The psychological status investigation on the nursing staffin a 3A‑level hospital during the prevalence of COVlD‑19 and the analysis of its influencing factors
2020-06-22HaiXiaCHENJuHongPEIXingLeiWANGRuiLingNANXinManDOU
Hai‑Xia CHEN, Ju‑Hong PEI, Xing‑Lei WANG,Rui‑Ling NAN, Xin‑Man DOU,4
1School of Nursing, Lanzhou University, Lanzhou, Gansu,
China; 2Department of Liver Diseases; 3Department of EICU;4Department of Nursing, Lanzhou University Second Hospital,Lanzhou, Gansu, China
ABSTRACT
Objective: The objective of the study is to investigate the psychological status of nursing staff both working on nonfront line and on the front line during the epidemic period of COVID‑19 and to analyze the influencing factors related to mental health state, as well as to provide targeted psychological intervening measures for nursing staff in the face of this major public health event.
Methods: We used data from January 28, 2019, to February 08, 2020, on the number of cases who worked in the 3A‑level hospital as nonfront‑line nurses (n = 29, 54%) and those who worked in Wuhan infectious hospital as the front‑line supporters (n = 25, 46%) came from the 3A‑level hospital. The participants completed the symptom checklist 90, and the researchers recorded data on demographics, psychological status, and the influencing factors.
Results: In our baseline scenario, we estimated that the total symptom index was 1.676 ± 0.654 for nurses who worked on the front line,1.260 ± 0.304 for those who worked as the front‑line reserve nurses, and was 1.486 ± 0.647 for those who worked as the nonfront‑line nurses.The results of correlation analysis show that the factors related to the psychological status of nurses include age, professional title, marital status, and family support; different factors have different effects on psychological status.
Conclusion: In the face of major public health emergencies, both front‑line nursing staff and nonfront‑line staff are confronted with different degrees of psychological stress, so effective psychological support should be given to improve the working efficiency and enthusiasm of nurses.
Keywords: COVID‑19, front‑line nurses, influencing factors, psychological status, reserve force
INTRODUCTION
COVID-19 is the major public health emergency that has attracted great attention from the World Health Organization and all over the world[1,2]not only because of its property of high infectivity and high fatality rate but also the diversity and uncertainty of clinical manifestations.[3-6]After the outbreak of the COVID-19 epidemic, hospitals have become the main locations to receive and treat infected patients.[7]In China,medical staff from all over the country arrived at Wuhan as the supporters at the beginning of outbreak and became the backbone in the fight against the epidemic. On the one hand,nursing staff has a high risk of being infected while caring the infected patients. On the other hand, the growing number of patients leads to a shortage of nursing resources. In this situation, long work hours and heavy workload make the nurses suffer from psychological disorders.[8]Some studies have reported the psychological status of the front-line nurses fighting COVID-19 and pointed out that most of them had stress reactions, which are mainly manifested as anxiety,terror, interpersonal sensitivity, and other psychological problems.[9]
In this study, we provide some relevant demographic data and psychological status of nonfront-line and the front-line nurses and analyze the influencing factors of these psychological issues. This study presented to hospital managers that the nurses working on the front-line need to receive psychological intervention, as well as to a portion of nonfront-line nurse staff.
METHODS
Data sources
The current study was conducted between January 28, 2019,and February 08, 2020, in a 3A-level hospital in China. The 54 participants were nurses who worked in the 3A-level hospital as the front-line reserve personnel (n = 15, 28%),duty nurses/nonfront-line nurses (n = 14, 26%) in general departments, and who worked in Wuhan infectious hospital as the front-line supporters (n = 25, 46%) came from the 3A-level hospital. All participants completed the symptom checklist-90 (SCL-90).[10]The researchers recorded data on demographics, psychological status, and influencing factors.
Ethical considerations
The questionnaire survey was conducted anonymously, and the purpose and significance of the survey were informed to the participant before the survey. We also promised that all information would just be used for research and keep strictly confidential.
Measurement
In this study, general information questionnaire made by researchers and SCL-90 compiled by an American psychologist Derogatis in 1975 were used for psychological test to assess the actual psychological status of participants in the current or recent week. SCL-90 includes nine dimensions of somatization, which are compulsive symptoms, interpersonal sensitivity, depression, anxiety,hostility, fear, paranoia, psychosis, and one other factor including diet, sleep. The 5-grade scoring method was adopted, 1 = none, 2 = mild, 3 = moderate, 4 = severe, and 5 = quite serious. There are no rigid rules to the definition of “mild, moderate and severe,” just was understood by the individuals themselves.
Research workers recorded data on demographic characteristics (age, gender, professional title, identity of the personnel, marital status, education background, job category, and family support), as shown in Table 1, and the symptom scores on each dimension.
Statistical analysis
The collected data were entered using EpiData 3.02 by two researchers to establish a database. We used SPSS 25.0 for statistical analysis (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).The logistic ordered regression model and logistic regression model were used to analyze the influencing factors related to mental health status of nurses.
RESULTS
Among the front-line nurses, 10 (40%) of the nursing staff thought that they needed psychological support. According to the national norm, 19 (76%) nurses’ habit in diet and sleep changed; 17 (68%) nurses had mild somatization; 14 (56%)nurses developed severe obsessive-compulsive symptoms;7 (28%) nurses reported various levels of hostility; 6 (24%)nurses experienced mild depression; and 5 (20%) nurses had moderate-to-severe somatic symptoms, manifested as obvious physical discomfort, such as headache and lumbago.Two (8%) showed significant anxiety and two (8%) showed significant interpersonal sensitivity; there were 10 (40%)person-times of the front-line nursing staff with abnormal factors such as fear, paranoia, and psychosis.
Overall, there were 13 (52%) nurses whose total symptom index was between 1.5 and 2.5, indicating some mild symptoms that occurred infrequently. Three were 12% of the nurses whose total symptom index was between 2.5 and 3.5,indicating that these nurses had more severe and frequent symptoms. Comparing with reserve staff and nursing staff in general departments, the total symptom index of front-line nursing staff was higher (P < 0.05), as shown in Tables 2 and 3.
Among front-line reverse nurses, 2 (13%) nurses considered that psychological support was needed; 12 (80%) nurses had mild somatization; and 9 (60%) nurses had minor and less frequent changes in their eating and sleeping status.One (6.7%) developed severe obsessive-compulsive symptoms.
Among nonfront-line nurses working in general wards,6 (43%) of them thought that they needed psychological support; 11 (78%) nurses had a slight change in their eating and sleeping status; 10 (71%) nurses had mild somatization;4 (29%) nurses had obsessive-compulsive symptoms range from moderate to severe; depression occurred in 2 (14%)nurses; 1 (7%) had severe physical discomfort; and 1 (7%)showed a predisposition to anxiety.The results of influencing factors analysis are shown in Table 4.The occurrence of obsessive-compulsive symptoms is associated with age, professional title, level of family support for the current work, and the current departments they work in. Age
between 41 and 50-year-old, primary title, family attitude of neutrality, general wards work, and thought they do not need psychological support are the independent risk factors for the obsessive-compulsive symptoms. Table 5 shows that interpersonal sensitivity is closely related to marital status, family attitude toward the current work, and the need for psychological support. Unmarried status, family’s neutral attitude, and self-belief that psychological support is not needed are independent risk factors for interpersonal sensitivity. As is shown in Table 6, the occurrence of depression is related to age and professional title.Age between 41 and 50 years and primary and intermediate professional titles are independent risk factors for depression.As shown in Table 7, the occurrence of anxiety is closely bound up with marital status, family attitude, and psychological support needs. Unmarried status, family neutral attitude, and self-belief that psychological supports are not needed are independent risk factors for anxiety. Both professional title and psychological support needs are related to the score of total symptom index,while the primary professional title and the ones who believe that they did not need psychological support are the independent risk factors to the total symptom index, shown in Table 8. As is shown in Table 9, both family attitude and psychological support needs are related to fear, while psychological support needs are related to paranoia.
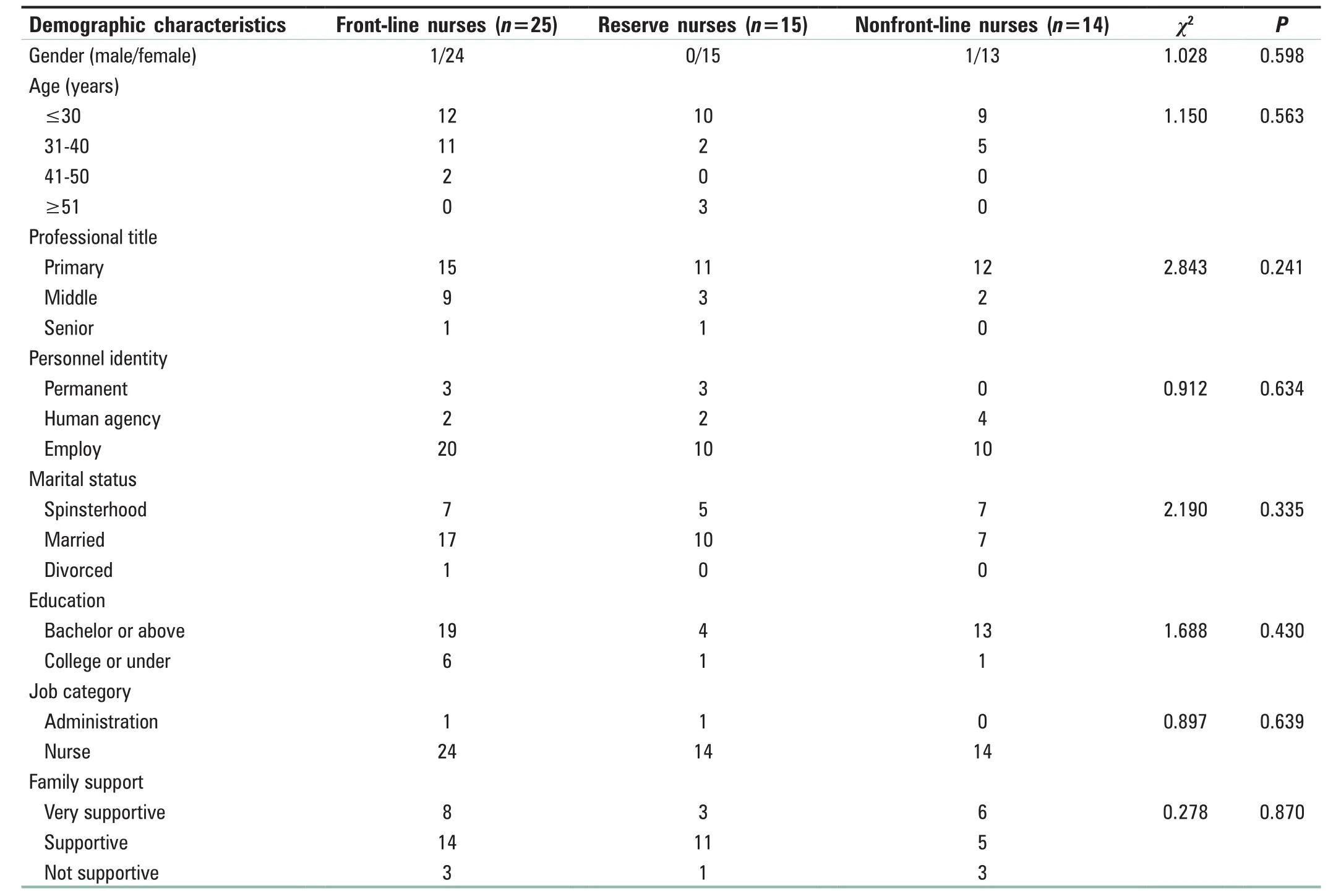
Table 1: Demographic data
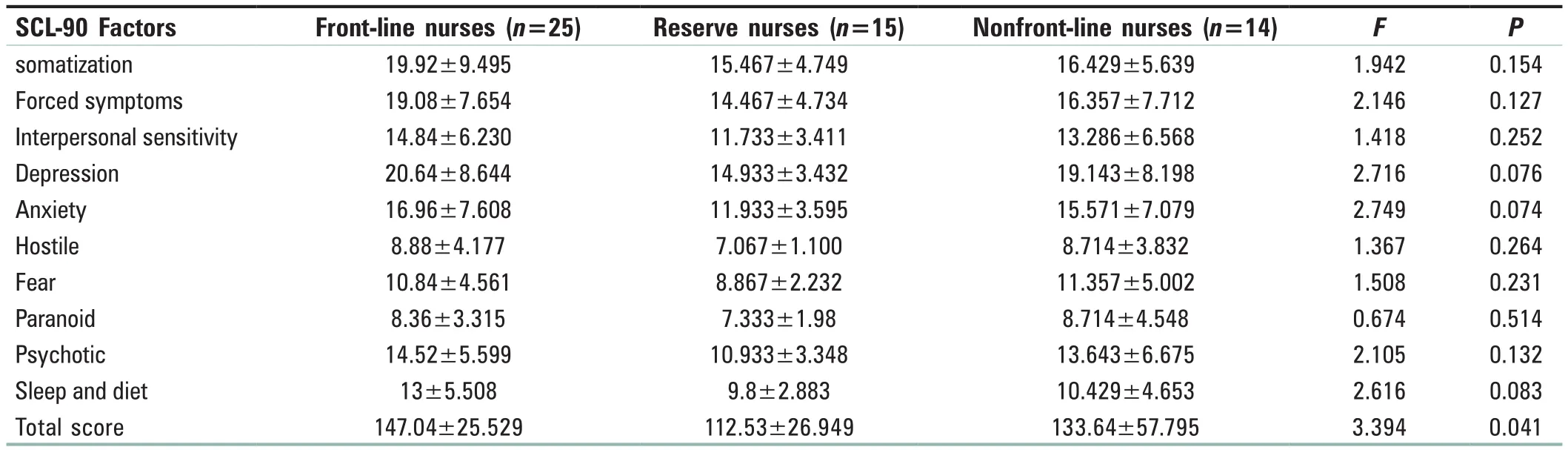
Table 2: Symptom checklist 90 factors of front-line nurses, reserve nurses, and nonfront-line nurses
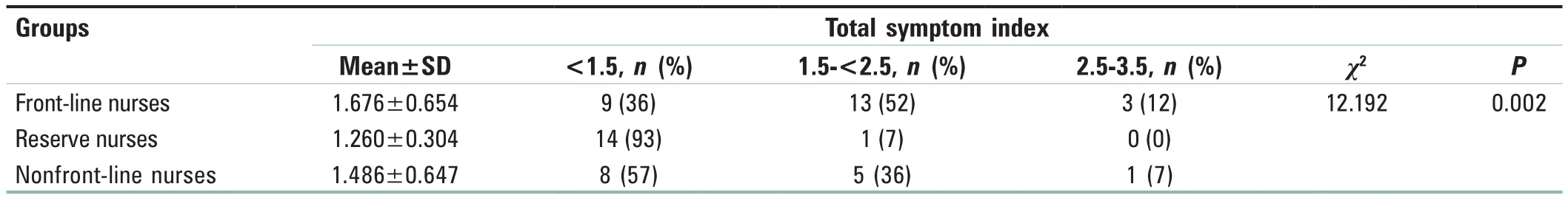
Table 3: Total symptom index of front-line nurses, reserve nurses, and nonfront-line nurses
DISCUSSION
Psychological reactions of nursing staff to the COVID‑19 epidemic
In the three nursing groups participating in this study,there are various degrees of psychological stress reaction,manifested as the discomfort of somatization, compulsive symptoms, sensitive interpersonal relationships, depression,anxiety, hostility, terror, paranoia, psychosis, and changes of diet and sleep pattern in daily life.
The mental health status of the front‑line nursesfighting the COVID‑19 epidemic
The outbreak of the COVID-19 epidemic is a disaster.Psychological quality is the basis of an effective responseto disaster relief. The occurrence of a disaster will have a huge impact on the psychology of each individual.Individuals who involve in the disaster will have an emotional response and tend to have a high risk of mental health problems,[9,11]which is consistent with the results of this study. Among front-line nurses, scores for abnormal factors such as physical symptoms, obsessive-compulsive symptoms, sensitive interpersonal relationships, and changes in sleep pattern and diet are higher than those of nonfront-line ones. On the one hand, the appearance of physical symptoms in front-line nurses may be related to high-intensity and overloaded work; on the other hand,this may be related to changes in their dietary patterns and rest rhythms and a long time of wearing airtight isolation clothing to save protective equipment. The presence of obsessive-compulsive symptoms is related to psychological stress of afraid of being infected for front-line nurses face numerous confirmed infected cases directly. Abnormal interpersonal relationships and abnormal sleep and diet may be closely related to the face of unfamiliar environments and other unfamiliar medical workers.[12]
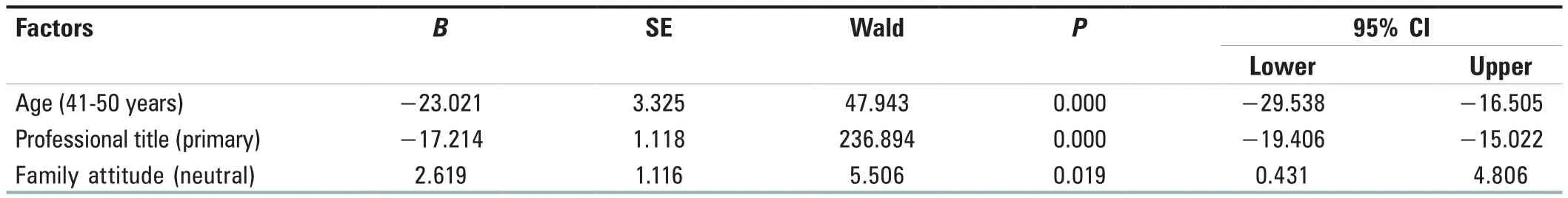
Table 4: Logistic regression analysis of risk factors for obsessive-compulsive symptoms
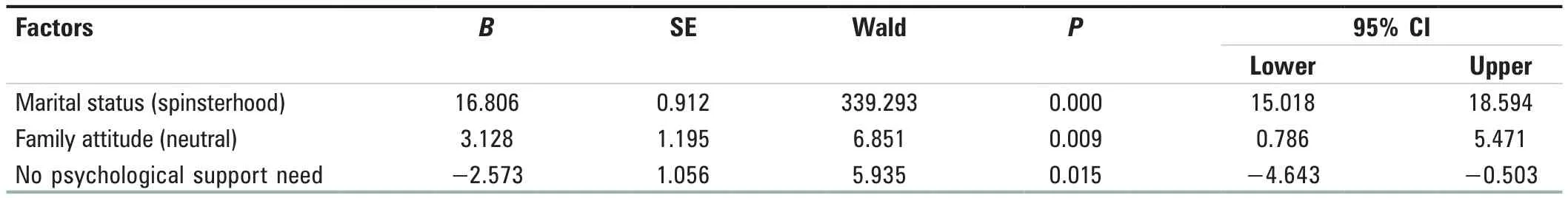
Table 5: Logistic regression analysis of risk factors for interpersonal sensitivity
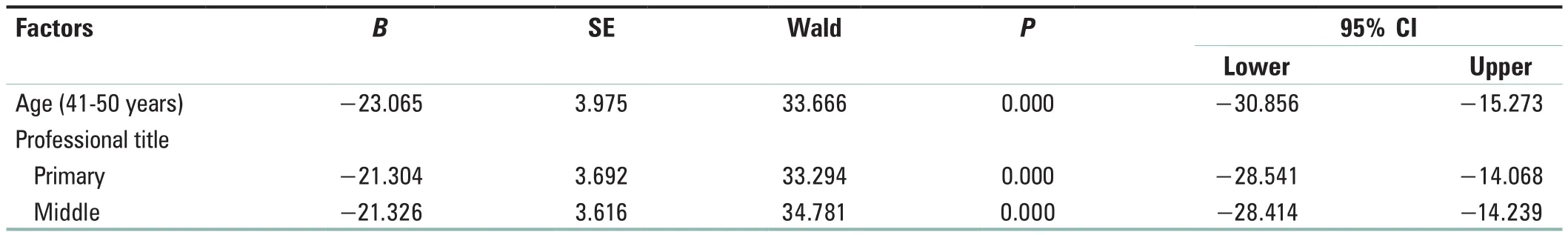
Table 6: Logistic regression analysis of risk factors for depression
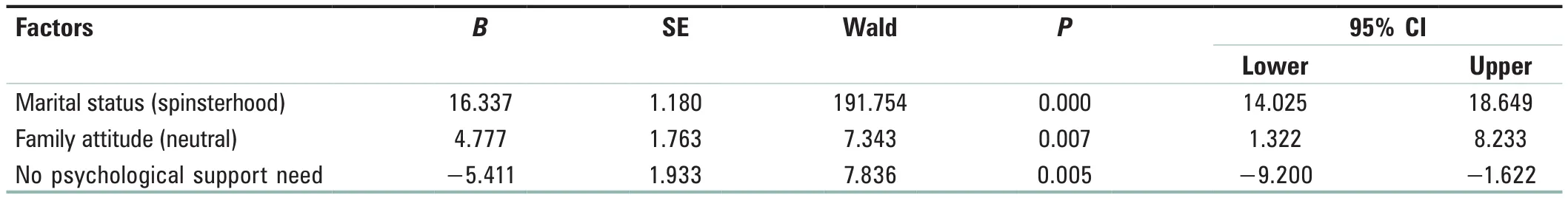
Table 7: Logistic regression analysis of risk factors for anxiety
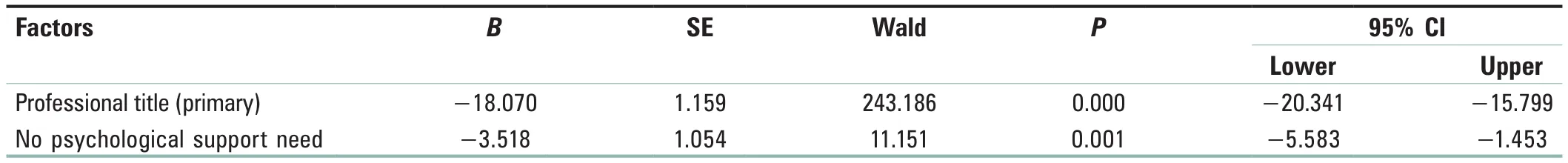
Table 8: Logistic regression analysis of risk factors for total symptom index
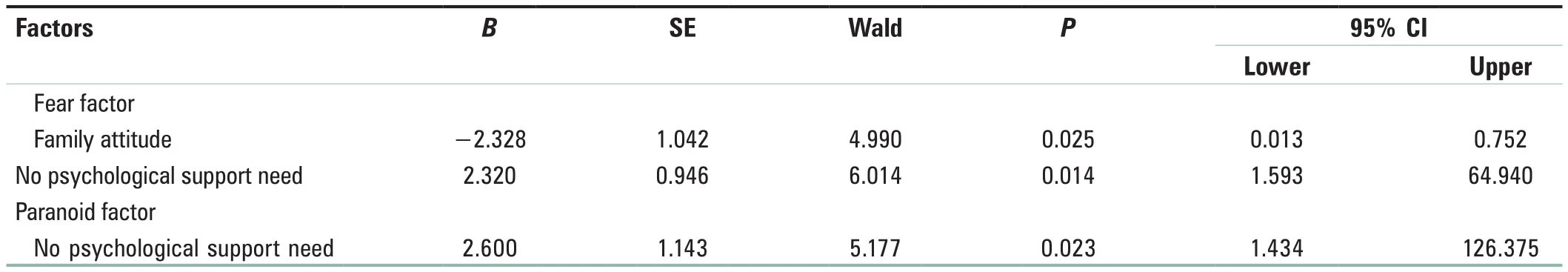
Table 9: Logistic regression analysis of risk factors for fear and paranoia
Mental health status of nonfront‑line support nursing staff
The COVID-19 has a characteristic of a wide area of infection,strong infectivity, and diversity of transmission. Facing the situation of epidemic outbreak, nonfront-line nurses also generally have different degree of psychological stress, with an abnormality in physical symptoms, obsessive-compulsive symptoms, sensitive interpersonal relationships, and changes of sleep and diet. This indicates that psychological stress and poor response in the face of major public health emergencies are common among nursing staff, which should be taken seriously. The score of the terror factor is higher than that of front-line nursing staff, which may be related to the lack of protective equipment compared to the front-line nursing staffs. It can be seen that under the current epidemic situation, the mental health of nursing staffs in ordinary wards should be paid attention to.
Analysis of psychological stress‑related factors of nursing staff
When engaged in anti-infection-related work, health-care workers are at risk of being infected. A previous research[13]has shown that this concern is the most potent cause of stress. In addition, this study shows that physical and psychological stress responses are also closely related to age,job title, marital status, and family support. (1) As women grow older, changes in hormone levels in the body can cause a series of emotional reactions,[14]leading to compulsive symptoms in older ones. (2) Nursing staff with primary and middle titles are more vulnerable to psychological stress,and depression is more likely to occur to them under high pressure comparing to nursing staff with senior professional titles.[15](3) Unmarried individuals are more likely to have psychological problems such as anxiety than married, which may related to the degree of the family support system. (4)Family members’ attitude toward the nursing staff’s work is negatively related to the generation of psychological stress.A strong family support system can promote the nursing staff to have more courage to face the disaster and strengthen their determination to overcome disaster.
Strategies to improve the psychological coping ability of nursing staff
First, strengthen the training of psychological ability and psychological support in the face of major public health emergencies. The current epidemic situation is serious,and a large number of nursing staff need to be deployed for front-line anti-epidemic work. However, the total number of nursing resources in China is currently relatively insufficient, and the ratio of doctor to nurse is imbalanced.Front-line nurses and general department nurses both face great occupational stress. Studies have shown that work stress can affect the physical and mental health of nurses, reduce the enthusiasm of the nurses, produce fatigue, and affect the quality of work.[16,17]Therefore,hospitals need to conduct comprehensive psychological stress training for all nursing staff in a timely manner and develop a targeted psychological support plan. Studies[18-20]have shown that mindfulness decompression training can effectively improve mood and reduce stress, burnout, and anxiety. For nurses who are older, junior to intermediate professional titles, unmarried, and have poor family support, it is necessary to provide in psychological comfort and support, to keep abreast of the psychological status of such nurses, and to provide psychological intervention when necessary.
Second, strengthen the training of emergency response ability for major public health emergencies. According to the analysis of questionnaire entries, 35% of nursing staff are worried that it will be difficult to complete the task. It can be seen that in this epidemic, the lack of knowledge and skills related to infection is one of the factors causing the change of mental health status of nursing staff. Therefore,the hospital conducts relevant knowledge and skills training in a timely manner and through intensive exercises to make the nursing staff proficient in relevant skills and has the ability to respond to major public health emergencies.Through training, the nursing staff’s confidence in the competence of the work can be strengthened, while their anxiety and psychological stress can be reduced and alleviated.
CONCLUSION
In this study, the SCL-90 scale was used to evaluate the mental health of nursing staff in the 3A-level hospitals during the period of the COVID-19 epidemic. It is both the front-line nurses fighting the epidemic and the general ward nurses that face different levels of psychological stress. Through correlation analysis, the factors affecting the mental health of nursing staff in the face of major public health emergencies are summarized, and the aim is to provide a reference for psychological support for nursing staff in epidemic prevention and control. The limitation of this study is that due to the influence of the epidemic situation, the data of questionnaires were used to collect on line instead of face-to-face method.In addition, the selection of research subjects may have sample selective shifts and lack of multicenter data support.Moreover, more clinical studies of psychological support programs are needed to refine emergency psychological training for major public health emergencies.
Financial support and sponsorship
This work was supported by the Lanzhou city science and technology project: Psychological Intervention Study of COVID-19 Isolation and Protection Medical Workers by Mindfulness Behavior Delivery.
Conflicts of interest
There are no conflicts of interest.
杂志排行
Journal of Integrative Nursing的其它文章
- The application of feedforward control in the nursing emergency management of COVlD‑19
- The psychological experience of Chinese nurses in support of COVlD‑19 frontline: A qualitative study
- Management strategy of prevention and control of nosocomial infection of COVlD‑19 in blood purification center
- The effects of health Qigong Baduanjin on the prevention,treatment, and recovery of COVlD‑19
- Traditional Chinese medicine nursing protocols for COVlD‑19
- Nursing emergency management practice of COVlD‑19 in a traditional Chinese medicine hospital
