Brain metastasis as exclusion criteria in extensivestage small cell lung cancer trials: a trend over decades
2020-07-30TakefumiKomiyaGerardChaayaLeighDeshotelsEmilyPowellAchutaKumarGuddati
Takefumi Komiya, Gerard Chaaya, Leigh Deshotels, Emily Powell, Achuta Kumar Guddati
1Medical Oncology, Parkview Cancer Institute, Fort Wayne, IN 46845, USA.
2Section of Hematology/Medical Oncology, Tulane University School of Medicine, New Orleans, LA 70112, USA.
3Department of Internal Medicine, Tulane University School of Medicine, New Orleans, LA 70112, USA.
4Parkview Research Center, Mirro Center for Research and Innovation, Fort Wayne, IN 46845, USA.
5Medical Oncology, Augusta University, Augusta, GA 30901, USA.
Abstract Aim: To investigate the frequencies and trends of brain metastases (BMs) as exclusion criteria in extensive-stage small cell lung cancer (ES-SCLC) trials.Methods: We conducted a comprehensive search to identify prospective clinical trials in patients with ES-SCLC.PubMed searches were conducted with the key words “small cell lung cancer” and “extensive”. The online archives of 20 oncology journals were also searched. Recent review articles in ES-SCLC were also investigated for additional articles. Eligible studies must have enrolled primarily ES-SCLC and been published in English. Studies involving brain/chest radiation and brain metastasis-specific trials were excluded. Studies were categorized into allowed/undefined, conditional, or complete exclusion of BM.Results: In total, 491 published studies were identified by PubMed (240), journal websites (198), and review articles(53). Early publication year (1970-1999) and first-line/maintenance setting were associated with higher incidence of complete exclusion of cases with BMs (P < 0.0001 and 0.0233, respectively). Incidence of complete exclusion was 27% in the 1990s, and then decreased to 12% in the 2000s and 8% in the 2010s.Conclusion: A significant number of ES-SCLC trials continues to exclude patients with BM. Future studies need to ease eligibility regarding BM according to ASCO/Friends recommendations.
Keywords: Brain metastasis, small cell lung cancer, clinical trials
INTRODUCTION
Despite the introduction of cancer prevention, screening, and new treatment modalities, cancer remains the leading cause of human mortality in both men and women worldwide. According to the National Cancer Institute Surveillance, Epidemiology, and End Results Program, more than 600,000 people die annually from cancer in the United States[1]. To develop novel therapies and further improve outcomes,well-designed clinical trials recruit candidates in numerous clinical settings. Although they are intended to help physicians’ decision-making in future oncology patients, these trials are often restrictive in patient selection. Patients with unfavorable risk factors are not permitted to participate due to fear of safety risks,resulting in a lack of generalizability to the typical patient population.
In the real world, oncologists often face clinical scenarios that have not been addressed in previous trials.Patients in oncology clinics may not have the same clinical characteristics that are required for participation in trials, indicating potential discrepancies in patient populations between clinical trial and non-clinical trial settings. In fact, a retrospective review of lung cancer cases at a Canadian institution showed that 73%of their consecutive patients would have been trial-ineligible for their hypothetical trials with common eligibility criteria[2]. Due to lack of data in the trials, patients may develop unexpected outcomes with newly-developed treatments or be undertreated because of the fear of unknown risk.
To address the lack of generalizability in oncology clinical trials, the American Society of Clinical Oncology(ASCO) and Friends of Cancer Research proposed to the Food and Drug Agency (FDA) that clinical trials must ease eligibility criteria and suggested re-considering several items commonly listed in exclusion criteria[3-6]. These include presence of brain metastases (BMs), history of HIV/Hepatitis B/C, minimum age, organ dysfunction, and prior and concurrent malignancies. These items have been frequently listed in exclusion criteria due to historical concerns without valid scientific analysis[3-6]. Oncology patients with any of these clinical characteristics tend to be excluded from clinical trials even though they account for a significant proportion of all cancer cases in the real world.
In this study, we focused on the presence of BMs as an exclusion criterion in prospective clinical trials of extensive-stage small cell lung cancer (ES-SCLC). Frequency of trial exclusion due to presence of BMs was assessed to determine a trend over several decades.
METHODS
We conducted systematic screening to identify prospective clinical trials in ES-SCLC [Table 1]. The initial screening used PubMed search with key words “small cell lung cancer” and “extensive”. Twenty journals commonly publishing these studies were identified during the PubMed search:Journal of Clinical Oncology,British Journal of Cancer,New England Journal of Medicine,Lancet,Lancet Oncology,Cancer Research,Clinical Cancer Research,Annals of Oncology,Lung Cancer,Journal of Thoracic Oncology,Journal of National Cancer Institute,Clinical Lung Cancer,Cancer,International Journal of Cancer,American Journal of Clinical Oncology,European Journal of Cancer,Annals of Internal Medicine,The Oncologist,Cancer ChemotherapyandPharmacology, andOncotarget. Online archives of these journals were investigated for additional articles. Recently published clinical reviews about ES-SCLC were also identified and investigated for more articles[7-10].
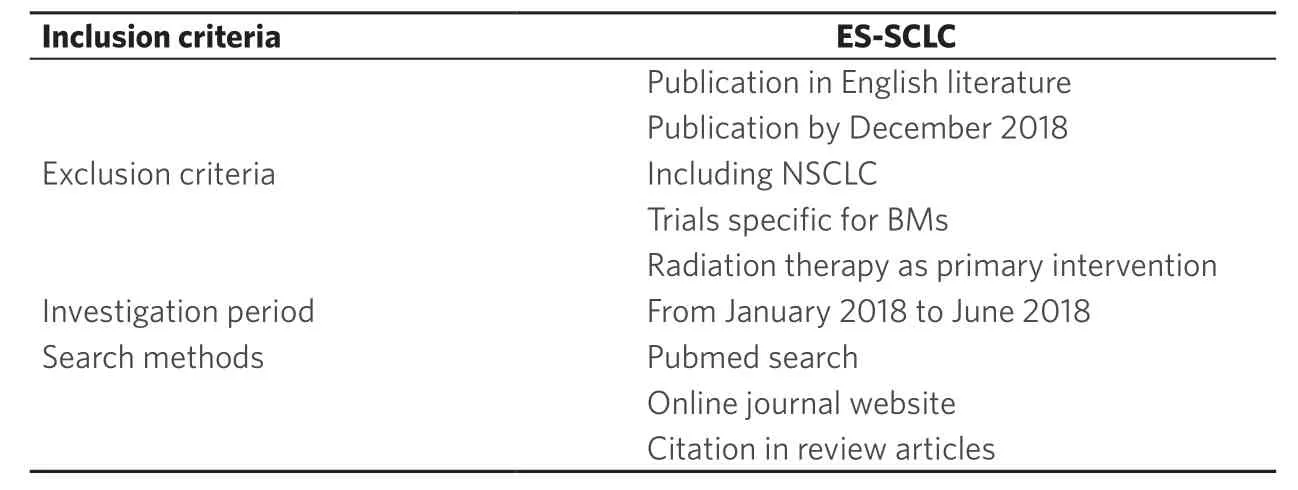
Table 1. Selection of ES-SCLC trials
Eligible studies must have enrolled primarily ES-SCLC and been published in English. Studies primarily investigating brain/chest radiation and BM-specific trials were excluded. Studies were categorized into allowed/undefined, conditional (e.g., only previously treated or asymptomatic BM are allowed), or complete exclusion of BM. Chi-squire test was used for categorical group comparison. Two-sidedP-values of less than 0.05 were defined as statistically significant.
RESULTS
The screening for clinical trials in ES-SCLC identified 240, 198, and 53 distinct articles by PubMed, journal website archives, and review articles, respectively. Characteristics of the trials are shown in Table 2. Most of the studies are published in journals with impact factor < 10, publication year 2000 or later, non-US sites,phases other than phase III, first-line setting, non-randomized, fewer than 100 patients, performance status other than 0-1, and no age limit. Radiographic screening of BM by magnetic resonance imaging (MRI) or computed tomography (CT) was mandated only in 32% (157 studies, data not shown). Anti-angiogenic agents were used only in 19 studies.
Early publication year (1970-1999) and first-line/maintenance setting were significantly associated with a higher incidence of complete exclusion of cases with BM (P< 0.0001 and 0.0233, respectively). The complete exclusion was 20% in earlyvs. 10% in late publication years, and 16% in first-line/maintenancevs. 8% in others. There was no correlation between the complete exclusion of BMs and other clinical characteristics including journal impact factor, region, trial phase, randomization, sample size, patient performance status, and age limit.
Studies in the 1990s had the highest incidence (27%) of complete exclusion, which decreased to 8% in the 2010s [Figure 1]. The conditional group increased from 25% in the 1970s to 34% in the 1990s and 79% in the 2010s.
DISCUSSION
Lung cancer is the most common cause of cancer mortality in the United States. Small cell lung cancer(SCLC), which accounts for approximately 15%-20% of all lung cancer cases, commonly presents with BMs[11-13]. Clinical trials in ES-SCLC focusing on systemic therapy often exclude patients with BMs primarily due to safety concerns; however, detailed incidence and trends in excluding BMs have not been investigated. The current study demonstrated that 8% of ES-SCLC trials in the 2010s still completely exclude patients with BM, whereas a recent analysis on non-small cell lung cancer trials at clinicaltrials.gov reported a complete exclusion rate of 14%[14].

Figure 1. A trend of brain metastasis as exclusion criteria in extensive-stage small cell lung cancer. Each bar indicates percentage of each group regarding exclusion of brain metastasis
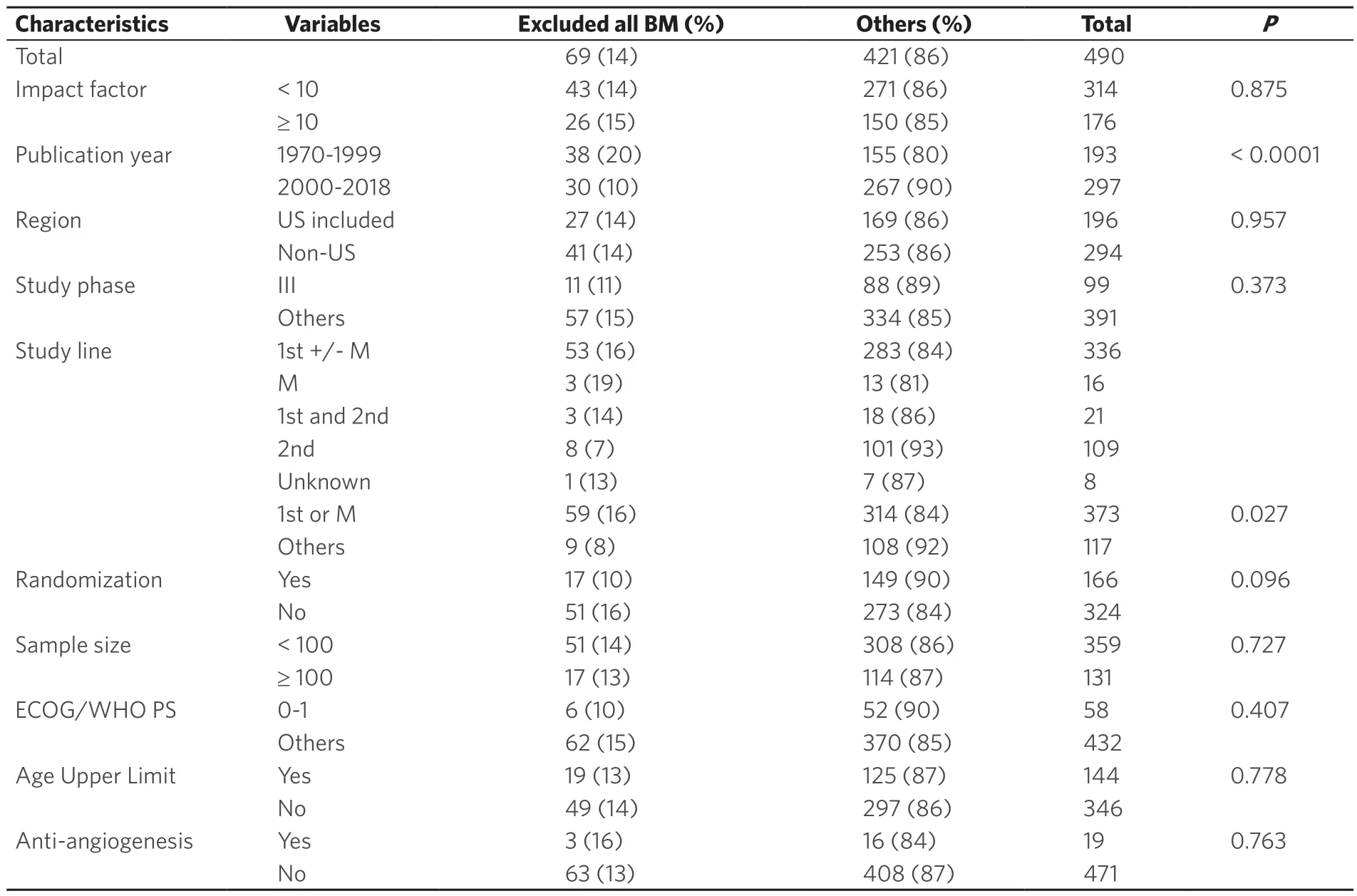
Table 2. Characteristics of studies in extensive-stage small cell lung cancer
ES-SCLC patients with BMs in the real-world setting do not benefit from clinical trials that do not include BM cases. New therapeutic interventions for these patients are unlikely to develop while they remain ignored by researchers. Expanding eligibility criteria to include patients with BMs would provide benefits in several aspects. In a population with a high incidence of BMs such as ES-SCLC, efficacy and safety effects unique to patients with BMs may exist. If the efficacy and safety of an investigational agent is assessed at an early phase, late phase studies may enroll patients to assess central nervous system (CNS) penetration along with related efficacy and safety. A successful example is a phase III trial comparing alectinibvs. crizotinib in advanced non-small cell lung cancer where alectinib demonstrated a CNS response rate of 81% in a population with 40% BM at baseline[12]. ASCO and Friends of Cancer Research strongly recommend investigation in patients with BMs in the setting of prospective trials rather than relying on post-marketing experience[4]. They state that previously treated and radiographically stable BM cases for at least four weeks should be included in prospective trials of all phases, whereas active/progressive BMs may require a studyto-study approach. A group from the FDA supports their recommendation by suggesting exclusion of only those who are symptomatic or are taking medications with known drug interactions[13].
Current staging methods of SCLC includes CT scans of chest/abdomen/pelvis, positron emission tomography scan, mediastinal staging procedures via bronchoscopy, and MRI of the brain. Lesions in the CNS have been previously assessed only clinically in early ages, while CT of the head came of use in the 1980s-early 1990s. With the now more recent use of MRI, more asymptomatic BM cases are presumably detected, likely explaining the increase of the conditional group as commented above. However, radiographic screening of BM was mandated only in 32% of studies overall, and 23% of studies published in the 2010s (data not shown). Changes in the management of BMs may also explain the trend over the decades. As stereotactic radiosurgery became available for small CNS lesions, more cases were identified that were previously treated with radiation therapy. In fact, the cases in the conditional group have grown over the decades [Table 2].They also include asymptomatic cases, those previously treated with radiation or surgery, and those in stable condition without the need for high dose steroids.
We are aware that removing restrictions in eligibility criteria may not necessarily result in rapid increases in enrollment of the previously-excluded population. For instance, a recent trial in extensive-stage SCLC that allowed the presence of BMs accrued a very limited number of patients[15]. Attitudes of investigators will hopefully change as ASCO/Friends recommendations become more appreciated in the next several years.
We acknowledge limitations in this study. With a retrospective search, there might be studies not covered by our search strategy. Studies not available in English publication were excluded, indicating potential publication bias. The articles in the earlier years had limited space to provide information such as detailed eligibility criteria, whereas recent articles can be more informative with online supplemental datasets.Information regarding eligibility of patients with leptomeningeal metastases were not available in most studies. Few agents with specific concerns on CNS disease such as anti-angiogenesis drugs have been tested in a limited number of trials. These potential biases may need to be considered for the interpretation of this study.
In conclusion, a significant number of ES-SCLC trials continue to exclude patients with BM, although conditional allowance has increased over the decades. Future studies need to further ease eligibility regarding BM according to ASCO/Friends recommendations.
DECLARATIONS
Acknowledgments
We thank the Parkview Research Center for administrative support.
Authors’ contributions
Substantial contributions to conception and design of the study and performed data analysis and interpretation: Komiya T
Data acquisition, as well as provided administrative, technical, and material support: Komiya T Manuscript writing: Komiya T, Chaaya G, Deshotels L, Powell E, Guddati AK
Availability of data and materials
List of clinical trials as primary data source can be found as supplemental information.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
