Analysis of status quo and research progress in nursing care for different typed coronavirus disease 2019:A literature review
2020-06-25BingRuiWEIDianFrancisSAVELLANOCuiHuanHU
Bing-Rui WEI, Dian Francis SAVELLANO,Cui-Huan HU
School of Nursing, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
ABSTRACT
At present, patients with coronavirus disease 2019 (COVID-19) are showing a surge in the world, to explore the clinical characteristics, treatment, and care of different types of COVID-19. The authors reviewed the existing literature, selected,and analyzed the diagnosis and treatment records of 11 patients with COVID-19 who were initially cured, including patient information, clinical manifestations, auxiliary examination results, treatment principles, nursing evaluation,nursing goals, nursing diagnosis, and nursing measures, and found clinical similarities and differences in the care of different types of patients. Among them, nine patients recovered and discharged after receiving treatment, and two died. As there is no speci fic medicine, only symptomatic treatment and supportive treatment can be given. Eleven common nursing measures and special nursing measures of different levels were carried out for patients diagnosed with mild, common, severe, and critical illnesses, and different treatment methods were given according to the severity of signs and symptoms. By summarizing the similarities and differences of clinical nursing interventions, we hope to help improve the quality of care for patients diagnosed with COVID-19.
Keywords: 2019 novel coronavirus, clinical nursing care, nursing intervention, literature review
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus (SARS-CoV-2). At the end of 2019, the first diagnosed person of the disease was located in Wuhan City, Hubei Province, Mainland China, and has since spread worldwide.[1]Till May 23, 2020, it has now spread to more than 210 countries and regions and has caused 4,993,470 confirmed cases and 327,738 deaths, reported to the WHO.[2]The cure of patients depends on supportive treatment and symptomatic care. However, only a few studies have explored the similarities and differences in the clinical care of patients with different types of COVID-19. In this article, we review the care of 11 patients with different typed COVID-19 and provide the reference for interventional research on nursing care of COVID-19.
Classi fication and characteristics of coronavirus disease 2019
The clinical type classification of COVID-19 can be divided into mild, common, severe, and critical, according to the Diagnosis and Treatment Protocol for COVID-19 (Trial Version 7) issued by the National Health Commission of China.[3]Mild patients did not have symptoms of pneumonia, and the prevalence was about 81%. Approximately 14% of the patients were developed into severe type, who had the following manifestations:dyspnea, shortness of breath (respiratory rate ≥30 breaths/min), hypoxemia (blood oxygen saturation [SpO2] ≤93% at rest), etc., Involvement and symptoms of different organs are the main consequences in critical COVID-19 patients,including respiratory failure, septic shock, or multiple organ failure, accounting for 5%.[4,5]Although mild patients account for the majority of cases, the mortality rate of critically ill patients is extremely high, close to 50%.[6]Due to various factors, for example, severely ill patients are mainly elderly people over 50 years old, this group of people mostly have basic diseases such as cardiovascular and cerebrovascular diseases, and the COVID-19 not only attacks the lungs but also attacks many organs such as the heart, kidneys, and intestines, causing multiple organ failure.[7]According to the statistics of clinical data, the kidney injury rate is 15%, and 20% of critically ill patients have heart injury.[7]These factors make the condition of critically ill patients change very quickly and the mortality rate is high.[8]Therefore, nursing care to prevent the conversion of mild to severe and critical illness, as well as nursing to treat critical illness, has received much attention.
MEDICAL RECORDS
In this study, a total of five English case reports and six Chinese case reports were included in the study, as well as other referred literature published. According to the statistics, the clinical characteristics, treatment, and nursing measures of the patients with different clinical types of COVID-19 are shown in Table 1.
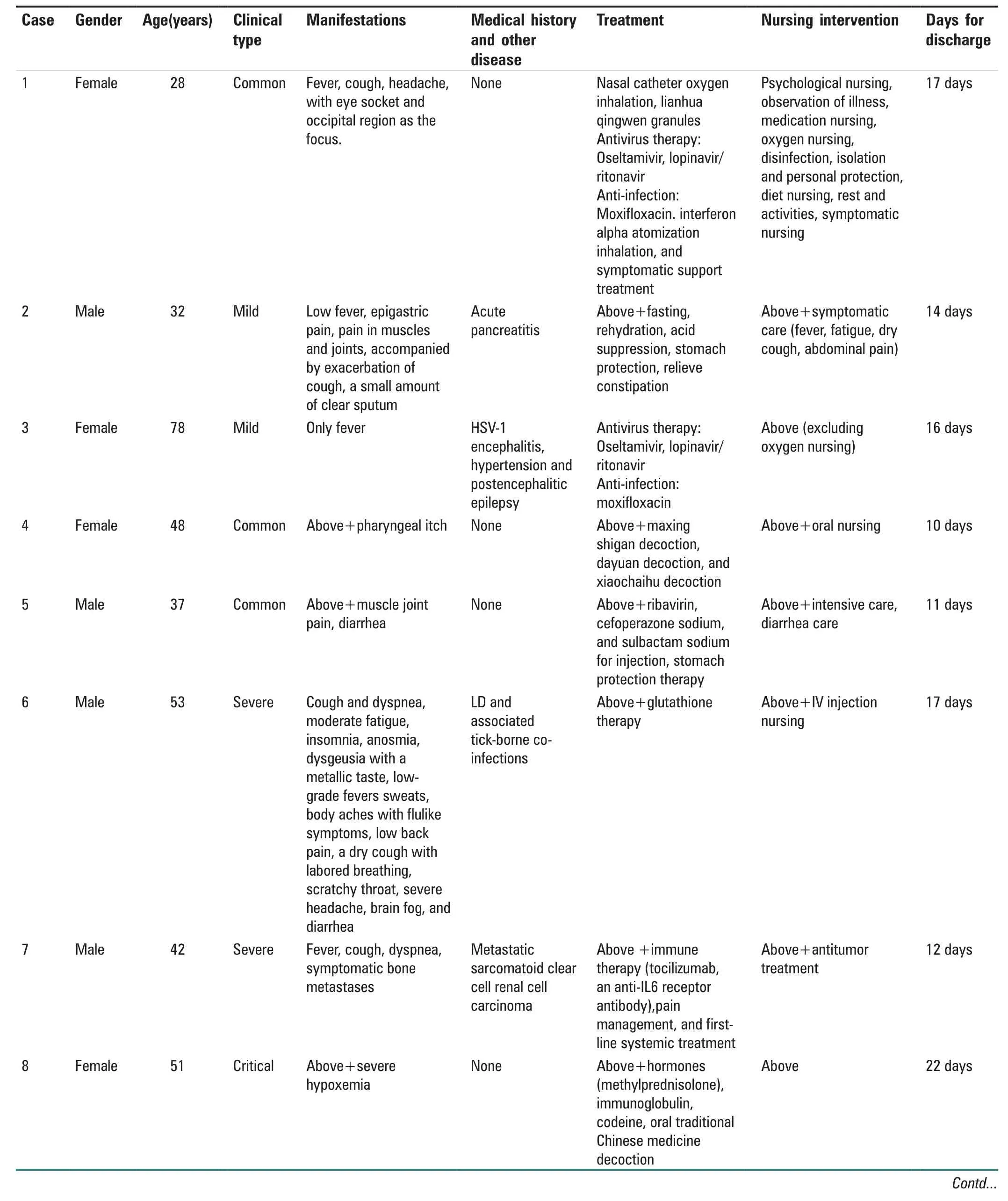
Table 1: The detail information of 11 cases
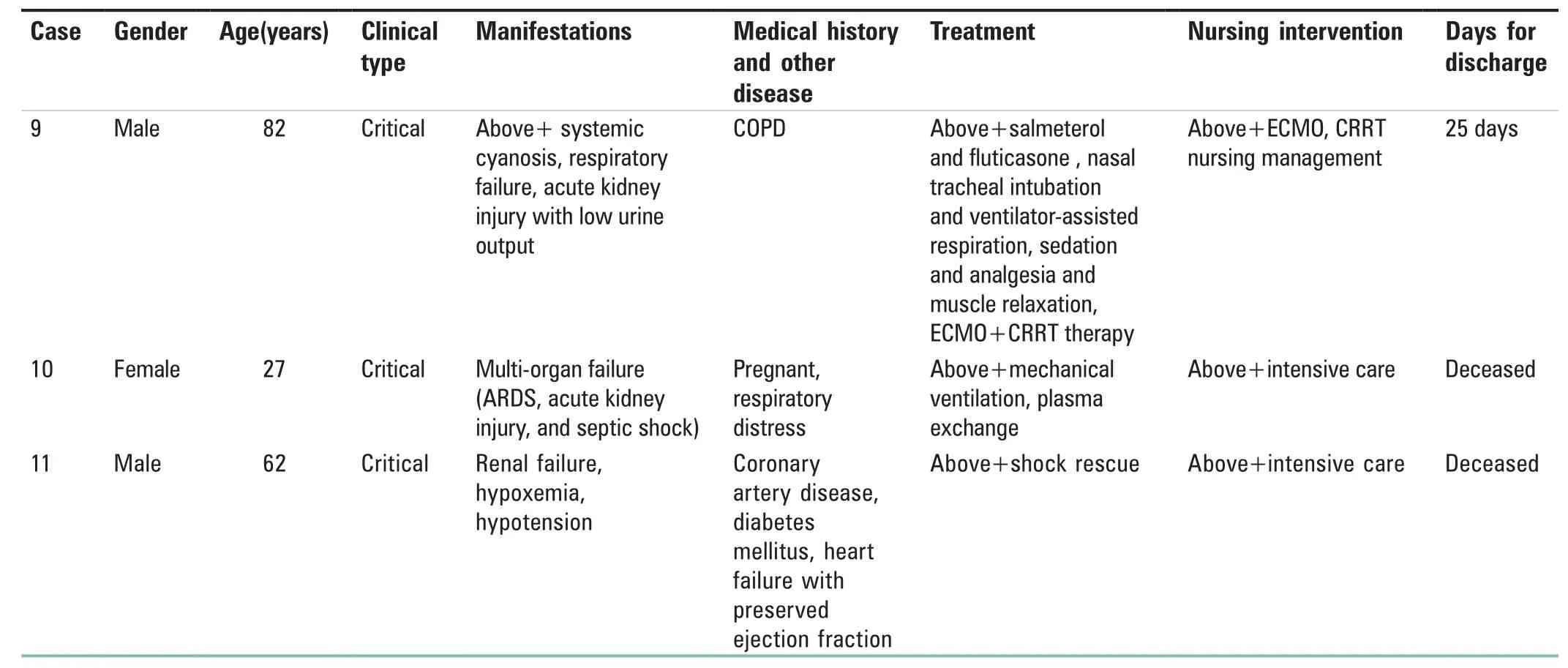
Table 1: Contd...
DISCUSSION
To date, there are no vaccines and any specific antiviral medicines to prevent or treat COVID-19. Those affected were given care to relieve symptoms; symptomatic treatment was provided for mild patients; supportive treatment was provided for critically ill patients; and most patients recovered because of supportive care.[9]To prevent the progress of the virus and to reduce the mortality rate, we searched a large number of COVID-19–related case reports in China and abroad and then conducted a statistical analysis to have a better understanding of the similarities and differences in treatment and care of patients diagnosed with COVID-19.
Nursing assessment Health history
Just like any other patients diagnosed with a disease, nurses obtain all necessary data from the patient, including from patient’s name, age, sex, eating habit, living environment,any previous medical history, to treatment history of other diseases. Since COVID-19 is a pandemic case, we also needed to ask questions on how and where the patient possibly acquired the disease – we ask the patients’ travel history and if the patient had any contact with other people diagnosed of COVID-19.
Physical condition
Nurses assess the patient’s vital signs (body temperature,blood pressure, pulse, respiratory rate) and SpO2and then assess the patient’s signs and symptoms, such as cough,sputum, fatigue, shortness of breath, diarrhea, and confirm if there are any signs of dehydration and electrolyte imbalance.Analysis of the blood includes blood leukocytes, lymphocytes,C-reactive protein, etc.
Psychosocial situation
It is necessary to assess the patient’s knowledge about the disease and health, current mental and emotional state,perception and recognition ability, the patient’s response to pressure and emotions about COVID-19, their views on their current status and self-image concept, etc.
Nursing diagnosis
1. Impaired gas exchange: related to hypoxemia
2. Ineffective airway clearance: related to fatigue and increased secretion
3. Hyperthermia: related to thermoregulation disorder
4. Diarrhea: related to the effect of COVID-19 on intestinal tract and intestinal dysfunction caused by infection
5. Changes in comfort level: related to chest tightness,shortness of breath, fatigue, etc.
6. Altered nutrition: Less than body requirements: related to fever, diarrhea, and reduced intake
7. Risk for impaired tissue integrity: related to high fever,moist skin, and due to long periods of bed rest
8. Risk for activity intolerance: related to poor peripheral circulation and respiratory dysfunction
9. Knowledge deficit: related to effective isolation and personal protection of COVID-19.
Common nursing interventions to promote coronavirus disease 2019 patients’ recovery Ward environment management
Disinfection is strictly enhanced. 1000 mg/L chlorine-containing disinfectant or 75% alcohol is used to disinfect objects and the floor. If no one is around,[10]the air is also disinfected.The patient eats alone and was instructed to use disposable tableware. If the patient needs to use reusable wares, it is advised that the utensils must be disinfected using boiling water for at least 15–30 min.
Proper hygiene is also promoted. The patient is advised to be hospitalized with bathroom privileges. Frequent hand washing is advised; in addition, hot baths are suggested to promote blood circulation. The patient was advised to keep a distance of at least 1 m and to wear a mask when talking.The mask and the distance are important since the virus can be airborne and can be transmitted through droplets.
Transmission of the COVID-19 virus through droplets is proven, while through air and digestive wastes such as feces and urine are yet to be determined.[11]Although it has been reported that there are traces of COVID-19 detected in some feces,[12]there is no definite evidence of fecal–oral transmission. Nevertheless, fecal matter and other wastes must be handled accordingly.
Nurses instruct patients to maintain good personal hygiene habits, instruct patients to wash their hands frequently, and instruct patients to cover toilet seats before flushing to ensure the cleanliness of the ward.
Wards are divided into different areas depending upon the severity of the case. Patients with different levels of illness are managed separately.[13]To maintain fresh air in the ward,the windows are left open for at least 2 or 3 times a day for around 30 min each time.[14]The patient’s room is kept clean and tidy, the warmers are turned on for a while to keep the room warm, but the central air-conditioning system is not used since it will only promote transmission of the disease.With a temperature of 25°C and a humidity of 50%–60%, the patient felt comfortable.
Life management
A quiet environment was kept to promote rest and recovery.[14]Sufficient sleep and rest can reduce oxygen consumption and relieve signs and symptoms of hypoxia, thus promoting faster recovery. Reduced activity will promote further healing of the damaged tissues. However, minimal movement can promote blood circulation that can supply oxygen to affected areas,thus avoiding development of ulcer and bed sores. Critically ill patients are at risk of falls and injury, so the bed bar should be pulled up to prevent accidental injury. Nurses should also assess any development of venous thrombosis of the lower extremities of the patients lying on the bed for a long time. If the patient is ambulatory, the patient can do simple exercises to promote blood circulation.[15]
Patients can choose reasonable body positions. For example,patients receiving common oxygen administration will be placed in semi-lying position, patients suffering from shock and circulatory instability will be placed in supine position,the head of bed will be raised, the end of the bed will be raised, and when necessary, patients will be placed in prone position according to doctor’s advice to promote venous return and ventilation.[16-18]
For some critically ill patients lacking help from their families due to weakness and isolation, nurses should give attention to oral care and skin care in their daily care. Oral care is assisted by a medical staff 2–3 times a day. Nurses should prevent secretions from splashing when implementing oral care, and the staff should wear a three-level protection when necessary.[16]
For some critically ill patients assisted by tubes, nurses should pay attention to the characteristics, quantity, color, and characteristics of the excretions to judge whether they need to be changed. When the tubes are in use, it is recommended that these tubes are tightly connected and fixed and has no obstructions. In addition to proper use of the tubes, nurses must also keep in mind the use of aseptic technique during the process to prevent secondary infection from the current disease.[18]
Some studies have pointed out that early lung rehabilitation can enhance muscle strength, relieve dyspnea, and improve body motor function, thus shortening hospitalization.[19]The nurse can train the patient to do some breathing exercises,for example, a simple breathing exercises; let the patient inhale air and then instruct the patient to slowly exhale for 2–3 s. Nurses can also teach the patient to follow the traditional “Six-Word Qigong;” i.e., the patient will say the syllables “Xu, Ha, Hu, Yan, Chui, and Xi” accompanied by inhaling and exhaling; this method is also an effective way in teaching breathing exercises.[20,21]On top of breathing exercises, the use of tools such as spirometer can be used as an aid. Breathing exercises can also prevent atelectasis and improve the patients’ breathing.
Medical nursing
COVID-19 is spread through droplets; as of now, this is the only confirmed method of transmission of the disease.[3]To protect the staff from getting infected, strict isolation of the patients and wearing of personal protective equipment are implemented. Due to these changes, operating procedures within the hospital or ward is also affected up to a certain degree; therefore, the healthcare team needed to improve the system. To make improvements, to prevent errors and cross infection, and to provide high-quality care for the patients,strict patient triage, timely shift of the nursing staff, and accurate implementation as per doctor's adivce are taken in the hospitals.[22]When dispensing medicines, nurses are advised to make preparation at a certain time and place to prevent drugs from unnecessary contamination.
At present, there are no specific drugs that can treat COVID-19, so the treatment measures are symptomatic and supportive treatment,[23]including antibiotics, antiviral drugs,hormones, immunity boosters, and other drugs.[24]Drugs such as oseltamivir, lopinavir, and ritonavir for antivirus and ceftriaxone as an antibacterial drug are given to patients as per doctor’s advice. To improve the prognosis of patients,Chinese and western medicine are combined.[25,26]Not only can medicines cure the disease, but also it cause side effects:oseltamivir possibly causes nausea, diarrhea, cough, and other adverse reactions; lopinavir/ritonavir possibly causes diarrhea and other bowel discomfort; interferon possibly causes flu-like symptoms such as headache, tiredness,and weakness. Since patients receive a handful of drugs,it is necessary and important to identify any adverse reactions.[27]Nurses should be responsible in taking extra steps in identifying any possible undesired outcomes from drugs; monitoring the patient’s vital signs and any kind of discomfort are just a few steps in recognizing adverse reactions. Closely monitoring the patients’ overall status not only tells unwanted reaction from drugs but also monitors the patients total health condition if it is improving or not.Drug interaction must also be explained to the patient for better understanding of the drugs and is advised to report any discomfort. For drugs that are given intravenously,the puncture site must have been checked for any signs of swelling and leaks every time when a nurse gives medicine.Hydrocolloid dressing is suggested to prevent phlebitis and to ensure smooth venous access.[24]Intravenous drip should not be too fast, 30–40 drops per minute. Due to the potency and the number of drugs taken by the patient, oral bicyclic tablets were prescribed to promote liver health and the patient’s liver and kidney functions were regularly tested.[28]Alpha-interferon inhalation was also prescribed; it will be administered through nebulizers. Nebulizers may generate mist that can pollute the indoor air and a possibility to spread the virus; to avoid the spread of the disease, it is important to maintain isolation during nebulization. If necessary, the combination of a fixed dose inhalation device and a mist storage tank is preferred.[18,29]The patient was taught how to properly inhale the mist during the procedure for efficiency.Immediately after the treatment, the patient’s facial skin was cleaned to keep the integrity of the skin.[30]
Psychological assessment and support
When the patient is admitted in the hospital, a trusting relationship between the staff and the patient must be established.[22,27]To do this, the nurse should explain the structure of the isolation ward, the division of areas, and the equipment and facilities in the room and explain that when a facility or an equipment is in use, only one person can use it at a time. These explanations are necessary so that let the patients know the scope of their activities, help them to get familiar with the environment, and know that the isolation measures are safe and reliable, thus giving reassurance to them and eliminating their possible doubts,[24]enabling them to obtain the support source of emotional stability and security during hospitalization.[22]To gain the further understanding and trust of patients, the nurse should explain to the patient any relevant information about COVID-19 infection and the importance of wearing masks and other protective gears and why the staff should also wear their personal protective equipment.[24]
COVID-19 is a new disease that is infectious and has no cure as of this time; this leads to anxiety and fear of patients and can result to lose confidence in the treatment. Some studies suggest that effective psychological counseling can promote the recovery of patients, improve the efficiency of the treatment,and promote positive desired outcome by improving the confidence of the patients.[22,31]Boosting ones' confidence is also vital, especially to patients who are receiving treatment in the intensive care unit, as confidence plays an important role in the prognosis and treatment of the patients.[32]
In the process of treatment, nurses should observe and listen to the needs of patients, observe and evaluate the psychological state of patients in time, and carry out psychological guidance; these assessments are also important to reduce the psychological pressure of patients and enhance comfort of the patients.[27,33]Treating patients without bias and to answer their questions patiently, communicating their progress of treatment,[22]establishing a good professional relationship with the patients, care for patients more, and to satisfy their sense of belongingness[24,27]are also a few extra steps to offer when confronting patients suffering from the virus. Not only do we have to educate the process, but we also have to teach the family members of the treatment, signs and symptoms, and transmission of COVID-19; knowledge regarding the pandemic can gain the cooperation and understanding of the family members and the patient.[34]
There are also a few more psychological problems that need to be tackled. Some patients feel guilty that they brought this disease into their family, and on top of that,they worried if they can keep their current job.[26,35]And because they are isolated in single rooms for a long time,without family members to accompany them, they are not only worried about their illness but also feel lonely.Therefore nurses should guide them to communicate with their families through video chat and other possible means to obtain family support. If possible, patients are encouraged to listen to music to relax their mood and watch videos to distract their attention.[22,36]For a small number of patients not cooperating with the medical staff due to fear of disease, even showing anger, aggression, abandonment of treatment, and other extreme behaviors,[37]nurses can give them corresponding psychological intervention measures,including listening and understanding, moderate empathy to stabilize patients’ emotions, even psychological health education or hotline assistance, and consultation and drug intervention if necessary.[19]
It is reported that whenever a patient’s condition worsens,it can lead to psychological pressure, thus triggers fear and delirium and difficulty in managing with the treatment. Due to lack of medical knowledge and extreme fear, patients force themselves not to sleep to prevent them from falling asleep and never waking up. They are in a state of psychological crisis, which seriously affects the patients’ ability to cope with the disease. Not enough sleep and confidence to recover are not conducive to the patient’s condition.[24]To control the situation, nurses who are capable and experienced in doing psychological consultation arrange treatment plan to answer the psychological needs of patients. These experienced nurses will try to relieve the stress of the patients and in turn promote a healthy sleeping pattern.[38]
There are also cases that a patient accidentally urinates, or stress urinary incontinence (SUI), which occurs when urine leaks out of the bladder due to an increased abdominal pressure. SUI can psychologically affect the confidence of patients, resulting to a strong sense of inferiority.[26]To solve this, nurses must educate the patient on how to effectively and efficiently cough out sputum and remind the patient to urinate time to time. Teaching Kegel exercise is an effective method to control SUI. Since the patients’ confidence is also affected,nurses must also help them by telling encouraging words that they can get better by cooperating with the treatment plan. By teaching effective coughing and Kegel exercise and by giving words of encouragement, SUI can be relieved.[39]
Oxygen nursing management
Those infected by the virus can only receive care to relieve symptoms, symptomatic treatment was provided for mild patients, supportive treatment was provided for critically ill patients, and most patients recover because of supportive care.[9]Dyspnea and hypoxemia are the common causes of death related to COVID-19.[40]
Oxygen should be administered as per doctor’s advice if the patient suffers from dyspnea, shortness of breath, and any signs of respiratory distress and hypoxemia.[33]Oxygen therapy measures include nasal catheter, mask oxygen supply, and nasal high-flow oxygen therapy.[41]Patients using nasal catheter oxygen inhalation or nasal high-flow oxygen therapy should wear a surgical mask or mask to reduce the spread of the virus in the air.[18]Whether the patient’s pulse,blood pressure, mental state, and skin color have improved is observed, while oxygen support is still administered, with the concentration adjusted as per doctor’s advice.
For continuous nasal catheter oxygen administration, to prevent infection, the nasal catheter needs to be replaced twice a day. Nasal secretions are cleaned in a timely manner to prevent any obstruction.[42]
For critically ill patients who use ventilator and prone position ventilation, the most important thing is to prevent ventilator-associated pneumonia. Nursing staff should pay attention to aseptic technique when operating the device and regularly disinfect and sterilize the pipeline. Regularly check the patency of the respiratory tract and artificial airway,perform sputum suction as required by the patient, and remove airway mucus secretions. If a patient has the ability to take care of himself/herself, the nurse instructs him/her to know how to effectively and efficiently cough out the sputum. Secretions are thought to be disposed properly to avoid further transmission of the virus.[18]
Hyperthermia treatment
Fever is a typical symptom of COVID-19.[3]Body temperature is an important vital sign and tells us if the patient is getting better,[26]so closely monitoring the temperature of patients is a basic task for nurses. When the temperature of patients is ≤38.5°C, it is measured once every 4 h; if it is >39°C, it will be measured once every 2 h. Patients with excessive sweating should replace soiled bed sheets and clothes in time to prevent catching colds and consider it as an infectious object to prevent the transmission of the virus.[43]Sweating may lead to hypovolemic shock due to excessive fluid loss;therefore, nurses should pay attention to changes in intake and output volume. Increased fluid intake is encouraged to prevent dehydration, electrolyte imbalance, and poor skin integrity, which are caused by hyperthermia. Because of dehydration related to hyperthermia, the oral cavity of the patient becomes dry, and it is suggested to do oral care as this is susceptible to the virus. Nurses should instruct food which is high in calorie, protein, and vitamin, low in fat, light,and easy to digest.[24]After the patient cools down and his/her body temperature is normal, the body temperature shall be measured every 4 h, and the changes of the patient’s body temperature should be closely monitored to provide basis for diagnosis and treatment.[26]
Management of diarrhea
A case report mentioned that patients suffered from mild diarrhea after oral administration of antiviral drugs and traditional Chinese medicines. Montmorillonite powder and Bifico are given as per doctor’s advice; these medicines can maintain intestinal homeostasis while relieving diarrhea and prevent further infection.[26]
When the patient continuously experience diarrhea, the nurse closely observe the amount, color, quantity, and character of the stool; take stool samples; and give antidiarrheal medicines.[24]On top of giving medicines, the nurse should also record a 24-h fluid intake and output,monitor electrolyte imbalance, and look out for any signs of hypokalemia and hyponatremia.[44]
It is important to observe patient’s appetite and food intake and to advice rehydration to prevent dehydration. To avoid dehydration, oral rehydration salts should be given.Semi-liquid food with low residue, low fat, and low cellulose and easy-to-digest liquid food are given to patients. Raw and cold food can further upset the stomach; hence, it should be avoided. If needed, the patient’s abdomen was kept warm by hot compress to relieve abdominal pain due to diarrhea.Because of frequent defecation that can lead to impaired perianal skin, gentle wiping of the anus with soft tissue paper and cleaning the perianal area with warm water after defecation are suggested.
Nutrition management
When a patient is ill, the body uses a large amount of nutrition to heal; therefore, the nutrition of the patient plays a vital role. Nutrition of the patient should be adequate and be supplemented.[45]Patients are given a high-calorie,high-protein, and high-vitamin diet and none spicy,stimulating food.[46]Appropriate addition of meat, poultry,soybeans, fish, nonstarch vegetables, and other food rich in ketone was given to enhance the body’s immunity. Hot soup is advised to relieve inflammation of the airway. Food rich in Vitamin C, such as vegetables and fruits, especially tomatoes,apples, and oranges, is suggested; Vitamin C tablets and zinc oral tablets are also suggested. High fluid intake was advised to dilute sputum and to correct the lost fluid during episodes of hyperthermia.
Vital signs monitoring and nursing
The vital signs of the patient such as body temperature,depth and rhythm of breathing, and SpO2were closely monitored. The medical team also pays attention to the patient’s consciousness, episodes of cough and its discharges,any signs of chest tightness, dyspnea, and cyanosis. Blood routine examinations, urine examinations, C-reactive protein,biochemical index (liver enzyme, myocardial enzyme, renal function, etc.), coagulation function, arterial blood gas analysis, and chest imaging are monitored according to prognosis of the condition.[45]
Nurses need to closely monitor the changes of vital signs,especially body temperature, respiration, and blood pressure.[27]Nurses need to record the vital signs of the patient every 4 h (or otherwise as per doctor’s advice), as well as the consciousness, heart rate/rhythm, respiration,SpO2, blood pressure, and urine volume. Nurses need to summarize the intake and output volume once every 4 h.Meanwhile, nurses need to observe the color, nature, stool frequency, nature, and volume of the patient’s urine and to make records. If the patient has cough, the sputum’s color,quantity, and other characteristics must be monitored; nurses should observe if the patient is also getting better throughout the treatment.[24]Nurses should also check for any electrolyte imbalance; changes on the treatment plan must be made accordingly if there are any abnormal deviations.[19]
Dyspnea is a common symptom of COVID-19; when monitoring the respiratory system of patients, it is necessary to observe any abnormal changes of patients’ respiratory depth frequency and any changes of the patients’ SpO2.SpO2tells us the concentration of the oxygen in the blood;99% SpO2must be maintained.[22]When the SpO2is more than 98%, the patient is given continuous low-flow oxygen inhalation for 2 L/min. When the SpO2is 95%–98%, nurses need to adjust the oxygen flow to 3 L/min and closely observe whether the SpO2increases. If there are no improvements,the arterial blood gas needs to be rechecked. When the SpO2 is < 94%, nurses need to check if the patient is experiencing chest tightness, wheezing, abnormal breathing frequency,and rhythm; if so, it is advice to adjust the oxygen flow to 5 L/min and immediately notify the doctor.
According to reports, 23.4% of the critically ill patients are at high risk to have cardiovascular attacks; if needed,electrocardiographic (ECG) monitors must be provided to monitor the condition of the heart. Central venous pressure (CVP), blood pressure, and heart rate must be monitored every 2 h, unless required otherwise. If there are any signs of shock and hypotension, nurses need to immediately notify the doctor and implement treatment measures.[19,22]
In some case reports, COVID-19 also affects the digestive tract; it can cause diarrhea, abdominal pain, poor appetite,and other gastrointestinal symptoms.[47]Any occurrence of any gastrointestinal problems must be reported including time, location, nature, and remission and if the medication is effective. In case of vomiting, the patient should lie on his/her side to prevent aspiration and asphyxia. The character,color, and quantity of the vomit must be recorded and notify the doctor in time.[22]
There are reported cases of hormonal imbalance, possibly due to the medications that the patients take. There is a case that the patient incurred high levels of glucose, but the patient does not have any history of diabetes; it is advised for the patient to have a more accurate test than the usual glucometer. Hormones can definitely affect the patients’ homeostasis; it can affect the blood sugar, can cause constipation and diarrhea, and affect the patients’ mood and comfort. Nurses can tackle hormonal changes by promoting a balanced diet, by promoting a rest and relaxing environment,and if needed, by giving medicines as per doctors’ advice.[26,48]
Patients with immunocompromised diseases, with chronic diseases, and with old age are more susceptible of contracting the disease. Mortality rate is high if the disease is not managed at the beginning. Preventing and detecting any complications at the onset of this virus, giving medical care at a timely manner, and implementing proper care will increase the chances of survival.[49]
Body pain is also a symptom of 2019-nCoV; it is important that this should not be overlooked at. Pain medications as per doctor’s advice can be given; promoting relaxation, deep breathing exercise, and other means of distraction can be promoted to minimize pain.[45]
Infection protection and management
During hospitalization, patients are required to wear a mask.Strict isolation was promoted and visitation is prohibited.All wastes are instructed to be disposed of properly. The patient’s respiratory secretions and blood samples that were collected are properly disposed of using a three-level protection technique.[50]The collected respiratory secretions,feces and urine, and vomit of the patient were managed separately; these wastes are not exposed and transferred by proper personnel. These wastes are treated as medical wastes and handled strictly with double-layer packaging, and the outside of the packaging is clearly marked, sealed, and disposed of. Proper sterile techniques are strictly followed.
Health education and discharge instruction
There are several conditions that a patient must meet before discharge. First, the patient’s body temperature must continuously be normal for at least the past 3 days. Second,the respiratory system should show big improvements – less coughs and sputum, no signs of wheezing, and no crackles upon auscultation. Third, computed tomographic scan of the lungs must show that the lesions made positive progress.Fourth, two consecutive negative results on a COVID-19 nucleic acid test from respiratory tract specimens were obtained (samples must be taken after every 48 h).[51]
After discharge, the patient is recommended to be quarantined in a designated observation facility for self-health monitoring for 14 days. During isolation, it is essential for patients to wear a mask, live in a single, well-ventilated room, reduce close contact with the family, eat meals alone,maintain good hand hygiene, and avoid going out. Patients can exercise, but adequate sleep and rest should be ensured;they can have reasonable diet and a stable mood. The patient is instructed to come back for a follow-up checkup at the 2ndand 4thweek after the discharge.[51]
Nursing of special treatment Circulation support – Extracorporeal membrane oxygenation care
Extracorporeal membrane oxygenation (ECMO) can partially or completely replace the cardiopulmonary function of patients for a long period of time; it can maintain the blood oxygen supply and provide short-term or long-term cardiopulmonary support. It is generally used for patients whose lungs cannot provide sufficient oxygen even when they have supplementary oxygen, when the lungs cannot remove excessive carbon dioxide even with the help of a mechanical ventilator, or if the heart cannot pump enough blood.
It is advised that two nurses take care of a patient who is using ECMO; these nurses timely evaluate and cooperate with the doctors to take feasible measures in assisting any abnormal findings. Nurses are responsible for monitoring any ECG changes, monitoring the blood pressure and mean arterial pressure – making sure that the pressure is above 60 mmHg – and monitoring the CVP.[34]
Since systemic heparinization is required during ECMO, and heparin is continuously infused through the ECMO system,the activated clotting time (ACT) should be monitored every hour to understand the heparinization. It is advised to maintain ACT between 140 and 180 s. Thrombosis and embolism may occur if ACT is insufficient. The patient’s SpO2, urine volume, liquid intake, and output volume need to be continuously monitored, and spot checks are made every hour. After blood is drawn for blood gas examination,the puncture site needs to be pressed for not less than 15 min because of the heparin. To keep the patient under anesthesia, all the time during ECMO, sedatives, analgesics,and muscle relaxants are administered to give the patient’s lungs sufficient rest and to ensure that the patient receives effective treatment. The patient is intubated and assisted by a ventilator; therefore, nurses must make sure that proper care is given. If there is an emergency, the doctor must be notified immediately.
Common complications include hemorrhage, embolism,and infection. As ECMO is performed on an extracorporeal machine, air embolism is a problem that nurses must prevent.Before the machine is put into operation, the pipelines shall be strictly inspected to remove air, and tightly connected without air leaks and disconnections during the use of ECMO machine. The patient must be assessed of his/her consciousness, vital signs, and any signs of thromboembolism every hour.
COVID-19 is a very contagious virus, and ECMO is an invasive procedure that increases the rate of transmission.Therefore, medical staff should strictly observe the principles of hand hygiene and sterile techniques and respiratory care (preventing occurrence of ventilator-associated pneumonia), administer antibiotics in a timely manner, and follow doctor’s advice.
Blood puri fication therapy – Continuous renal replacement therapy nursing management
A clinical analysis[52]found out that there may be extensive renal damage in patients infected with COVID-19. Among 51 patients, proteinuria was found in 32 patients, accounting for 63%. A research group of Suzhou hospital affiliated to Nanjing Medical University, suggested that COVID-19 may cause kidney damage. The results show that about 3%–10% of patients infected with the COVID-19 have abnormal renal function, including the increase of creatinine or urea nitrogen.Accordingly, experts suggest that kidneys must be protected as soon as a patient is diagnosed of COVID-19.[53]
Continuous renal replacement therapy (CRRT) refers to a group of therapeutic techniques for extracorporeal blood purification. According to the diameter size of the solute particles in the solution, harmful substances can be filtered out through dialysis, thereby adjusting and maintaining the water, electrolyte and acid-base balance in the blood.In CRRT treatment for patients with COVID-19, the water content in the blood plasma and the solute with small and medium molecular weight dissolved in the blood plasma are removed by convection. At the same time, substances required by the body are delivered into the body in the form of fluid replacement to maintain homeostasis.[54]During CRRT treatment, nurses should closely monitor vital signs, heart rate, blood pressure, respiration, SpO2, and CVP; accurately record the amount of liquid in and out per hour; discover and deal with various abnormal situations in time; and observe the positive desired outcomes.
Nurses should closely observe the color of blood in the filter and pay attention to leaks. Before the CRRT is used, the device must be checked. When preparing the replacement fluid, potassium, sodium, calcium, magnesium, and other electrolytes must be added as per doctor’s advice. During the treatment, the coagulation function and blood gas analysis must be checked every 2–4 h according to the doctor’s advice, and any abnormal findings must be reported in time.Electrolyte, creatinine, and urea nitrogen must be checked daily. Depending on the test results, the replacement liquid can be modified to ensure that homeostasis is achieved.
The speed of filtration and the administration of replacement fluids must be closely monitored: input and output exchange is very important for this process. If the filtration volume exceeds the intake volume, it will cause hypovolemia and hypotension; inadequate filtration volume can cause hypervolemia and hypertension; hence, any signs of abnormal homeostasis of fluids must be dealt with accordingly.
Common complications include hemorrhage, coagulation,and infection. Bleeding should be detected as early as possible; the use of anticoagulant should be adjusted in time or heparin-free machines should be used; protamine should be used to neutralize the anticoagulant effect of heparin when necessary. However, if the patient has little or no heparin and the treatment time is long, extracorporeal coagulation will easily occur. Before the use of CRRT, the filter and tubes must be soaked in heparin-saline solution.
If the color of the blood in the pipeline darkens, the temperature drops, and the filtration volume decreases significantly, indicating that coagulation is imminent or has occurred, then the process must be stopped immediately.The filtration device should be flushed with heparin-saline solution, and the causes of the coagulation must be checked. If the blood coagulation cannot be removed by the heparin-saline solution, then the filter should be replaced.Due to the critical condition and low resistance of patients,various invasive tests and treatments are easy to cause infection. Aseptic principle should be strictly implemented when carrying out various nursing technical operations;sterile technique plays an important role to reduce the rate of transmission and recurrence.
Nursing care of deep vein catheterization is important to prevent nosocomial infections. If a urinary catheter is present,nurses should keep it clean to prevent urinary tract infections.
Immunotherapy – Nursing care of tocilzumab therapy
Chinese scientists have found that in the treatment of COVID-19, the cytokine storm, namely cytokine release syndrome, in which the level of interleukin-6 is increased during the treatment of severe and critical cases; this gene is one of the reasons why COVID-19 turns out to be dangerous and lethal.[55]There are data that suggest that this treatment scheme can prevent the worsening of the situation by blocking cytokine storms and improve the prognosis of patients.[56]Tocilizumab has become a new treatment method for severe and critical cases of COVID-19. It has been included in the “COVID-19 Diagnosis and Treatment Plan (Trial 7thEdition).” This is also the first time that immunotherapy is used as a treatment method for severe and critical cases of COVID-19.[57]
The application of tocilizumab needs to be evaluated. In general, tocilizumab is not needed for patients diagnosed for a mild case. As for patients diagnosed with severe COVID-19,if there are any other existing infections, and tocilizumab will be used to inhibit the inflammatory reaction, the patient’s own resistance will also be weakened, which may further aggravate the infections. Due to this reason, before a patient is given tocilizumab, he/she must undergo rigorous checks to avoid complications.[58]
Because tocilizumab is sensitive, it should be stored in a cool dry place at 2°C–8°C and away from light. Nurses need to check whether the liquid has developed any granules or any change in color before its preparation. Only when the liquid medicine is clear to semitransparent, is colorless to light yellow, and has no visible particles, then it can be used. Like any other drugs, nurses must do a skin test before administering the drug. When skin test shows negative, this drug must be given intravenously with 100 mL of normal saline solution through a piggyback intravenous set at a rate of 20–30 g TT/min running for 1 h. Once the drug is administered, the tubes must be flushed with 0.9% normal saline solution,
In any circumstances that the drug should be used later, it can be stored in a cool place at 2°C–8°C for no more than 24 h.The common adverse reactions of tocilizumab are urinary infection, itching, sinus pain, sore throat, headache and dizziness, and mild stomach cramps. It is important to check if there are any signs of anaphylaxis and hypersensitivity to the drug; if there are any, the process must be stopped and the doctor must be notified right away.[59]
CONCLUSION
In this review of literature, we can agree that nurses play a big role in fighting COVID-19. Most of the cases turned out for the better, proving that the skills of nurses are important in managing and preventing the virus and in treating patients diagnosed off COVID-19. Nurses have professional responsibilities to constantly think, research,analyze, and discuss the quality of care given to patients and how to improve nursing. While we still need to know more about the virus, people in the older age group, people with pre-existing medical conditions such as diabetes and heart diseases, and immunocompromised patients are also required more attention in clinical nursing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Con flicts of interest
There are no conflicts of interest.
杂志排行
Journal of Integrative Nursing的其它文章
- Construction of nursing standard of integrated traditional Chinese and Western medicine for patients with COVID-19 (mild and common) in Beijing based on Delphi method
- Assessing the reasons for increase in self-medication and control measures among student nurses in University of Benin Teaching Hospital, Edo State, Nigeria
- Anxiety and perception among nurses toward the outbreak of COVID-19 in University of Uyo Teaching Hospital, Akwa Ibom State
- The impact of sleep quality on reported anxiety and fatigue among shift nurses: The mediating role of resilience
- An innovative approach of using online problem-based learning and case-based learning in teaching disaster nursing during the COVID-19 pandemic
- Effect of mild moxibustion in improving the quality of life of patients with diabetic peripheral neuropathy
