on March 12, 2019 (Additional file 1); as it conforms to the principles stated in theDeclaration of Helsinkiand its later amendments.16The study conformed to the reporting guidelines of the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement17(Additional file 2).
Participants
Between January 2018 and January 2020, participants were recruited from hip OA patients who had been selected for surgery by the chief orthopaedic surgeon involved in the present study. During recruitment, patients are informed of the purposes of our study. The main inclusion criterion was the existence of 3 or 4 grade hip OA according to the Kellgren-Lawrence classification system.18BMI was used as a factor in the randomization process and the randomization list was formed on this basis. Specifically, participants were divided into two groups according to their BMI.19Patients with a BMI value between 20 kg/m2and 30 kg/m2were enrolled in the first group (nonobese group), while patients with a BMI value ≥ 30 kg/m2were enrolled in the second group (obese group). The patients had to meet the following inclusion criteria: age > 50 years, symptomatic hip OA, and ambulatory before surgery. Patients were excluded if they suffered from dementia, chronic respiratory disease, chronic renal failure, heart failure or a neurological disorder. After recruitment, any patient who experienced postoperative complications, such as wound healing problems, periprosthetic fracture, dislocation or pulmonary embolism, was replaced by another patient who satisfied the inclusion criteria. In addition, patients were excluded if they discontinued the postoperative physiotherapy intervention before the 6thweek’s measurements. No patient or clinician was blinded to the group allocation.
Upon acceptance, on admission day (1 day before surgery), participants written informed consent (Additional file 3), their demographic and clinical characteristics, as well as the preoperative outcomes were recorded. The two postoperative measurements (at the end of the 6thweek, and again at the end of the 12thweek) were also recorded after schedule appointments. All measurements were made by the same examiner, who was not involved in any part of the study, in the orthopaedic department’s examination room.
I ntervention
Primary THA via DAA-MIS technique using a traction table, through a single incision,20was performed in all patients and an uncemented prosthesis was used. The technique has been already described by our chief orthopaedic surgeon, in a previous publication.20It is worth noting that the benefits of DAA-MIS include the ideal soft tissue interval, the fact that the femur is more superficial than any other approach and its respect to muscles and nerves of the hip region, making it suitable for obese patients. In such patients, the key point is that the subcutaneous tissue superficial to the tensor fascia should be retracted -i.e. using a plastic soft-tissue protector- to facilitate visualization.20Physiotherapy was started on the first postoperative day and lasted 6 weeks, first on a daily inpatient basis, and then home-based after discharge (three sessions per week) until the end of the 6thweek. To protect the healing of muscles and the anterior capsule, adduction past neutral position, external rotation past 45°, hyperextension, and hip flexion past 90° should be avoided for at least 6 weeks.21In both groups, the in-hospital physiotherapy programme included ankle pumps, isometric contraction of quadriceps, heel slides, supine hip abduction/adduction (mid-range of motion), isometric contraction of gluteal muscles, transfer training, such as supine to sitting position, sit to stand, and ambulation with a walker. During the home-based physiotherapy, the previous exercises were continued and were gradually progressed in difficulty, as individual tolerated. When the patient acquires ease in changing direction during walking with assistance and is able to turn safely while walking with the assistive device, then he/she may start to train with exercises in the upright position. Briefly, the exercises from upright position included: hip flexion with extended knee, hip abduction/adduction (0°-30°), hip flexion combined with knee flexion, standing toe raises and lateral steps. The 6thweek physiotherapy’s goals were the adequate range of hip motion within the aforementioned postoperative precautions, and the sufficient muscles’ strength in order to allow patients to return to normal daily-life activities, as well as the independent or a single cane ambulation, as individual tolerated.21One physiotherapist was responsible for all participants and carried out the physiotherapy intervention both during hospitalization and at the patient’s home, being responsible for the progress according to the clinic’s protocol and confirming the patient’s adherence to it. These physiotherapy sessions ensured the participants’ optimal compliance.
Procedures
Outcome measures were obtained at three different time points: prior to surgery (baseline), postoperatively at the end of the 6thweek, and again at the end of the 12thweek. Pain levels were measured using the self-reported Face Pain Scale-Revised (FPS-R).22,23Functional ability was measured with the objective physical performance measure Timed Up & Go (TUG) test,24and with the reliable and validated Greek version of the patient-reported outcome, modified Harris Hip Score (MHHS-Gr).25Quality of life was evaluated with the reliable and validated Greek version of the patient-reported outcome, 12-item International Hip Outcome Tool (iHOT12-Gr).26
Outcome measures
FPS-R
The FPS-R is an instrument frequently used to measure pain intensity. It includes six facial expressions that cover the entire range of pain levels in a hierarchical order.22The instrument asks patients to describe their pain according to one of the six facial expressions that corresponds to their pain and enables them to translate their subjective experience of pain into a quantitative, numeric measure. The FPS-R scoring options and their meaning are: 0 (no pain), 2 (mild pain), 4 (moderate pain), 6 (severe pain), 8 (very severe pain) and 10 (worst pain possible).23
TUG test
The TUG test was used to assess participants’ functionality. This test was introduced in 1991 as a modification of the “Get Up and Go” test.24It is a simple, rapid and widely used clinical tool for the measurement of the functionality and mobility of the lower limbs.27The TUG test measures the time (in seconds) taken by a participant to stand up from an armed chair with a seat height of 46 cm, walk for 3 m, turn around a cone and return to sit on the same chair. Participants were asked to perform the test in a quick, yet safe, pace, and were allowed to use the walking aid on which they depended on at the time of measurement. The participants performed the test twice, with a 5-minute resting interval between tries. The shorter of the two performance times was recorded.
MHHS
The MHHS is a patient-reported questionnaire that includes assessments based on pain and functional limitations regarding gait and daily-life activities. One item evaluates the pain (0-44 points), while 7 items evaluate the patient’s functionality (0-47 points). The total points form a scale from 0 to 91. A multiplier of 1.1 provides a total score of 100 (best possible outcome).28
iHOT12
The iHOT12 is a quality-of-life patient-reported questionnaire that comprises 12 items. Each question has equal score-value, so that the mean of all questions amounts to the score result, ranging from 0 to 100 points. A score of 100 indicates excellent quality of life (full function and no symptoms), whereas a score of zero signifies maximum limitations and extreme symptoms.29
Statistical analysis
Data are expressed as mean ± standard deviation for continuous variables and as percentages for categorical data.
Homogeneity of demographic and clinical characteristics between groups, comparison of variables (FPS-R, TUG test, MHHS-Gr and iHOT12-Gr) between groups at each time point and percentage change of the variables from baseline were evaluated using the independent samplest-test or the Mann-WhitneyUtest in case of violation of normality. To control the type I error, the Bonferroni correction was used.
The comparison of variables during the observation period per group (baselinevs.6thweekvs.12thweek) was performed using the one-way analysis of variance model with repeated measurements. Pairwise comparisons (post hoctests) between time measurements were performed using the Bonferroni test. All tests were two-sided and statistical significance was set atP< 0.05. All analyses were carried out using the statistical package SPSS version 21.00 (IBM Corporation, Somers, NY, USA).
RESULTS
Participant baseline data
Ninety patients were assessed for eligibility. Twenty of them were excluded on the basis of the exclusion criteria and 10 were lost to follow-up. Finally, the data from 60 patients (30 per group) were analyzed. The recruitment procedure is depicted in the flow diagram in Figure 1. Regarding baseline (preoperative) measurements, homogeneity between groups for all demographic and clinical characteristics was found, except for weight (P< 0.001) and BMI (P< 0.001; Table 1).
Preoperative versus postoperative results regardless BMI
Six weeks after DAA-MIS, both obese and nonobese patients had significantly less pain (FPS-R), higher functionality (TUG test and MHSS-Gr) and better quality of life (iHOT12-Gr), compared to preoperative measurements (P< 0.001). The improvement in all overall outcomes continued, showing a further statistically significant difference in 12-week measurements (P< 0.001). The explicit absolute values and the postoperative percentage changes in FPS-R, TUG test, MHSS-Gr, and iHOT12-Gr are shown in Table 2. All the patients included in our study benefited from the DAA-MIS technique.

Figure 1: Flow diagram of the study.
Comparison between obese and nonobese groups
Analyses of the percentage changes between groups revealed no statistically significant differences between groups at the 6thweek’s measurements (Table 2). However, the nonobese group experienced less pain (FPS-R = 0.08%), shorter time (TUG test = 0.76%) and reported a better quality of life (iHOT12-Gr = 8.74%), while the obese group reported better functionality (MHSS-Gr = 21.76%) (Table 2). At the 12thpostoperative week, the nonobese group experienced even less pain (FPS-R = 5.14%), even shorter time (TUG test = 2.7%), while the obese group reported even better functional ability (MHHS-Gr = 48.45%) and a better quality of life (iHOT12-Gr = 3.35%). Despite these improvements, once again no statistically significant differences were observed between the obese and nonobese patients (Table 2), suggesting that BMI was not a factor that had influenced the outcome of DAA-MIS.
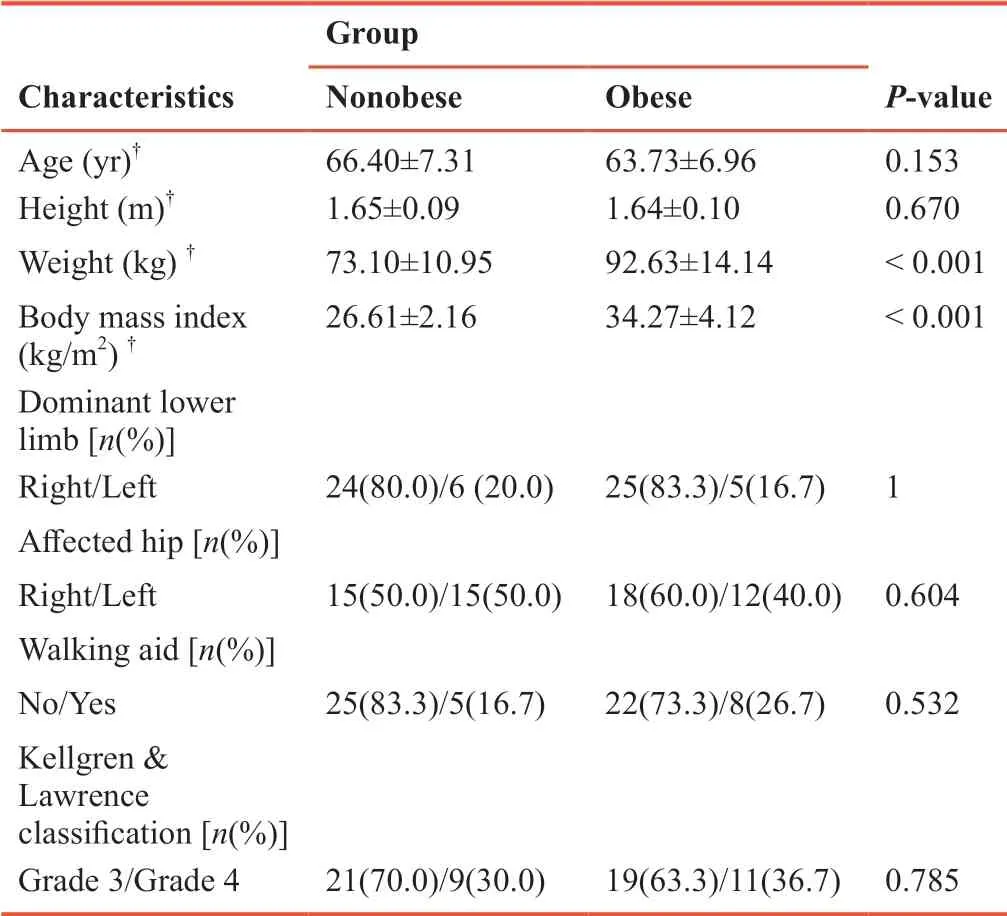
Table 1: Demographic and clinical characteristics of the study’s population
DISCUSSION
To our knowledge, this study is among the very few studies to focus on the effect of obesity on postoperative pain levels, functionality and quality of life in patients who underwent primary THA via DAA-MIS. In the present study, we found similar improvements in pain, functionality and quality of life after DAA-MIS in both obese and nonobese patients, suggesting that BMI should not be considered as a factor that will influence postoperative outcomes. Our results are in line with other studies that reported that obese patients do not differ from the nonobese in terms of postoperative outcomes.13-15
All our hip OA patients, regardless of BMI, benefited from the performance of THA via DAA-MIS. THA is universally acknowledged as one of the most successful surgical procedures for patients with hip OA, as it has the greatest potential to relieve pain, improve function and enhance the quality of life.30The latest tissue-sparing techniques of THA, which are associated with faster recovery, lower costs and better outcomes, have resulted in the rapid adoption of DAA-MIS for primary THA.31
It is worth noted that, at baseline, the obese group had a significantly lower MHHS-Gr score compared to nonobese patients, but this difference was not observed in the other outcomes. Although the difference did not reach statistical significance, postoperatively the obese group showed a greater percentage improvement in MHHS-Gr at both the 6thand 12thweeks. However, although the nonobese group reported better iHOT12-Gr scores at the 6thpostoperative week, in the 12-week measurements the percentage improvement of the obese group exceeded that of the nonobese patients; obese patients reported better quality of life. These findings could be explained in terms of how individuals view themselves in relation to disability and whether they have high or low expectations regarding their performance of daily-life activities.32Nonobese individuals might have higher expectations and so underestimated their postoperative functionality, being used to high functional levels pre-OA, which were only limited by the gradual aggravation of hip OA.33On the other hand, obese individuals, who had experienced a low level of functionality as their weight33exacerbated their OA-related disability, viewed their postoperative experience as a remarkable improvement in their functionality; thus, they may have overestimated their functional level.32This explanation of an apparently paradoxical finding is supported by the results of the TUG test, an objective physical performance measure, in which a corresponding difference was not observed. However, MHHS-Gr and iHOT12-Gr, as patient-reported outcomes, and the TUG test, as a physical performance measure, provide complementary information, and both are needed to perceive the level of disability in its entirety and its impact on quality of life; this is essential in clinical research and practice involving hip OA patients.34
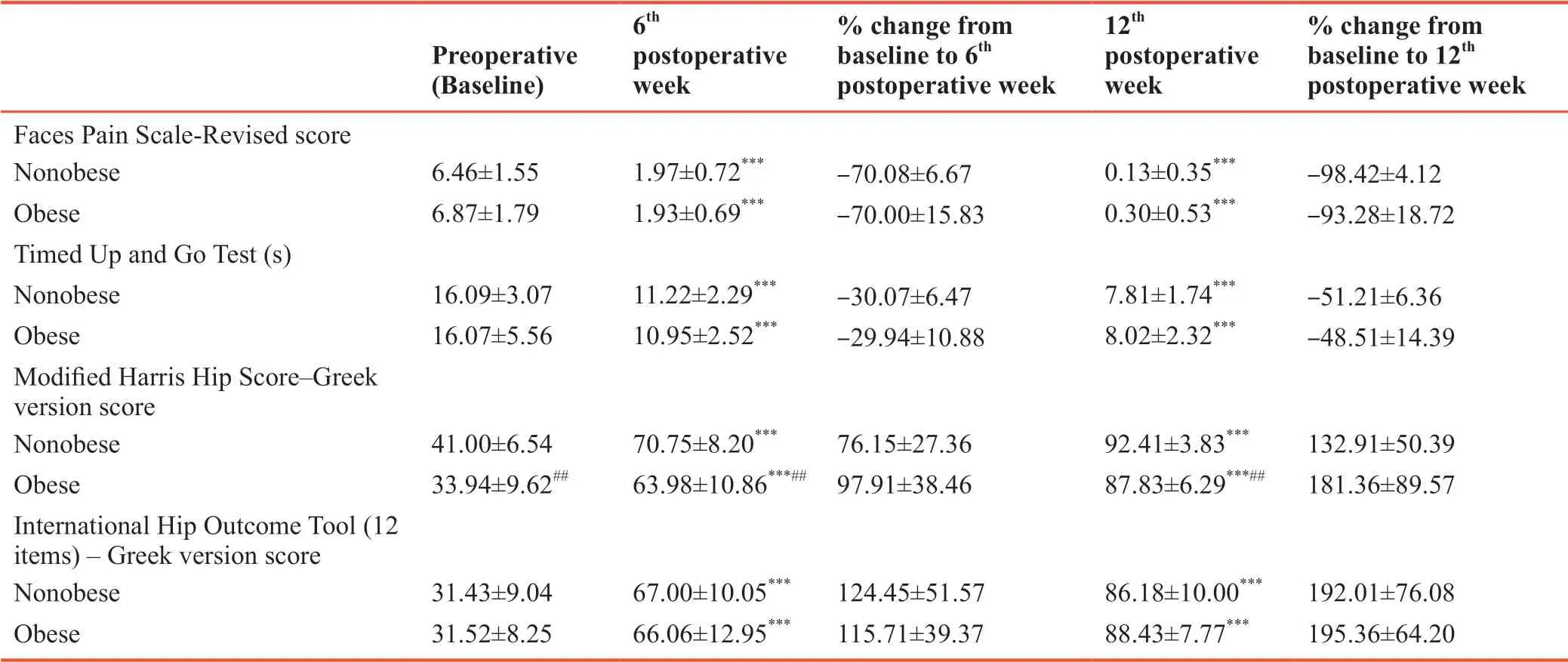
Table 2: Comparison of pain levels, functional status, and quality of life between groups at baseline and the 6th and 12th postoperative weeks
There were no incidences of wound infection in either the nonobese or the obese groups of our study, although in other studies it was reported that the postoperative wound infection rate was higher in obese patients who underwent DAA, mainly because of the overlying abdominal adipose tissue that may disturb wound healing.35,36However, these findings were similar to complication rates in the literature for other THA surgical approaches.36
Strengths and limitations
In the present two-group comparative study, all patients underwent uncemented THA via DAA-MIS performed by the chief orthopedic surgeon, and the same physiotherapist was responsible for the physiotherapy in all patients. Moreover, all measurements were made by the same examiner, who was not involved in any other part of the study. The dropout rate was very low, since the supervision and guidance from the physiotherapist during home sessions helped ensure patient adherence after discharge. These factors added strength and statistical power to the results of this study.
On the other hand, there are important limitations that must be mentioned. Patients were followed until the 12thpostoperative week; hence, it is unclear whether the observed postoperative outcomes would be maintained over time. Moreover, recording and evaluation of the impact of possible obesityrelated comorbidities on the postoperative outcomes was not included in the design of the present study.
Conclusion
In the present study, we found similar improvements in pain and functionality after THA with the DAA-MIS approach in both obese and nonobese patients, suggesting that BMI should not be considered as a factor that influences the outcome of THA via DAA-MIS. This surgical technique could therefore be a suitable approach for THA in obese patients. An understanding of the changes in pain, functional outcomes and quality of life in both obese and nonobese patients, as reported in the current study, will be helpful for both the patient and the surgeons in the decision process regarding the best THA approach. Further research is needed to verify our results regarding the impact of obesity on pain, functional and quality-of-life outcomes after DAA-MIS.
Additional files
Additional file 1: Ethical Approval Documentation (Greek).
Additional file 2: TREND checklist.
Additional file 3: Model consent form (Greek).
Acknowledgments
The authors would like to thank Dr. Antonios Galanos, Biostatistician of Laboratory for Research of the Musculoskeletal System (LRMS), Faculty of Medicine, National and Kapodistrian University of Athens, Greece for the statistical analysis of the data.
Author contributions
Study concept, guarantor: SS and GAM; study design, definition of intellectual content: SS, GP and GAM; literature search, experimental studies, data acquisition: SS, DT and MS; clinical studies: SS, DT, GP, MS; statistical analysis: GP; manuscript preparation: SS, DT; manuscript editing: SS, DT, GP, GAM. All authors conducted data analysis and manuscript review, and approved the final version of the paper.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Financial support
None.
Institutional review board statement
This study protocol was approved by both the Ethics committee the Scientific Research Council of the “KAT” General Hospital of Attica, Athens, Greece (ref: ΔΣ234/12-03-2019) on March 12, 2019, and was performed in accordance with theDeclaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement
This study followed the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement.
Biostatistics statement
The statistical methods of this study were reviewed by the biostatistician of Laboratory for Research of the Musculoskeletal System (LRMS), Faculty of Medicine, National and Kapodistrian University of Athens, Greece.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Individual participant data collected during this trial will be available after de-identification (text, tables, figures, and appendices), beginning 9 months and ending 36 months following article publication. Study Protocol and Informed Consent Form, will be available. Access will be granted to researchers who provide methodologically sound proposal, in order for them to achieve aims in the approved proposal. Proposals should be directed to Dr Sophia Stasi (soniastasi1@gmail.com). To gain access, data requestors will need to sign a data access agreement. After 36 months the data will not be applicable.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.