CerebrospinaI fluid amyIoid beta and tau proteins in atypicaI Parkinsonism: a review
2020-07-28VasiIiosConstantinidesGeorgeParaskevasFotiniBoufidouMaraBourbouIiPanagiotisParaskevasLeonidasStefanisEIisabethKapaki
VasiIios C.Constantinides, George P.Paraskevas, Fotini Boufidou, Mara BourbouIi, Panagiotis G.Paraskevas, Leonidas Stefanis, EIisabeth Kapaki
11st Department of Neurology, National and Kapodistrian University of Athens, Athens, P.C.11528, Greece.
2Department of Neurology, University of Crete, Heraklion 70013, Greece.
3Department of Nursing, Technological Educational Institute of Crete, Heraklion 71500, Greece.
Abstract Progressive supranuclear palsy, corticobasal degeneration, multiple system atrophy and dementia with Lewy bodies are the most common causes of atypical Parkinsonism and enter the differential diagnosis of Parkinson's disease.multiple system atrophy, dementia with Lewy bodies and Parkinson's disease are synucleinopathies,whereas progressive supranuclear palsy and corticobasal degeneration are tauopathies.Multiple cerebrospinal fluid markers have been applied on cohorts of patients with Parkinsonism, with the aim to develop biomarkers for these disorders.Total tau (τT), phosphorylated tau at threonine 181 (τP-181) and amyloid-beta with 42 amino acids(Aβ42) are considered classical biomarkers for Alzheimer's disease.The aim of the present study is to review the literature regarding these classical cerebrospinal fluid biomarkers in cohorts with Parkinsonism, as well as present data on novel approaches regarding analysis of these proteins.
Keywords: Biomarkers, cerebrospinal fluid, progressive supranuclear palsy, corticobasal degeneration, multiple system atrophy, dementia with Lewy bodies, tau protein, phosphorylated tau protein, amyloid beta
INTRODUCTION
Parkinson's disease (PD) is the most common neurodegenerative movement disorder.The pathologic hallmarks of PD are Lewy bodies, which consist of intraneuronal cytoplasmic depositions of pathological a-synuclein[1].Thus, PD is considered a synucleinopathy.Clinical diagnosis of PD is straightforward in typical cases.However, it can be problematic in patients with atypical clinical features.Accuracy of clinical diagnosis of PD is suboptimal, since as many as 25% of patients can be misdiagnosed[2].
Progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), multiple system atrophy (MSA)and dementia with Lewy bodies (DLB) are the most common causes of atypical Parkinsonism.All of these diseases manifest with Parkinsonism, which is poorly or only transiently responsive to dopaminergic treatment.
MSA is a synucleinopathy, like PD.Its pathologic hallmark is glial cytoplasmic inclusions, which consist of abnormal a-synuclein deposition in oligodendrocytes[3].DLB is also a synucleinopathy, characterized by predominantly cortical Lewy bodies[4].PSP and CBD on the other hand are considered tauopathies, since their main pathologic findings (tufted astrocytes and astrocytic plaques, respectively) consist of abnormal tau protein aggregates in astrocytes[5,6].
Tau protein can present in six isoforms, depending on the alternate splicing of the microtubule associated protein tau (MAPT) gene[7].This results in the variable expression of no, one or two oligonucleotides (N1 and N2) coded by exons 2 and 3 of theMAPTgene, as well as the presence of 3-repeat (3R) or 4-repeat(4R) microtubule binding regions coded by exon 10.Depending on the predominance of 3R- or 4R-tau isoforms, tauopathies are further divided into 4R- or 3R-tauopahies.PSP and CBD are considered 4-repeat(4R) tauopathies, Alzheimer's disease (AD) is a mixed 3R- and 4R-tauopathy, whereas Pick's disease is a 3R-tauopathy.
Total tau protein (τT), phosphorylated tau protein at threonine 181 (τP-181) and amyloid beta with 42 amino acids (Aβ42) are well-characterized cerebrospinal fluid (CSF) biomarkers of AD.These biomarkers have been incorporated into the most recent AD diagnostic criteria[8]and are the basis of the recently proposed AT(N) taxonomy system, which introduces biomarkers (according to their molecular specificity) for thein vivopathological characterization of patients with AD[9].
The aim of this review is to present data on the utility of these three classical CSF biomarkers (τT, τP-181and Aβ42) in the differential diagnosis of atypical Parkinsonism from PD.To this end, only studies which included patients with atypical Parkinsonismvs.PD or healthy controls are included.
This review includes representative studies which either have established our current knowledge on CSF biomarkers in Parkinsonism or provide new insights on the subject [Table 1].
STUDIES IN PSP
Most studies do not report any differences in CSF Aβ42between PSP and other causes of Parkinsonism or controls[10-16].Interestingly, however, some studies have reported lower Aβ42values in PSP compared to controls[17-19].Moreover, a single study reported lower Aβ42levels in PSPvs.PD[19].According to this study,Aβ42could differentiate PSP from PD with 83% sensitivity and 67% specificity.
Regarding CSF τT, several studies could not establish any differences between PSP patients and controls[13-17].Likewise, no difference in τTwas evident between PSP and CBD[13,15-17], MSA[13,15,16]or PD[15,16]in most studies.Two studies have supported that PSP patients exhibit lower τTlevels when compared to controls[18,19], whereas a single study posited that patients with PSP have lower τTlevels compared to CBD,but higher τTlevels compared to PD[12].

Table 1.Overview of the studies with data on classical CSF biomarkers in cohorts with Parkinsonism
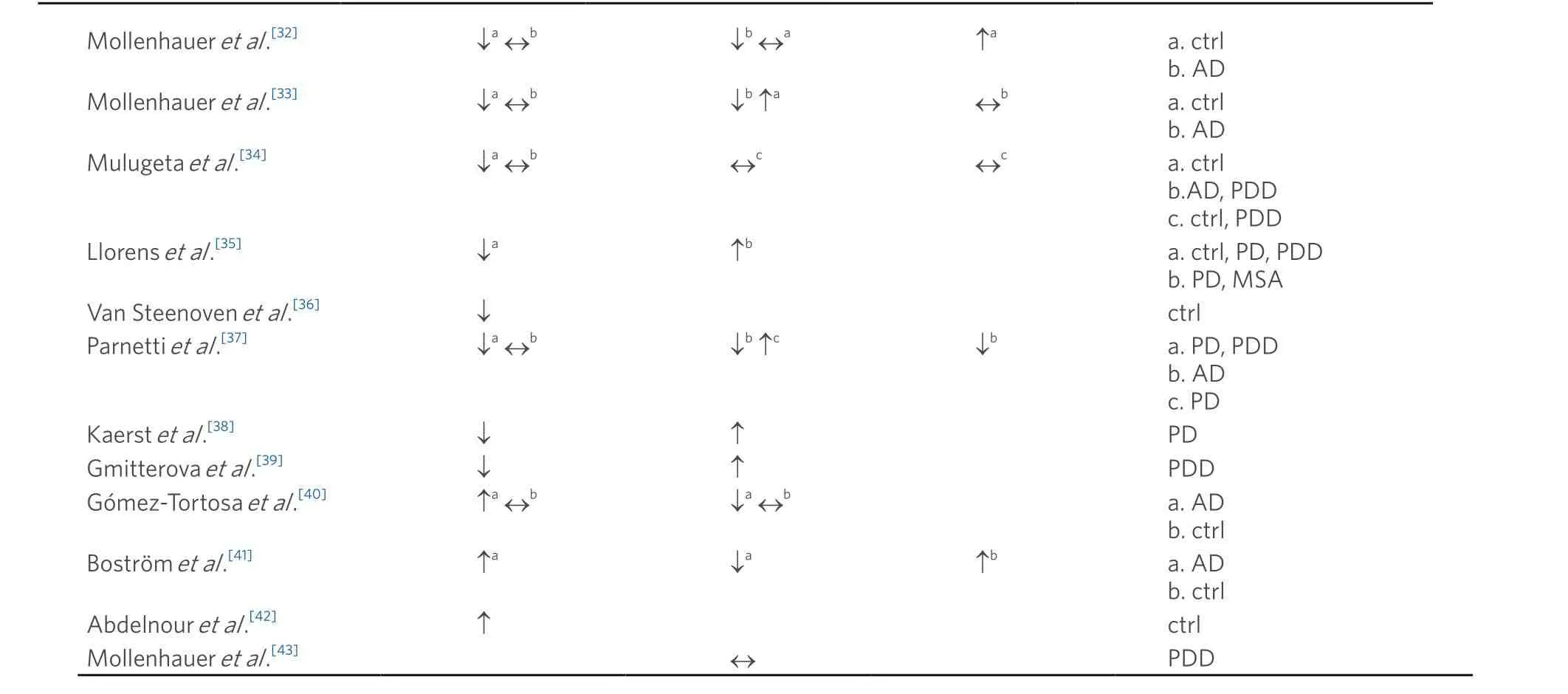
↑: elevated CSF levels; ↓: decreased CSF levels; ↔: no difference in CSF levels; CSF: cerebrospinal fluid; AD: Alzheimer's disease; PD:Parkinson's disease; MSA: multiple system atrophy; PSP: progressive supranuclear palsy; CBD: corticobasal degeneration; DLB: dementia with Lewy bodies; PDD: parkinson's disease dementia
CSF τP-181does not seem to be useful in the differentiation of PSP from other causes of Parkinsonism or controls[12,14-18].Two studies have reported lower τP-181levels compared to controls[13,19].
Few studies include data on ratios of CSF biomarkers.In a large study, which included PSP, CBD and AD patients, elevated τP-181/Aβ42ratio values could differentiate AD from PSP and CBD[17].Another study posited that lower τP-181/ τTratio values could discriminate patients with atypical Parkinsonism (PSP and MSA) from PD[20].This ratio was optimal for discriminating PSP from CBD with a reported sensitivity of 86% and specificity of 75%[12].PSP patients could also be differentiated from controls by lowerand higherratios.
A single study examined classical CSF biomarkers in different phenotypes of PSP.To this end, patients with classic Richardson's syndrome (RS) were compared to patients with PSP-Parkinsonism (PSP-P).Interestingly, only patients with PSP-P had elevated total τTlevels, compared to RS, PD and controls.Aβ42on the other hand was significantly lower in RS patients compared to PSP-P[20].
Few PSP patients seem to harbor a CSF-AD profile (generally defined as decreased Aβ42with elevated τTor τP-181).In a large cohort, including diverse neurodegenerative disorders, 10% of PSP patients had a CSFAD profile, as determined by an index incorporating CSF Aβ42and τP-181values[14].Likewise, only one of 19 PSP patients (~5%) had a typical CSF-AD profile, as determined by abnormal Aβ42, τTand τP-181values, in a cohort of patients with Parkinsonism[16].
Lastly, the possible relationship between CSF biomarkers and clinical characteristics has also been extensively studied in PSP.Most studies agree that there is no clinical-biochemical correlation in PSP[12-15,17].Two studies have correlated low Aβ42levels with higher disease severity, as measured by Hoehn and Yahr score[10]or the PSP Rating Scale[19].
As a general conclusion, there are no significant abnormalities in the classical CSF biomarkers in PSP.Despite being a 4R-tauopathy, CSF tau proteins do not seem to differ between PSP and other Parkinsonian disorders.CSF total tau protein, which is considered a non-specific marker of neurodegeneration, would be expected to increase in PSP, as is the case in AD.A plausible explanation would be that tau protein in PSP is concentrated intracellularly (in astrocytic plaques, tufted astrocytes and neurofibrillary tangles), and for this reason it does not enter the cerebrospinal fluid.
Additionally, no obvious clinical-biochemical correlation has been observed, while an AD biomarker profile in PSP (indicating an AD co-occurrence or possibly a PSP-like phenotype of AD) is a rarity.The presence of a CSF-AD profile in PSP patients is more likely to be indicative of the presence of dual underlying pathologies (AD and PSP), since pathological studies have not established a correlation of AD pathology and Richardson syndrome (the most common phenotype of PSP).
STUDIES IN CBD
Most studies have focused on CSF tau proteins in CBD, since CBD is a tauopathy.Several of these studies have reported elevated levels of τTin CBD, compared to controls[12,16,21-23], PSP[12,22,23]and PD[12,13].Interestingly, τTcould differentiate CBD from PSP with 80% specificity and sensitivity in one study[23].Likewise, CSF τTprovided 75% sensitivity and 90% specificity in the discrimination of CBD from PD in another study[12].However, no difference in τTbetween CBD and controls[14,15,17], PSP[13,15,16,20], MSA[15,16]and PD[15,16]has also been reported.
Regarding CSF τP-181, most studies did not establish any meaningful difference between CBD patients and other Parkinsonian disorders or controls[13-17].A single study has reported elevated CSF τP-181levels in CBD compared to PD[12], and another study in CBD patients compared to MSA patients[13].
CSF Aβ42levels do not differ in CBD compared to other Parkinsonian disorders, according to several studies[12,13,15,17].However, lower Aβ42has been described in CBD patients compared to controls[14,17]and PD[16].
Regarding CSF biomarker indices, few studies have included relevant data in CBD.One study reported decreased Aβ42/τTratio in CBS compared to PD and controls, whereas τP-181/τTratio in CBS was decreased compared to controls[12].According to this study, τP-181/τTwas optimal for PSPvs.CBD discrimination (86%sensitivity and 75% specificity).Another study posited that CBD patients have elevated τT/Aβ42and τP-181/Aβ42compared to PD[16].
Clinical and demographic data do not correlate with levels of classical CSF biomarkers in CBD, according to most relevant studies[13-15].A single study reported that cognitive status, as measured by MMSE,correlated with both τTand τP-181levels and was inversely correlated with Aβ42levels[12].Intriguingly,τTlevels in CBD and PSP were dependent on disease severity in a single study, with maximal levels in medium-stage disease[23].
Few studies have focused on the presence of a CSF-AD profile in cohorts of Parkinsonian disorders.According to this approach, patients are divided in those harboring a CSF-AD profile and those who do not harbor such a profile.An initial study concluded that 20% of CBS patients harbored a CSF-AD profile(as defined by τT> 400 pg/mL, Aβ42< 400 pg/mL and τT/Aβ42ratio > 1)[24].In another cohort, 38% of CBS patients had a CSF-AD profile, based on an index which included τP-181and Aβ42values[14].Along the same lines, a third study posited that ~30% of CBS patients had a typical CSF-AD profile (elevated τTand τP-181combined with decreased Aβ42)[16].Interestingly, when patients with a CSF-AD profile were excluded from analyses, an initially reported elevated τTand decreased Aβ42protein in CBS disappeared, and CBS patients no longer differed from PD or controls.This implied that the elevated τTand decreased Aβ42levels in CBS might have been the result of the inclusion of AD patients who presented with a CBS phenotype.The CSF profile was implemented in another study by the same study group to investigate possible differences between AD and non-AD pathology in a CBS cohort[25].
In conclusion, abnormalities in classical CSF biomarkers are common in CBD.The commonly reported elevation in τTand τP-181and decrease in Aβ42, does not seem to be a biochemical fingerprint of CBD but rather is a result of the inclusion in analyses of patients with AD pathology and a CBS phenotype.Up to 30% of CBS patients have an AD-biomarker profile, which is in accordance with pathological studies.Thus,CSF biomarkers are particularly useful tools in thein vivodiscrimination of corticobasal syndrome in CBSnon-AD and CBS-AD.
STUDIES IN MSA
An initial study on CSF Aβ42in MSA reported lower levels compared to PD, PSP and controls[10].A different study group also found lower Aβ42levels in MSA compared to controls[26].However, several other studies could not establish any meaningful difference in Aβ42levels in MSA compared to other Parkinsonian disorders or controls[11,13,15,16,20,26,27].
Results regarding τTin MSA are conflicting, with most studies reporting an increase of τTin MSA compared to either controls[20,28,29]or other Parkinsonian disorders[13,20,29-31].However, some studies have reported no difference between MSA and other Parkinsonian disorders[16,26,27], whereas a single study has supported that MSA patients exhibit lower τTcompared to controls[26].
Few studies have included τP-181data in the comparison of biomarkers in MSA and other Parkinsonian disorders.These studies did not find any difference in τP-181levels in MSA compared to other study groups[15,16,20,26].A single study has supported lower τP-181levels in MSA compared to PD and controls[13].
Two studies have included CSF biomarker indices in the differential diagnosis of MSA from related disorders.More specifically, a study has supported that MSA patients have significantly lower τP-181/τTratios compared to PD[20].Another study posited that higher values of τT/Aβ42ratio could differentiate MSA from PD with high specificity but only moderate sensitivity[16].
Regarding disease subtypes, MSA-C and MSA-P patients did not differ in their CSF biochemical profile in all relevant studies[11,20,28,30].
Clinical-biochemical correlation studies in MSA are sparse.A study correlated disease severity in MSA with lower CSF Aβ42levels[10].Another study supported that both τTand τP-181levels increased with age in MSA[26].A study implementing a battery of CSF biomarkers in a cohort of diverse neurodegenerative disorders could not establish any correlation between CSF biomarkers and clinical characteristics[15].In conclusion, data on classical CSF biomarkers are largely inconclusive.
STUDIES IN DLB
It is well documented that CSF Aβ42in DLB is decreased compared to controls[14,32-36], PD[35,37,38]and parkinson's disease dementia (PDD)[35,37,39]according to the majority of studies on the subject.Comparison of Aβ42levels between AD and DLB has yielded conflicting results, with some studies reporting greater Aβ42levels in DLB compared to AD[14,40,41], and other studies not reporting any significant difference between the two groups[32-34,37].A single study reported greater Aβ42values in DLB compared to controls[42]and another study did not find any difference between the two groups[40].Another study did not report a difference between DLB and PDD[34].There is consensus among studies that CSF τTis increased in AD compared to DLB[14,32,33,37,40,41].DLB patients have been reported to harbor elevated τTlevels compared to controls[14,33], although several studies could not establish any difference between DLB and controls[32,34,40].Regarding other synucleinopathies (PD,PDD and MSA), studies have produced mixed results, reporting either an increase in τTin DLB compared to PD/PDD[35,37-39]and MSA[35]or no difference among patient groups[34,43].
Few studies have included τP-181in analyses of DLB cohorts.According to these limited studies, τP-181is elevated in AD compared to DLB[14,37], although one study could not establish a difference between AD and DLB[33].Comparison between DLB and controls regarding τP-181has produced mixed results, with some studies reporting an increase in τP-181in DLB[14,32,41], whereas other studies could not establish any difference between groups[34].PD/PDD patients do not differ from DLB in their τP-181profile[34,44].
Lower CSF Aβ42levels in DLB correlate with a worse outcome, according to several studies[14,40,42,45].Likewise, elevated τTlevels correlate with a poorer prognosis in DLB[37-39,41].
Several studies in DLB, which contain longitudinal data regarding CSF biomarker level alterations over time, provide conflicting results.Two studies have reported stable Aβ42over time in cohorts of DLB patients[39,46].According to these studies, CSF τTand τP-181levels either increase[39]or decrease over time[46].Conversely, two other studies have provided a different profile, with unaltered τTand τP-181levels over time,combined with a decrease in Aβ42during the transition from prodromal to demented stage of DLB[47,48].
A CSF-AD profile (as defined by a decrease in Aβ42and an increase in τTand/or τP-181) is common in DLB patients, presenting in 25%-50% of patients[14,42,45,49].This profile invariably correlates with poorer prognosis[42,45].According to a recent study, as many as 85% of DLB patients have decreased Aβ42in CSF,either isolated (45%) or in the context of a CSF-AD profile (40%)[49].
A single study has provided insight into the relationship between pathological finding and CSF biochemical profile[44].In this cohort, 72% of DLB patients had senile plaques and 50% had neurofibrillary tangles.Interestingly, there was a correlation between the presence of senile plaques and CSF Aβ42levels.The cooccurrence of neurofibrillary tangles did not affect τTand τP-181levels in DLB patients.
In conclusion, there is a general agreement that Aβ42levels are decreased in DLB, either alone or accompanied by increased τTor τP-181levels.The decrease of Aβ42levels have been shown to correlate with faster disease progression.Decreased CSF Aβ42levels and increased τTand τP-181in DLB could be attributed to the frequent co-occurrence of AD pathology in patients with Lewy body disease.This hypothesis would explain the correlation of a CSF-AD profile with worse outcomes in DLB patients.Intriguingly, multiple lines of evidence suggest an interplay between a-synuclein and tau/amyloid beta aggregation, which may explain the frequent co-occurrence of AD pathology and Lewy body disease[50-52].
METHODOLOGICAL CONSIDERATIONS
Most studies on classical biomarkers in atypical Parkinsonism implemented enzyme-linked immunosorbent assays (ELISAs).Advantages of ELISAs include relatively low cost, high reproducibility and high availability, since commercial ELISAs of classical CSF biomarkers are readily available.There have been efforts, however, to implement novel techniques and to target different proteins in search of new biomarkers in neurodegenerative diseases.
To this end, a study examined differences in tau isoforms in CSF, which may reflect differences in posttranslational processing of tau protein.More specifically, differences in tau proteolytic products in CSF were the main study endpoint.By means of immunoprecipitation, extended (55 kDa) and truncated forms(33 kDa) of tau protein were determined in CSF.The tau 33 kDa/55 kDa ratio was significantly lower in PSP patients, compared to patients with AD, FTD, CBD, PD and DLB and emerged as a possible biomarker for PSP[53].The same study group replicated these results in a larger cohort[54].However, these promising results were not be replicated by another study group[55].
In another study, immuno-PCR essays were developed to measure 3R- and 4R-tau isoforms in CSF.These essays were tested in four different cohorts, which included PSP, CBD, PDD and PDD patients.The study we are referring to included four cohorts, in which the 3R and 4R-tau isoform levels varied considerably among the four cohorts (mean values in control groups ranging for both 3R- and 4R-tau from < 5 pg/mL to ~50 pg/mL).Analysis of tau isoforms in all cohorts combined indicated lower 4R-tau levels in PSP and AD.3R-tau did not differ among study groups.The 3R-tau/τTand 3R-tau/τP-181ratios were decreased in AD compared to PDD.The 4R-tau/τTwas lower in PSP and AD compared to controls and the 4R-tau/τP-181ratio was higher in PDD compared to PSP, CBD and AD[56].
Wagshalet al.[18]developed a multitude of novel ELISAs, which target different epitopes of tau proteins, in order to examine differences in the concentration of diverse tau protein fragments in CSF.These ELISAs were applied in patients with AD, PSP and controls.Interestingly, PSP patients had lower concentrations of most tau fragments compared to controls.
Another study group implemented mass spectrometry to quantify tau-specific peptides in the entire sequence of tau protein in a cohort of PSP, AD and DLB.This novel approach yielded data for 18 tau peptides.By use of these peptides, the authors determined that the 1N and 3R-tau isoforms were mostly represented in CSF.Levels of tau peptides were intra-correlated and significantly increased in AD patients.Interestingly, AD patients had relatively decreased levels of peptides in the central core region of tau protein.This region contains phosphorylation sites, which may explain this finding[57].
Along the same lines, Cicognolaet al.[58]developed novel antibodies against tau fragments at amino acid 123 and 224 (tau-123 and tau-224, respectively), after having identified endogenous tau fragments ending at these amino acids.They concluded that anti-tau-224, but not anti-tau-123, was present in neurofibrillary tangles and neuropil threads of AD patients, whereas tau-224 levels were elevated in CSF of these patients and correlated with conversion from mild cognitive impairment to AD.The authors concluded that only tau-224 is neuron-specific, whereas tau-123 may represent a general non-specific marker of tau metabolism.
DISCUSSION
There has been extensive research on classical CSF biomarkers in patients with Parkinsonism, as illustrated in this review of the literature.Most studies agree that PSP patients do not exhibit a specific CSF biochemical profile.Few studies have reported decreased Aβ42levels.A CSF-AD profile has rarely been described in PSP patients.
An elevation in CSF τTlevels has been systematically reported in CBS.Moreover, few studies have also documented a decrease in Aβ42and an increase in τP-181in these patients.Interestingly, a significant percentage (< 40%) of CBS patients can harbor a CSF-AD profile[14,16,24].This is in agreement with clinicalpathological studies of CBS[59-62], where AD is a relatively common underlying pathology of CBS.A study emphasized that the frequently reported elevation in CSF τTand reduction in Aβ42in CBS might not represent an inherent biochemical characteristic of CBS and could be attributed to the inclusion of AD patients presenting with CBS[16].Thus, classical CSF biomarkers are particularly important in CBS cohorts,since they can indicate an underlying AD pathology.
Regarding MSA, most studies report an elevation in CSF τTprotein, whereas a decrease in Aβ42levels in MSA has been rarely reported.Although an interplay between a-synuclein and Aβ42has been established in vitro, alterations in CSF Aβ42levels in a synucleinopathy are difficult to explain[63].In a transgenic mouse model with expression of both β-amyloid peptides and synuclein, β-amyloid peptides promoted aggregation of a-synuclein[50].Likewise, pathological data from PD and DLB patients support the accumulation of tau oligomers in these brains.Moreover, oligomeric tau forms may co-exist in the same aggregates with a-synuclein, forming hybrid oligomers[51].Along the same lines, a-synuclein may induce specific toxic tau oligomers in cell cultures[52].
DLB patients exhibit significantly lower CSF Aβ42values compared to other Parkinsonian disorders.Moreover, studies support that τTin DLB may be elevated.However, AD can be differentiated from DLB by means of a significant increase in τTand τP-181in AD compared to DLB.A significant percentage of DLB patients harbor a CSF-AD profile, which indicates the frequent co-occurrence of Lewy body and AD pathologies, especially in older patients.
CONCLUSIONS AND FUTURE DIRECTIONS
Classical CSF biomarkers in atypical Parkinsonism are important, particularly for the diagnostic workup of CBS and DLB patients.A CSF-AD profile in a CBS patient indicates an underlying AD pathology.Conversely, in DLB patients, the presence of a CSF-AD profile indicates the co-occurrence of AD and Lewy body pathologies, which usually correlates with poorer prognosis.Although some differences have been reported in classical CSF biomarkers in both PSP and MSA, the results are inconsistent and require further research.
The disparity of results on classical biomarkers in atypical Parkinsonism can be largely attributed to the great heterogeneity of studies.This heterogeneity refers to diagnostic criteria, cohort synthesis, statistical analysis and pre-analytical and analytical factors.Standardization of these pre-analytical and analytical confounders, as established in recent recommendations, is paramount for more robust results[64].Moreover,large cohorts of Parkinsonian disorders with CSF biomarker data and pathology-confirmed diagnoses are lacking.These studies would reliably inform us on the interplay between CSF biomarkers and pathological findings.This disparity in results also illustrates the limitations of classical biomarkers in the differential diagnosis of patients with Parkinsonism, and emphasizes the need for novel approaches.
To this end, differences in isoforms of these known proteins (e.g., 3R-vs.4R-tau protein), differences in proteolytic products and quantification of specific peptides of these proteins are promising new approaches.Moreover, better characterization of other proteins which may serve as biomarkers (such as a-synuclein or TDP-43) is of great importance.
DECLARATIONS
Authors' contributions
Conception of the study, drafting of the manuscript, literature review: Constantinides VC
Conception of the study, critical appraisal of manuscript: Paraskevas GP, Boufidou F
Conception of the study, critical appraisal of manuscript, literature review: Bourbouli M, Paraskevas PG
Conception of the study, critical appraisal of manuscript: Stefanis L, Kapaki E
AvaiIabiIity of data and materiaIs
Not applicable.
FinanciaI support and sponsorship
None.
ConfIicts of interest
All authors declared that there are no conflicts of interest.
EthicaI approvaI and consent to participate
Not applicable.
Consent for pubIication
Not applicable.
Copyright
© The Author(s) 2020.
杂志排行
Neuroimmunology and Neuroinflammation的其它文章
- Assessment of cerebrospinaI fluid α-synucIein as a potentiaI biomarker in Parkinson's disease and synucIeinopathies
- CerebrospinaI fluid biomarkers in idiopathic normaI pressure hydrocephaIus
- AUTHOR INSTRUCTIONS
- Phf15 - a novel transcriptional repressor regulating inflammation in a mouse microgIiaI ceII Iine
- An association between mitochondria and microglia effector function: what do we think we know?
- COVID-19 neurotropism and implications for therapy