老年隐匿性高血压病人长时血压变异性与左心室肥厚的相关性
2020-07-04邹超斌胡松文新平朱厚梅鞠萍毛拥军
邹超斌 胡松 文新平 朱厚梅 鞠萍 毛拥军
[摘要] 目的 探討老年隐匿性高血压(MH)病人长时血压变异性与左心室肥厚的相关性。
方法 选取老年体检者102例,根据诊室血压及7 d家庭自测血压,将受试者分为正常血压组(NH组)65例和MH组37例。所有受试者均通过超声心动图检测左心室舒张末期内径(LVDd)、舒张末期室间隔厚度(IVST)、左心室后壁厚度(LVPW)、左心室质量(LVM)、左心室质量指数(LVMI)等指标。
结果 MH组诊室收缩压、自测收缩压、自测舒张压、自测收缩压变异性、自测舒张压变异性、LVDd、LVPW、LVM、LVMI均显著大于NH组(t=3.448~28.928,P<0.05)。MH组自测收缩压变异性与LVDd、LVPW、LVM、LVMI呈正相关(r=0.336~0.600,P<0.01)。MH组病人自测收缩压变异性是LVDd、LVM、LVMI的独立影响因素。
结论 与正常血压人群相比,老年MH病人长时血压变异性升高,并与左心室肥厚呈正相关。
[关键词] 隐性高血压;老年人;血压测定;血压监测,便携式;心脏扩大;危险因素
[中图分类号] R544.1;R541.3
[文献标志码] A
[文章编号] 2096-5532(2020)03-0265-05
doi:10.11712/jms.2096-5532.2020.56.044
[开放科学(资源服务)标识码(OSID)]
[网络出版] http://kns.cnki.net/kcms/detail/37.1517.R.20200320.1519.006.html;2020-03-23 13:42:46
ASSOCIATION BETWEEN LONG-TERM BLOOD PRESSURE VARIABILITY AND LEFT VENTRICULAR HYPERTROPHY IN ELDERLY PATIENTS WITH MASKED HYPERTENSION
\ ZOU Chaobin, HU Song, WEN Xinping, ZHU Houmei, JU Ping, MAO Yongjun
\ (Department of Geriatric Medicine, The Affiliated Hospital of Qindao University, Qingdao 266100, China)
[ABSTRACT]\ Objective\ To investigate the association between long-term blood pressure variability and left ventricular hypertrophy in elderly patients with masked hypertension (MH).
\ Methods\ A total of 102 elderly patients who underwent physical examination were enrolled, and according to the blood pressure measured in the consulting room and the results of 7 day home blood pressure monitoring, they were divided into normal pressure group with 65 patients and MH group with 37 patients. Echocardiography was performed for all patients to monitor left ventricular end-systolic dimension (LVDd), end-diastolic interventricular septal thickness (IVST), left ventricular posterior wall thickness (LVPW), left ventricular mass (LVM), and left ventricular mass index (LVMI).
\ Results\ Compared with the normal pressure group, the MH group had significantly higher systolic pressure measured in the consulting room and systolic pressure, diastolic pressure, systolic blood pressure variability, diastolic blood pressure variability, LVDd, LVPW, LVM, and LVMI measured at home (t=3.448-28.928,P<0.05). In the MH group, systolic blood pressure variability measured at home was positively correlated with LVDd, LVPW, LVM, and LVMI (r=0.336-0.600,P<0.01), and systolic blood pressure variability measured at home was an independent influencing factor for LVDd, LVM, and LVMI.
\ Conclusion\ Compared with the population with normal blood pressure, the elderly patients with MH have greater long-term blood pressure variability, which is positively correlated with left ventricular hypertrophy.
[KEY WORDS]\ masked hypertension; aged; blood pressure determination; blood pressure monitoring, ambulatory; cardiomegaly; risk factors
隐匿性高血压(MH)是指诊室血压正常而诊室外血压异常升高的一种临床现象。PICKERING于2002年首次提出了MH的概念。目前国际上大多
数高血压指南将MH定义为:在未进行降压治疗的
个体中,诊室血压<18.62/11.79 kPa,24 h平均血压
≥17.29/10.64 kPa和(或)日间平均血压≥17.96/11.30 kPa和(或)夜间平均血压≥15.96/9.31 kPa;或者家庭血压监测(HBPM)的诊断阈值为≥17.96/11.30 kPa[1-2];在接受降压治疗的病人中,则定义为隐匿性未控制的高血压。近年来越来越多的研究表明,MH具有与持续性高血压(SH)相似的靶器官损
害和心血管病风险,MH才逐渐引起临床医生的注意。随着具有存储功能的自动电子血压计的普及,HBPM在高血压管理中的作用日益突出,该法能有效提高高血压的知晓率、控制率及高血压诊断的准确性,可以有效鉴别白大衣高血压及MH,同时可以观察比诊室血压及24 h动态血压更长时间的血压变异情况[3]。左心室结构异常是高血压靶器官亚临床损害的表现之一。既往研究表明,MH病人左心室肥厚患病率明显高于正常血压人群[4-6]。但是目前有关老年MH病人长时血压变异性(BPV)与靶器官损害的研究较少。本研究旨在探讨老年MH病人长时BPV与左心室肥厚的相关性。现将结果报告如下。
1 资料和方法
1.1 一般资料
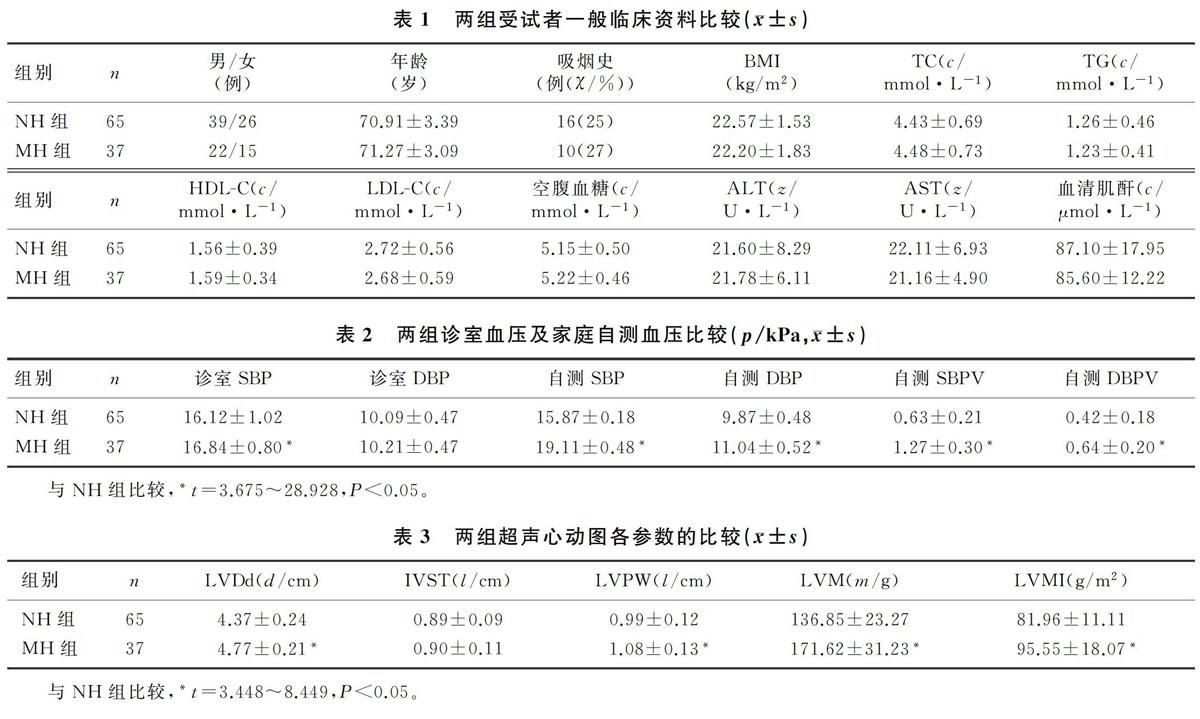
选择2018年8月—2019年6月在我院下属社区卫生服务中心体检的老年体检者102例。均排除继发性高血压、糖尿病、脑卒中、慢性心力衰竭、心肌梗死、免疫性疾病、感染性疾病、严重肝肾疾病、恶性肿瘤及长期卧床者。所有受试者均签署知情同意书。根据家庭自测血压和诊室血压将受试者分为两组,其中MH组37例,正常血压组(NH组)65例。高血压的诊断标准:在未使用降压药物的情况下,非同日3次测量诊室血压,收缩压(SBP)≥18.62 kPa和(或)舒张压(DBP)≥11.97 kPa[2]。MH的诊断标准:诊室血压<18.62/11.97 kPa,家庭自测血压≥17.96/11.30 kPa[7-9]。两组年龄、性别、吸烟史、体质量指数(BMI)、三酰甘油(TG)、胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、谷丙转氨酶(ALT)、谷草转氨酶(AST)、空腹血糖、血清肌酐等比较,差异均无统计学意义(P>0.05)。见表1。
1.2 方法
1.2.1 诊室血压的测量 嘱受检者坐位休息至少5 min,然后由经过专业培训的医务人员使用电子血压计(型号为HEM-7136)测量其优势手上臂血压3次,每次间隔1 min,连续测量3 d,取平均值。
1.2.2 家庭自测血压测量 所有受试者及其至少一名亲属接受家庭血压测量培训,经考核合格后,提供每位受检者1台通过国际标准认证的并且具有记忆功能的上臂式全自动电子血压计(型号为HEM-7136)。每天测量时间段为6:00—9:00、17:00—21:00,早上测量在起床后1 h之内、剧烈运动前、早餐前、排尿之后;晚上测量则需在晚餐后、睡覺之前进行。每次测量前静坐休息5 min,早晚各测量2次,每次测量2遍,间隔1~2 min,连续测量7 d[2]。去除第1天的血压测量值,将以后6 d连续血压测量值的标准差作为长时BPV。
1.2.3 超声心动图检查 应用彩色多普勒超声诊断仪,测定左心室舒张末期内径(LVDd)、舒张期室间隔厚度(IVST)及左心室后壁厚度(LVPW),连续测定3个心动周期,计算其平均值。根据Decerux公式,计算左心室质量(LVM)和左心室质量指数(LVMI)。左心室肥厚的诊断标准:LVMI>125 g/m2(男)及LVMI>110 g/m2(女)。
1.2.4 实验室检查 清晨采集空腹静脉血5 mL,应用全自动生化分析仪检测LDL-C、HDL-C、TG、TC、空腹血糖、ALT、AST、血清肌酐等。
1.2.5 统计学处理 应用SPSS 24.0软件进行统计分析。计量资料以±s表示,组间比较采用独立样本t检验;计数资料组间比较采用χ2检验;相关分析采用Pearson相关分析,多因素分析采用多元线性逐步回归分析。以P<0.05为差异具有统计学意义。
2 结果
2.1 两组诊室血压及家庭自测血压比较
与NH组比较,MH组诊室SBP、自测SBP、自测DBP、自测收缩压变异性(SBPV)、自测舒张压变异性(DBPV)均明显升高,差异有统计学意义(t=3.675~28.928,P<0.05);两组诊室DBP比较差异无统计学意义(t=1.179,P>0.05)。见表2。
2.2 两组超声心动图参数的比较
MH组LVDd、LVPW、LVM、LVMI均明显高于NH组,差异有统计学意义(t=3.448~8.449,P<0.05);两组IVST比较,差异无统计学意义(t=0.428,P>0.05)。见表3。
2.3 MH病人BPV与左心室各参数的相关性分析
Pearson 相关分析显示,MH病人自测SBPV与LVDd、LVPW、LVM、LVMI均呈正相关(r=0.336~0.600,P<0.01)。
2.4 MH病人左心室肥厚影响因素的多元线性逐步回归分析
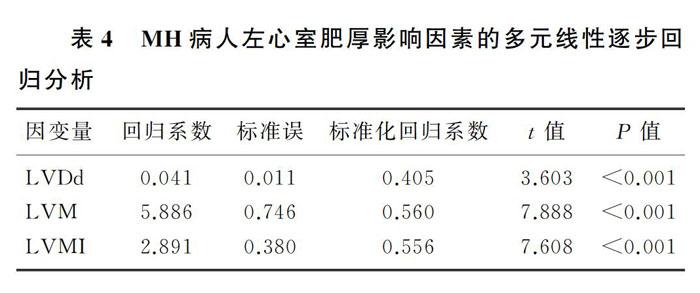
分别以MH组病人的LVDd、LVPW、IVST、LVM、LVMI为因变量,自测SBP、自测DBP、自测SBPV、自测DBPV、年龄、BMI、吸烟史、TC、TG、HDL-C、LDL-C、空腹血糖、ALT、AST、血清肌酐为自变量进行多元线性逐步回归分析,分析结果显示,自测SBPV为 LVDd、LVM和LVMI的独立影响因素。见表4。
3 讨论
由于缺乏典型的临床特征,MH常常容易被忽略。有横断面研究结果显示,由于研究对象的年龄、地域、种族及对MH定义的不同,MH患病率存在显著差异,在8%~49%之间[10-16]。MH对靶器官的损害更不易被察觉。既往研究结果表明,MH对靶器官的损害与SH相似,主要包括心、肾、脑等靶器官不同程度的损害[17];同时,MH比正常血压人群更容易进展为SH[18],是强有力的血管事件预测因子[5,19-20]。近年来,随着家庭自动电子血压监测技术的成熟和普及,MH及其导致的靶器官损害也越来越引起人们的关注。
目前评估诊室外血压的方式主要包括HBPM和动态血压监测(ABPM)。研究表明,与诊室血压相比,HBPM具有以下的优势:①能够识别白大衣高血压和MH;②能够提供比诊室更放松的测量环境;③能够增强病人积极参与自我血压管理的意识;④能够提供更长时间的血压测量值;⑤能够更好地预测靶器官损害和心血管事件,并提供更加准确的心血管危险分层[21]。有研究结果显示,HBPM与日间ABPM在正常血压阈值、重现性、诊断白大衣高血压和MH的准确性及预后价值方面存在良好的一致性[10,22-23],二者可以互为补充;与ABPM相比,HBPM还具有费用低、可重复性好、易推广等优点;HBPM不仅能够提供更加精确的血压读数,减少降压药物的过度使用,提高病人的治疗依从性和高血压的控制率,同时还可以评估更长时间的血压变异程度,有利于高血压病人的长期随访,从而为监测血压的长期变化提供了一种有效的方式。在过去的10年里,HBPM被越来越多的高血压管理指南推荐用于高血压管理的临床实践中[1,10,24]。
BPV是指一定时间内血压的变化程度,通常使用一段时间内多次血压测量值的标准差、变异系数表示。根据血压测量时间段的长短可将BPV分为短时[25]和长时血压变异。其中长时变异包括数日、数月、数年甚至更长时间的血压变异情况,血压测量次数及准确性、动脉壁的弹性、气候变化、降压药物的使用等均可对其造成影响[26-27]。BPV监测模式包括诊室血压测量、ABPM以及HBPM,不同的测量方法和测量时间间隔都会对BPV产生影响。有研究认为,HBPM可以提供长时血压变化的信息,在高血压靶器官损伤发生和恶化的判断中起着重要和独立的作用[28-30]。CACCIOLATI等[31]根据诊室血压和家庭自测血压将1 701例老年人分為NH组、白大衣高血压组(WCH组)、MH组、SH组进行研究,结果显示,MH组的BPV均明显高于NH组及WCH组,而与SH组相似。本研究结果也显示,MH组病人的长时BPV显著高于NH组。
ROTHWELL等[32]研究发现,BPV是高血压靶器官损害和心血管事件的独立预测因子。有研究表明,与独立的血压水平相比,长时BPV在靶器官损害的进展中具有较高的预测价值[33],增大的BPV不仅与心、脑及血管的损害有关,还可能增加心血管事件和死亡的风险[34-35]。STERGIOU等[36]在对BPV变化的研究中发现,HBPM对心血管事件发生的评估价值比诊室血压测量和24 h ABPM更具有实用性。MATSUI等[37]对未使用降压药物高血压病人的研究同样表明,HBPM的BPV增高与心血管损害具有相关性。HOSHIDE等[38]研究也发现,家庭自测血压的日间BPV与心血管病、卒中以及总死亡率的风险有关。
在本研究中,MH组病人的BPV明显增高,而且LVDd、LVPW、LVM、LVMI也较NH组明显升高。相关及回归分析结果显示,MH病人自测SBPV与LVDd、LVM、LVMI呈正相关,是左心室肥厚独立的危险因素。表明MH病人长时BPV明显升高会导致左心室肥厚的发生。
总之,MH是一种常见的高血压状态,具有与SH相似的靶器官损害和心血管危险性,然而,MH病人常因诊室血压正常而不易被识别,临床上易被漏诊,预后差。家庭自测血压可以弥补诊室血压监测的不足,其推广应用有利于及早识别、诊断MH,并进行早期的干预治疗,提高MH的治疗率及控制率,阻止其进展为SH,这对预防MH病人心、脑、肾等靶器官损害,提高其生活质量具有重要意义。
[参考文献]
[1]WILLIAMS B, MANCIA G, SPIERING W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension[J]. Kardiol Pol, 2019,77(2):71-159.
[2]《中国高血压防治指南》修订委员会. 中国高血压防治指南2018年修订版[J]. 心脑血管病防治, 2019,19(1):6-49.
[3]王继光. 2019中国家庭血压监测指南[J]. 诊断学理论与实践, 2019,27(3):258-262.
[4]CUSPIDI C, SALA C, TADIC M, et al. Untreated masked hypertension and subclinical cardiac damage: a systematic review and meta-analysis[J]. American Journal of Hypertension, 2015,28(6):806-813.
[5]CUSPIDI C, FACCHETTI R, QUARTI-TREVANO F, et al. Incident left ventricular hypertrophy in masked hypertension[J]. Hypertension, 2019,74(1):56-62.
[6]SEKOBA NP, KRUGER R, LABUSCHAGNE P, et al. Left ventricular mass independently associates with masked hypertension in young healthy adults: the African-PREDICT study[J]. J Hypertens, 2018,36(8):1689-1696.
[7]SHARMAN J E, HOWES F, HEAD G A, et al. How to measure home blood pressure: recommendations for healthcare professionals and patients[J]. Australian Family Physician, 2016,45(1):31-34.
[8]PARK S, BURANAKITJAROEN P, CHEN C H, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network[J]. Journal of Human Hypertension, 2018,32(4):249-258.
[9]KARIO K, PARK S, BURANAKITJAROEN P, et al. Gui-
dance on home blood pressure monitoring: a statement of the HOPE Asia Network[J]. Journal of Clinical Hypertension (Greenwich, Conn.), 2018,20(3):456-461.
[10]WHELTON P K, CAREY R M, ARONOW W S, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines[J]. Hypertension, 2018,71(6):1269-1324.
[11]MANCIA G, FAGARD R, NARKIEWICZ K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)[J]. European Heart Journal, 2013,34(28):2159-2219.
[12]WANG Y C, SHIMBO D, MUNTNER P, et al. Prevalence of masked hypertension among US adults with nonelevated clinic blood pressure[J]. American Journal of Epidemiology, 2017,185(3):194-202.
[13]ATES I, ALTAY M, KAPLAN M, et al. Relationship between socioeconomic level, and the prevalence of masked hypertension and asymptomatic organ damage[J]. Medical Science Monitor, 2015,21:1022-1030.
[14]OMBONI S, ARISTIZABAL D, DE LA SIERRA A, et al. Hypertension types defined by clinic and ambulatory blood pressure in 14 143 patients referred to hypertension clinics worldwide. Data from the Artemis study[J]. Journal of Hyper-tension, 2016,34(11):2187-2198.
[15]RIZZONI D. Masked hypertension: how to identify and when to treat[J]? High Blood Pressure & Cardiovascular Prevention: the Official Journal of the Italian Society of Hypertension, 2016,23(3):181-186.
[16]TRACHSEL L D, CARLENR F, BRUGGER N, et al. Masked hypertension and cardiac remodeling in middle-aged endurance athletes[J]. J Hypertens, 2015,33(6):1276-1283.
[17]ESEME M, ASIL S, YAVUZ B, et al. Masked hypertension is associated with end organ damage in geriatric age: Geriatric MASked Hypertension and End organ damage (G-MASH-End organ Study)[J]. Blood Press, 2019. doi:10.1080/08037051.2019.1675475.
[18]CACCIOLATI C, HANON O, DUFOUIL C, et al. Categories of hypertension in the elderly and their 1-year evolution: the three-city study[J]. J Hypertens, 2013,31(4):680-689.
[19]MWASONGWE S, MIN Y I, BOOTH J N, et al. Masked hypertension and kidney function decline: the Jackson Heart Study[J]. Journal of Hypertension, 2018,36(7):1524-1532.
[20]SATOH M, ASAYAMA K, KIKUYA M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the ohasama study[J]. Hypertension, 2016,67(1):48-55.
[21]STERGIOU G S, ASAYAMA K, THIJS L, et al. Prognosis of white-coat and masked hypertension: International database of home blood pressure in relation to cardiovascular outcome[J]. Hypertension, 2014,63(4):675-682.
[22]HODGKINSON J, MANT J, MARTIN U, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review[J]. BMJ (Clinical Research ed.), 2011,342:d3621.
[23]SHIMAMOTO K, ANDO K, FUJITA T, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014)[J]. Hypertension Research: Official Journal of the Japanese Society of Hypertension, 2014,37(4):253-390.
[24]CLOUTIER L, DASKALOPOULOU S S, PADWAL R S, et al. A new algorithm for the diagnosis of hypertension in Canada[J]. The Canadian Journal of Cardiology, 2015,31(5):620-630.
[25]MADDEN J M, OFLYNN A M, DOLAN E, et al. Short-term blood pressure variability over 24 h and target organ damage in middle-aged men and women[J]. J Hum Hypertens, 2015,29(12):719-725.
[26]HOCHT C, DEL MAURO J S, BERTERA F M, et al. Drugs affecting blood pressure variability: an update[J]. Current Pharmaceutical Design, 2015,21(6):744-755.
[27]PARATI G, OCHOA J E, LOMBARDI C, et al. Assessment and interpretation of blood pressure variability in a clinical setting[J]. Blood Pressure, 2013,22(6):345-354.
[28]HARA A, TANAKA K, OHKUBO T, et al. Ambulatory versus home versus clinic blood pressure: the association with subclinical cerebrovascular diseases: the Ohasama Study[J]. Hypertension, 2012,59(1):22-28.
[29]STERGIOU G S, NTINERI A, KOLLIAS A A, et al. Blood pressure variability assessed by home measurements: a systematic review[J]. Hypertension Research, 2014,37(6):565-572.
[30]USHIGOME E, FUKUI M, HAMAGUCHI M, et al. Factors affecting variability in home blood pressure in patients with type 2 diabetes: post hoc analysis of a cross-sectional multicenter study[J]. Journal of Human Hypertension, 2014,28(10):594-599.
[31]CACCIOLATI C, TZOURIO C, HANON O. Blood pressure variability in elderly persons with white-coat and masked hypertension compared to those with normotension and sustained hypertension[J]. American Journal of Hypertension, 2013,26(3):367-372.
[32]ROTHWELL P M, HOWARD S C, DOLAN E, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke[J]. Lancet Neurology, 2010,9(5):469-480.
[33]MASUGATA H, SENDA S, MURAO K, et al. Visit-to-visit variability in blood pressure over a 1-year period is a marker of left ventricular diastolic dysfunction in treated hypertensive patients[J]. Hypertension Research: Official Journal of the Japanese Society of Hypertension, 2011,34(7):846-850.
[34]ARASHI H, OGAWA H, YAMAGUCHI J I, et al. Impact of visit-to-visit variability and systolic blood pressure control on subsequent outcomes in hypertensive patients with coronary artery disease (from the HIJ-CREATE substudy)[J]. The American Journal of Cardiology, 2015,116(2):236-242.
[35]DIAZ K M, TANNER RM, FALZON L, et al. Visit-to-visit variability of blood pressure and cardiovascular disease and all-cause mortality: a systematic review and meta-analysis[J]. Hypertension, 2014,64(5):965-982.
[36]STERGIOU G S, NASOTHIMIOU E G. Home monitoring is the optimal method for assessing blood pressure variability[J]. Hypertension Research: Official Journal of the Japanese Society of Hypertension, 2011,34(12):1246-1248.
[37]MATSUI Y, ISHIKAWA J, EGUCHI K, et al. Maximum value of home blood pressure: a novel indicator of target organ damage in hypertension[J]. Hypertension, 2011,57(6):1087-1093.
[38]HOSHIDE S, YANO Y, MIZUNO H, et al. Day-by-day variability of home blood pressure and incident cardiovascular di-
sease in clinical practice: the J-HOP study (Japan morning surge-home blood pressure)[J]. Hypertension, 2018,71(1):177-184.
(本文編辑 马伟平)
[收稿日期]2019-09-07; [修订日期]2020-02-20
[基金项目]国家自然科学基金资助项目(31571829)
[第一作者]邹超斌(1992-),男,硕士研究生。
[通信作者]毛拥军(1964-),男,博士,主任医师,博士生导师。E-mail:mmc168@126.com。
