Mitral valve repair in infective endocarditis:which evidence?
2020-07-30
Dipartimento medicina sperimentale e clinica,Università di Firenze,Firenze 50124,Italy.
Abstract
Keywords:Infective endocarditis,valve repair,valve replacement,survival
INTRODUCTION
Epidemiology of native valve endocarditis
The epidemiology of native valve endocarditis has undergone significant changes over the past few decades.The incidence is reported between 1.5 and 5 per 100,000 persons per year,although large epidemiological studies have shown a continuous increasing trend[1-3].This is associated with a significant increase in economic costs,above $120,000 per patient[4].Both native and prosthetic valve endocarditis epidemiology are affected by the increasing number of health care-associated infections,contributing for not less than 25% of overall cases.Hemodialysis,implantable cardiac devices,venous catheters,immunosuppression,and intravenous drug use are main risk factors for infective endocarditis (IE)[5,6].Patients are older and frail,often affected by serious comorbidities.Infections due to staphylococci are continuously increasing in comparison to oral streptococci.Staphylococci at present are the most frequent etiologic organism.A Danish study showed that between 1957 and 1990,Staphylococcus aureus bacteremia increased from 3 to 20 per 100,000 person-years,paralleling the increase of hospital admissions and invasive medical procedures[7].Hand-hygiene,barrier precautions,and antisepsis are effective measures in reducing the rate of bacteremia.Microbial eradication is the goal of treatment in IE.Broad spectrum empiric antibiotic treatment should be started as soon as possible,immediately after collection of samples for blood-culture.Identification of etiologic microorganism allows tailored therapy to be administered,even if antibiotic resistance is a growing worrying phenomenon[2,8].Overview of medical management of IE is beyond the aim of present review.It must be emphasized that in patients in medical treatment,a close reassessment of clinical,laboratory and echocardiographic findings is mandatory since infective endocarditis may rapidly progress even under antibiotic treatment.Moreover,in patients without indication to urgent surgery,hemodynamic changes related to residual valve damage are associated with a decreased life expectancy.A large study conducted in France showed that surgical treatment was the only independent predictor of long-term survival in patients admitted to hospital for infective endocarditis[9].
Indications to surgery
The indications for surgery in patients with IE have been defined by American Association for Thoracic Surgery,American Heart/American College of Cardiology and European Heart Society (ESC)[10-12].According to guidelines,surgery is defined as urgent,usually within index hospitalization before completion of a full course of antibiotics.The ESC guidelines distinguish emergency surgery (within 24 h) from urgent surgery (within a few days),or elective surgery (after 1 to 2 weeks) of antibiotic therapy.More than 50% of patients with native valve endocarditis needs surgery,more frequently on an urgent basis.
Hemodynamic impairment due to severe valve regurgitation,characterized by severe left ventricular dysfunction,refractory pulmonary edema and/or cardiogenic shock,is the more frequent indication for urgent surgery (class I level of evidence B).Early surgery is also indicated in the case of extension of the infection beyond the valve annulus,with perivalvular abscess,fistula,or pseudoaneurysm formation or with involvement of heart conduction system (AV block).
In native valve endocarditis,extra valvular spreading occurs in about 30% of cases.Urgent surgery may be needed to prevent potential catastrophic embolism in the presence of large (> 10 mm) and/or mobile vegetations.A randomized study showed that in native valve endocarditis characterized by large vegetations (> 10 mm) and/or severe valve regurgitation,surgery was associated with a significant decreased risk of death and embolic events in comparison with medical care[13].
Neurologic involvement,not rarely asymptomatic,may be demonstrated in about 50% of patients with infective endocarditis.Staphylococcus aureusis the more frequent etiologic agent.The timing of surgery in patients after embolic stroke is challenging and controlled studies are not available.Delay in surgery may be associated with risk of recurrent embolism,however patients undergoing early surgery are at the risk of hemorrhagic transformation of the stroke since full anticoagulation is needed for cardiopulmonary by-pass.Moreover,hypoperfusion during surgery may be associated to an extension of ischemic area.A careful multidisciplinary evaluation weighing the relative role of severity of hemodynamic impairment against that of neurologic damage may help in scheduling surgery.Results from observational studies suggest that the risk of further neurologic impairment is related more to severity of baseline neurologic damage than to surgery timing.In the case of hemorrhagic stroke surgery should be delayed at least 30 days.
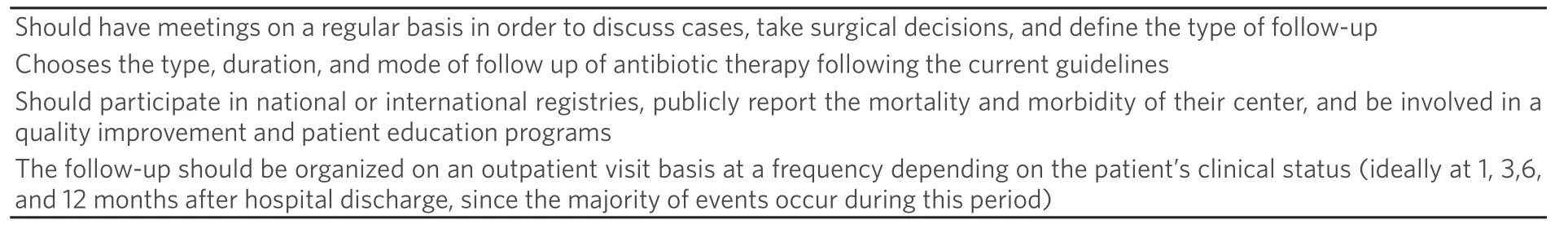
Table1.The endocarditis team - role

Table2.Factors related to choice of surgical strategy
ESC guidelines suggest that patients with IE should be referred to specialist centers and managed with a multidisciplinary specialized team (the “Endocarditis Team”) including “at least cardiac surgeons,cardiologists,anesthesiologists,infectious disease specialists,microbiologists and,when available,specialists in valve diseases,CHD,pacemaker extraction,echocardiography and other cardiac imaging techniques,neurologists,and facilities for neurosurgery and interventional neuroradiology” [Table1][11].An approach by a formalized multidisciplinary team led to a reduction in in-hospital and long-term mortality.This decrease in mortality was even more impressive since patients were old and suffered from several comorbidities[14,15].
Despite a clear indication,about 25% of all patients with IE still do not undergo surgery.Independent factors associated with a decision not to proceed with surgery include liver disease [odds ratio (OR) for surgery:0.16;95%CI:0.04-0.64],stroke before surgical decision (OR = 0.54;95%CI:0.32-0.90),andStaphylococcus aureusinfection (OR = 0.50;95%CI:0.30-0.85)[16].
A comprehensive multidisciplinary evaluation in IE may be extremely useful for the individualisation of proper surgical strategy,whose objectives are total removal of infected tissues and reconstruction of cardiac morphology.
With mitral and tricuspid involvement,the extent of valvular destruction and of extra valvular extension are the main determinant in the choice between valve repair and replacement.Involvement of valve leaflets,including perforation,favors mitral valve (MV) repair.Neo-chordae may be used in the case of isolated or multiple ruptured chordae.Extensive damage of a single leaflet or abscess formation are not necessarily a contraindication for valve repair.Extensive damage of the anterior leaflet,large lesions involving the posterior leaflet or the MV commissures and perivalvular extension with annular abscesses are considered the main technical difficulties for mitral repair.Intraoperative assessment of the valve after initial debridement allows to evaluate whether the remaining tissue is of sufficient quality to achieve a durable result.Intraoperative transesophageal echocardiography should guide surgeons in assessing residual valve regurgitation after valve repair [Table2].
MV repair vs. valve replacement
No randomized trial has been conducted comparing MV repair and replacement in patients with infective endocarditis.In light of present evidence,it may be ethically unfeasible in the future to conduct such randomized studies.Available information relies on observational studies often reporting a small number of patients.Valve repair has decreased risk of prolonged anticoagulation and to left ventricular geometric changes,which are associated with valve replacement.In a pivotal review by Feringaet al.[17],470/1194 (39%) patients with MV endocarditis underwent valve repair.In-hospital mortality (2.3%vs.14.4%) and longterm mortality (7.8%vs.40.5%) were significantly lower after valve repair in comparison with replacement.Moreover,after MV repair,the authors reported a significant decrease in the rates of early and late reoperation,early and late cerebrovascular events and late recurrent endocarditis.
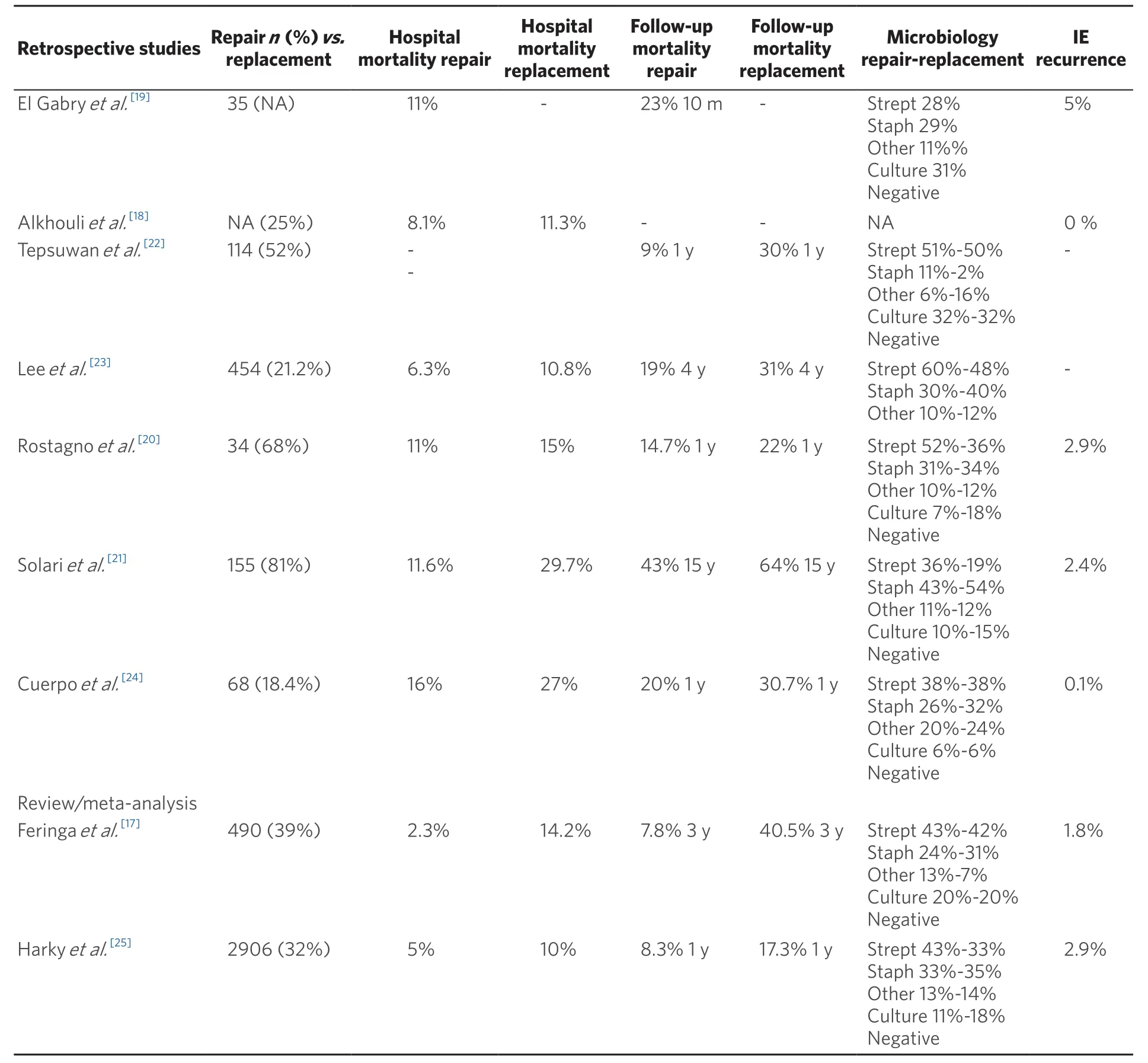
Table3.Results of study comparing MV repair and replacement in infective endocarditis
In the last decade,the number of patients with IE undergoing MV surgery has increased significantly as well as the number of mitral valve repair[18].However,the percentage of repairvs.replacement showed high variability in different centers.Overall MV repair is associated with a better outcome in comparison to valve replacement both in term of in-hospital and long-term mortality[19-25].Furthermore,the risk of recurrence of endocarditis is significantly lower after MV repair.Finally MV repair was associated with shorter length of hospitalization and reduced cost.Results were not significant influenced by the need for concomitant surgical procedures (CABG,aortic replacement,tricuspid repair/replacement),although MV replacement was sometimes preferred in these patients[25].It must be emphasized that patients who underwent MV replacement were on average older with more preoperative comorbidities and severe clinical conditions[22].
CONCLUSION
Results from previous investigations [Table3] suggest that MV repair in native MV endocarditis is associated with a significant decrease in early and long-mortality,endocarditis recurrence and need for reintervention.In particular,the risk of reinfection is significantly higher (from 8% to 27%vs.less than 3%) in patients with MV replacement.The number of patients undergoing repair is still highly variable in different centers (from 18% to 80%).Experience of surgical team in repair techniques is essential particularly when facing extensive damage of MV components.Low-volume centers show significantly lower repair rates with suboptimal results and higher re-intervention rate.Several limitations should be considered in the evaluation of studies reporting favorable results of MV repair in infective endocarditis.
Firstly,all published investigations are retrospective observational studies and no randomized control study has ever done comparing the two techniques.Considering present evidence,it appears difficult that it will ever be proposed in the future.Nevertheless,a selection bias may affect most of reported experience since valve replacement was mainly performed in patients with more severe clinical conditions and extensive valve damage.This may have contributed both to higher hospital and long-term mortality reported in valve replacement group.Concomitant surgical procedures were performed more frequently in patients undergoing valve replacement than in patients with MV repair,carrying a higher surgical risk.
Thirdly in the everyday life,management of MV endocarditis depends on experience of surgical teams.This appears the main determinant in the strategy adopted for surgery and its outcomes.A lower repair rates and less optimal outcomes,with residual valve regurgitation and need for re-intervention,has been reported in low-volume centers.
Finally,microbiological etiology may play a relevant role in establish surgical strategy.Staphylococcus aureus related IE are associated with more extensive valve lesions and significantly higher mortality.A lower repair rate,although not uniformly reported in different centers,is often observed in patients with staphylococcus infection.
In conclusion,MV repair may be considered the first choice treatment of MV endocarditis “with favorable anatomy” in experienced centers.However,multidisciplinary evaluation should direct definite choice in the individual patient.
DECLARATIONS
Authors’ contributions
The author contributed solely to the article.
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
The author declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
