Contemporary indications for and outcomes of hepatic resection for neuroendocrine liver metastases
2020-06-12StevenScovilleDimitriosXourafasAslamEjazAllanTsungTimothyPawlikJordanCloyd
Steven D Scoville, Dimitrios Xourafas, Aslam M Ejaz, Allan Tsung, Timothy Pawlik, Jordan M Cloyd
Abstract
Key words: Carcinoid; Neuroendocrine tumor; Primary tumor resection; Intraoperative ablation; Cholecystectomy; Small bowel resection
INTRODUCTION
Neuroendocrine tumors (NET) are a heterogeneous group of neoplasms that can occur anywhere in the body but commonly arise from the gastrointestinal tract. While relatively rare, the incidence and prevalence of NETs are steadily increasing, at least in part due to improved imaging and diagnostic techniques[1,2]. Despite their low grade nature, a substantial proportion (60%-80%) of well-differentiated NETs are diagnosed with or will develop neuroendocrine liver metastases (NELM), which is one of the strongest prognostic factors among patients with NETs[3]. For example, the 5-year overall survival of patients with untreated NELM range from 13% to 54%,compared with 61% to 79% among individuals who undergo treatment[4-8].
Multiple treatments exist for patients with NELM including surgical resection,ablative techniques, transarterial therapies, somatostatin analogs, cytotoxic chemotherapy, targeted therapies, and peptide receptor radionuclide therapy[4]. Other novel systemic and targeted therapies are rapidly emerging[9,10]. Despite the absence of level I evidence, surgical resection is associated with the best long-term outcomes based on retrospective cohort studies and meta-analyses[6,11,12]. Indeed, even cytoreductive surgery (i.e., surgical debulking) of NELM has been associated with improved overall survival if residual disease less than 10%-30% can be achieved[5,13-15].Based on these data, surgical resection of NELM has been recommended as the preferred initial approach, when feasible, by the European Neuroendocrine Tumors Society and North American Neuroendocrine Tumors Society[16,17].
Previous studies evaluating the short-term outcomes of surgery for NELM have frequently been limited by their retrospective, single-institution nature[18-22]. Other more recent multi-institutional studies have been limited to high-volume institutions and conducted over long study periods[6,14,23]. Thus, there is a need for an evaluation of contemporary practice patterns and outcomes from a population-based perspective.Such information would inform patient selection and facilitate patient education and the informed consent process. Therefore, we utilized the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) targeted hepatectomy database to analyze contemporary characteristics of patients with NELM who underwent liver resection (LR) in the United States and evaluate factors associated with postoperative morbidity and mortality.
MATERIALS AND METHODS
Data acquisition and study population
The ACS-NSQIP data set is a national validated and risk adjusted outcomes based database that includes demographic, clinical, perioperative, and 30-d postoperative details of patients undergoing surgery from 600 eligible hospitals across the United States. The ACS-NSQIP uses a systemic sampling process to ensure that each case has an equal chance of selection and it is frequently monitored to minimize sample bias. A retrospective review of the 2014-2017 ACS-NSQIP and targeted hepatectomy databases were performed and patients were matched based on case ID numbers. All adult patients undergoing LR were identified using Current Procedural Terminology codes 47120, 47122, 47125, and 47130.
Study variables and outcomes
Independent variables included demographic, preoperative health status, relevant comorbidities, operative, and postoperative outcomes. Demographics included age and gender. Preoperative health included American Society of Anesthesiologists(ASA) classification, body mass index, weight loss within 6 mo from surgery,smoking, chronic steroid use, preoperative sepsis (systemic inflammatory response syndrome or septic shock) and preoperative transfusion. Comorbidities included diabetes mellitus, chronic obstructive pulmonary disease, hypertension requiring medications, bleeding disorders, congestive heart failure. Targeted hepatectomy variables included neoadjuvant therapy within 90 d of surgery, ascites, viral hepatitis,and pre-operative biliary stent placement. Operative variables consisted of operative approach (open, laparoscopic, robotic), type of resection (trisegmentectomy, total right or left hemihepatectomy, or partial hepatectomy), concomitant procedures(cholecystectomy, intestinal resection, partial pancreatectomy), size of metastatic lesion (< 2, 2-5, or > 5 cm) number of metastatic lesions (1-2, 3-5, or > 5), number of concurrent partial hepatectomies (0, 1-5, 6-9, or > 10), liver texture (normal, congested,cirrhotic or fatty), operative time, pringle maneuver during resection, concomitant intraoperative ablation (IA), and biliary reconstruction.
Overall morbidity included each of the following within 30 d from the date of surgery: Superficial, deep and organ/space surgical site infection, sepsis, respiratory complications including pneumonia or reintubation, pulmonary embolism, deep vein thrombosis, myocardial infarct, cardiac arrest, stroke, renal complications such as renal insufficiency or urinary tract infection, hemorrhage requiring at least 4 U of packed red blood cells, bile leak, liver intervention post hepatectomy and postoperative liver failure. Perioperative mortality was also measured and defined as death within 30 d after LR. Length of stay, discharge disposition, 30-d readmission and reoperation were also among the postoperative measures assessed.
Statistical analysis
Descriptive statistics were reported as percentages of the total number of patients in the study. Univariate and multivariate analyses were used to identify factors associated with the development of overall morbidity and mortality within 30 d of surgery. Logistic regression analysis was used for univariate analysis. Stepwise logistic regression analysis was used for multivariable analysis and included all noncollinear variables. Results are reported as odds ratios (OR) and 95% confidence intervals (CI). Analyses were performed using SAS 9.2 (SAS Institute, Inc., Cary, NC,United States). P values < 0.05 were considered statistically significant. All statistics were performed by an experienced biostatistician.
RESULTS
Patient characteristics
Between 2014-2017, 669 patients were identified within the ACS-NSQIP database who underwent LR for NELM. Complete demographic and clinicopathologic criteria of the cohort are listed in Table 1. The median age was 60 [interquartile range (IQR): 51-67],51% were male and the mean body mass index was 27.4 (IQR: 24-32). Most patients underwent partial hepatectomy (71%) while fewer underwent hemihepatectomy(23%) or trisegmentectomy (6%). The majority of operations were open (82%); fewer were laparoscopic (17%) or robotic (1%). The mean number of lesions resected was 3.8(range 1-9) and the most common size of the largest tumor was 2-5 cm (45%) (Figure 1A and B). Among all patients, 30.6% underwent concomitant IA in conjunction with a LR. In addition, 45.4% of patients underwent a combined resection in addition to the LR. The most common concomitant procedure was a cholecystectomy (28.8%),followed by intestinal resection (20.2%) and pancreatectomy (3.4%) (Figure 1C).
Perioperative outcomes
Table 2 reports the postoperative outcomes of patients undergoing resection of NELM. Median operative time was 232 min (IQR: 179-297) and the mean length of stay was 6 (IQR: 4-8) d. The overall 30-d complication rate was 29% with the most common perioperative complications being perioperative transfusion (15.5%),intraabdominal infection (7.3%), bile leakage (5.9%), sepsis (5.6%), surgical site infection (3.5%), reoperation (3.1%), pneumonia (2.9%), liver failure (2.6%), and pulmonary embolism (2%). Of note, serious adverse events such as stroke, cardiac arrest, and myocardial infarction occurred in less than 1% of all patients undergoing resection for NELM. Postoperative mortality occurred in 1.3%. The vast majority(95%) of patients were able to be discharged home and readmission was required in 11.2% of the patients.
Predictors of postoperative morbidity
Factors associated with 30-d morbidity on univariate analysis are reported in Table 3.ASA class of ≥ 3 (OR = 2.418, 95%CI: 1.422-4.113, P = 0.0011), open approach (OR =1.943, 95%CI: 1.218-3.102, P = 0.0053), right, left or trisection hepatectomy (OR = 1.660,95%CI 1.169-2.355, P = 0.0046), and operative time (> 230 min, OR = 2.403, 95%CI:1.407-2.968, P = 0.0002) were all associated with increased morbidity while IA was associated with a decrease in perioperative morbidity (OR = 0.686, 95%CI: 0.476-0.988,P = 0.0431). Interestingly, the use of concomitant procedures (including bowel resections, cholecystectomy, or pancreatectomy), as well as the size or number of tumors were not associated with postoperative morbidity.
On multivariable logistic regression, ASA class of ≥ 3 (OR = 2.089, 95%CI: 1.197-3.645, P = 0.0095), open approach (OR = 1.867, 95%CI: 1.148-3.036, P = 0.0118), right,left or trisegmental hepatectomy (OR = 1.618, 95%CI: 1.014-2.582, P = 0.0437), and operative time > 230 min (OR = 1.731, 95%CI: 1.168-2.565, P = 0.0062) were independently associated with increased morbidity while normal liver texture was protective of overall morbidity (OR = 0.641, 95%CI: 0.433-0.950, P = 0.0266) (Table 4).
DISCUSSION
The incidence of NETs is increasing worldwide and a majority of patients will present with metastatic disease in their liver[1]. NELM is a strong negative prognostic factor for survival and is associated with significant reductions in patient quality of life[24].While several systemic and liver-directed therapies are available, surgical resection is typically recommended when feasible[25]. In this paper, we used a contemporary,population-based, prospective database to define the characteristics and outcomes of patients undergoing surgery for NELM in the United States. These results highlight several important findings. First, the majority of operations are being performed for small tumors in the setting of multifocal disease and typically are minor resections.Second, a significant proportion of cases are being performed concomitant with another operation, either liver IA, cholecystectomy, or (presumably) primary tumor resection. Finally, modern surgery for NELM can be performed with relatively minimal postoperative morbidity (29%) and mortality (1.3%). These results are criticalfor informed preoperative discussions with patients as well as future comparative effectiveness research with other liver-directed treatments.

Table 1 Demographic, clinical, and operative characteristics of patients with neuroendocrine liver metastases undergoing resection
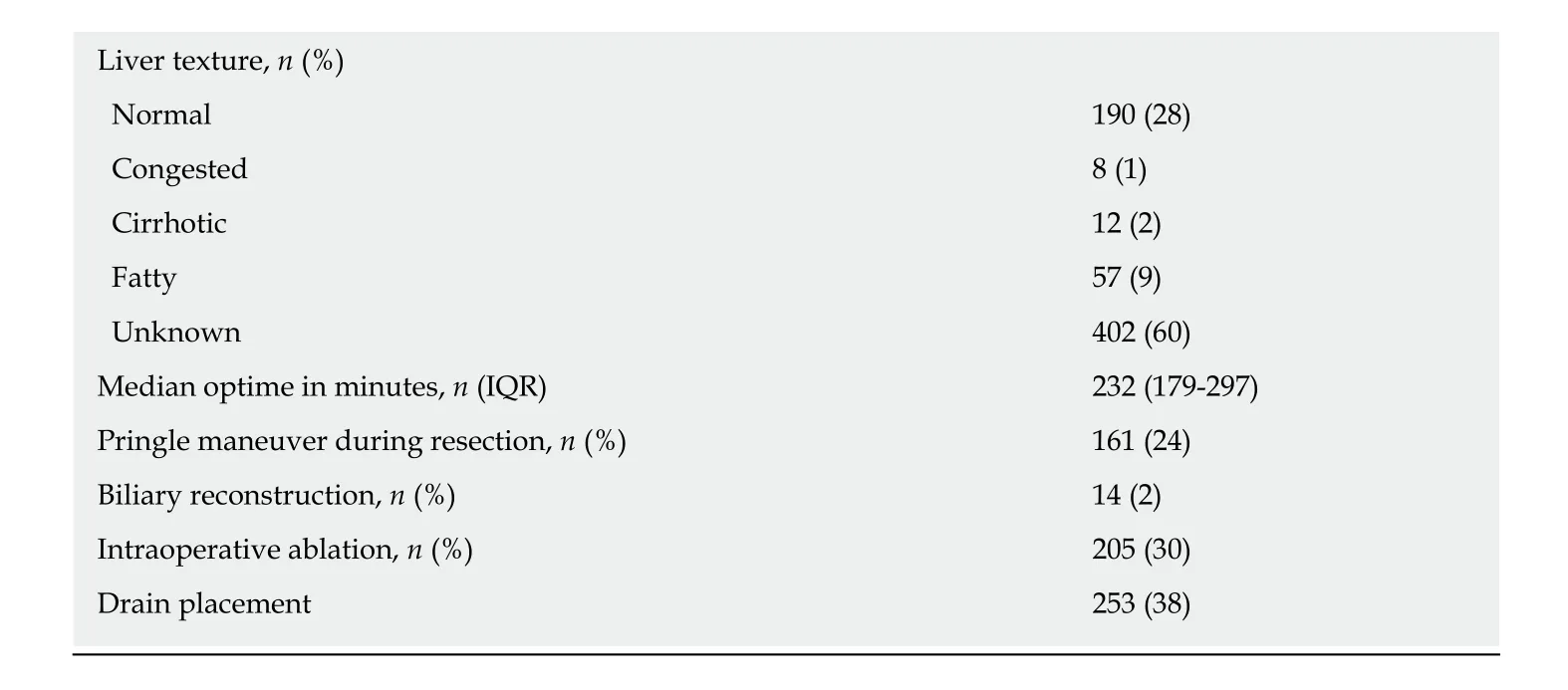
NELM: Neuroendocrine liver metastases; IQR: Interquartile range; BMI: Body mass index; ASA: American Society of Anesthesiology.
Recent advances in the perioperative management of patients undergoing LR have improved the safety of hepatectomy and expanded criteria for selecting patients for surgery. Indeed, a recent study by Cloyd et al[26]evaluated nearly 4000 patients who underwent LR over two decades and noted steady improvements in postoperative morbidity despite increases in case complexity. Improvements in the outcomes of LR are likely multifactorial but improved patient selection, evaluation and optimization,are paramount. Accurate liver volumetry and future liver remnant augmentation have been important strategies for minimizing post hepatectomy and postoperative liver failure[27,28]. Improved perioperative and anesthetic care, including reduced intravenous fluid administration and less blood loss, have similarly been critical advances in contemporary hepatic surgery. The introduction of enhanced recovery after surgery processes have further contributed to reduced morbidity following surgery and are now commonly routinized at major medical centers[29]. Finally,implementation of laparoscopic and robotic approaches for surgery have led to reduced postoperative pain, blood loss, and length of hospital stay with similar outcomes compared with open approaches[30-33].
Prior studies evaluating the role of IA for NELM have demonstrated that this therapeutic approach is generally well tolerated and is indicated for patients whose tumors are not amenable to resection[6,34]though the safety of IA during surgery for NELM has not been thoroughly evaluated[34-36]. In this study, we noted that IA was associated with decreased 30-d morbidity in univariate analysis though this association did not persist on multivariate analysis. These findings are consistent with a recent study evaluating IA during resection of colorectal liver metastasis which found lower overall morbidity, hospital length of stay, and readmission rates in patients who underwent LR and IA compared to patients who underwent LR alone[37].Based on these results and others, IA appears to be a safe and effective strategy to expand the surgical options for patients with multifocal NELM.
While the role of primary tumor resection in the setting of unresectable NELM remains controversial, resection of the primary NET is indicated when liver metastases are resectable[19,38-41]. The current study suggests that resection of the primary (e.g., pancreatectomy, intestinal resection) can be performed safely and is not associated with increased postoperative morbidity. These findings are consistent with the large body of literature which suggests that most LRs for colorectal liver metastasis can be performed safely in a combined fashion with standard colorectal resections[42,43].
While the ACS-NSQIP targeted hepatectomy database has the advantage of containing hepatectomy-specific perioperative variables, a limitation of the current database was the lack of cancer- and patient-specific information. For example, the database lacked relevant information such as the symptomatic status of patients,functional status of tumors, tumor grade, or presence of extra-hepatic disease. In addition, it lacked Furthermore, as the study was limited to the 30-d postoperative period, we were unable to describe the long-term efficacy of LR for NELM. However,the purpose of the current study was to evaluate the indications for and short-term outcomes of surgery for NELM. Multiple prior studies have found that LR for NELM is associated with good long-term survival[4,6,44]. Similarly, the ACS-NSQIP database did not have information on carcinoid crisis, however, previous studies have shown this to be a relatively rare event[45,46]. This study had several other limitations,primarily related to its retrospective nature and the fact that data were limited to the 30-d postoperative period which may be insufficient to capture all complications.

Figure 1 Indications for liver resection for neuroendocrine liver metastases. Overall size (A) and number (B) of neuroendocrine liver metastases and frequency of concomitant procedures including intraoperative ablation (C)among patients undergoing liver resection for neuroendocrine liver metastases.
In conclusion, in this contemporary population-based analysis, we demonstrated that LR can be performed for NELM with relatively low postoperative morbidity and mortality. Concomitant operations such as cholecystectomy, bowel resection,pancreatectomy, and IA can safely be performed and do not contribute to increased morbidity. Careful patient selection, minimizing operative time, and utilizing minimally invasive surgical approaches may help reduce postoperative morbidity.While multiple therapeutic options exist for NELM, given the excellent long-term outcomes observed in the literature and the satisfactory short-term outcomes demonstrated herein, surgical resection should remain the standard of care when feasible.
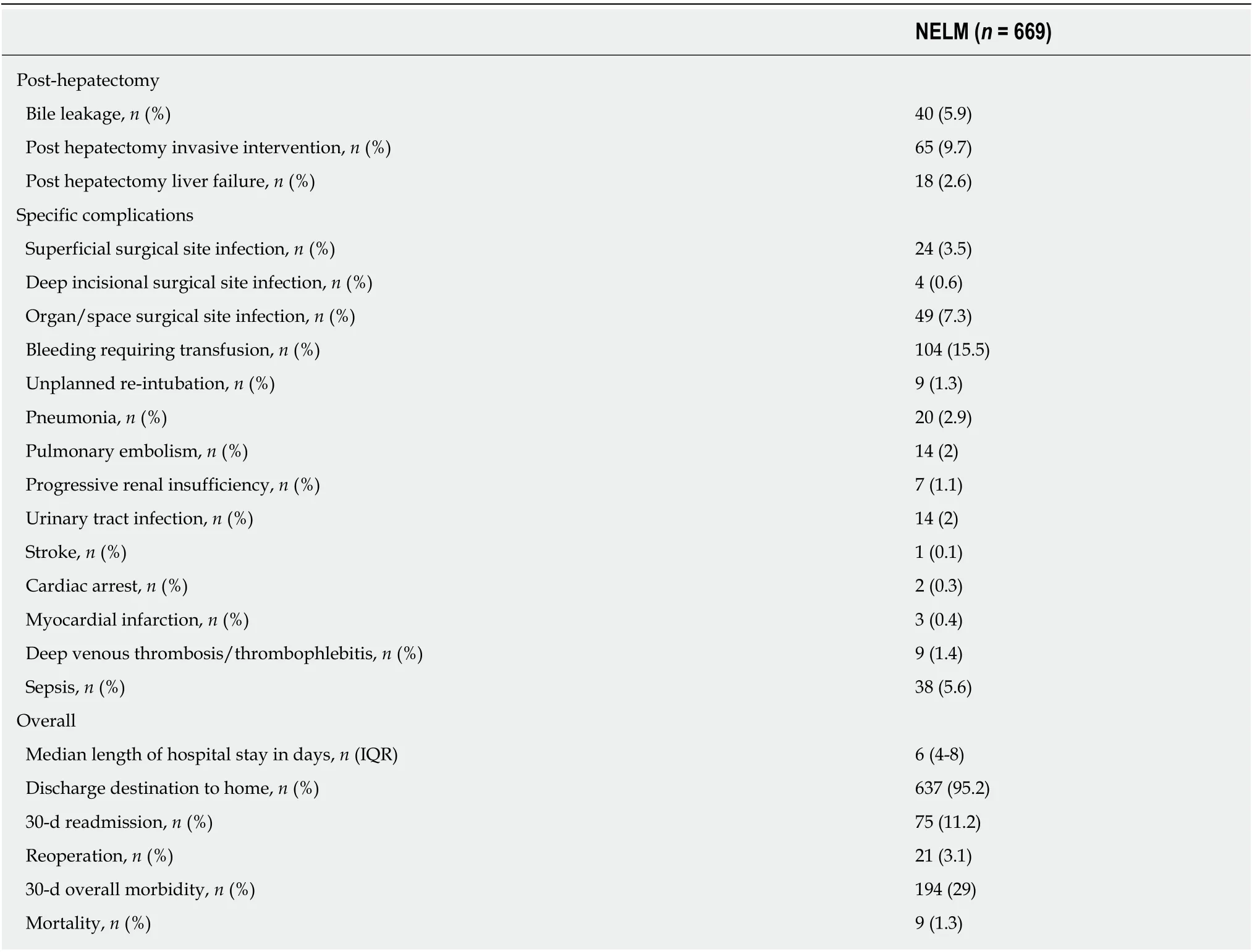
Table 2 Postoperative outcomes of patients with neuroendocrine liver metastases undergoing liver resection

Table 3 Significant predictors of 30-d overall morbidity among patients undergoing hepatectomy for neuroendocrine liver metastases based on univariate logistic regression analysis

Table 4 Significant predictors of 30-d overall morbidity among patients undergoing hepatectomy for neuroendocrine liver metastases based on multivariate stepwise logistic regression analysis
ARTICLE HIGHLIGHTS
Research methods
A retrospective review of the 2014-2017 American College of Surgeons National Surgical Quality Improvement Program targeted hepatectomy database was performed to identify patients who underwent hepatic resection for NELM. Perioperative characteristics and 30-d morbidity and mortality were analyzed.
Research results
Among 669 patients who underwent liver resection for NELM, the number of metastases resected ranged from 1 to 9 though the most common (45%) number of tumors resected was one.The majority (68%) of patients had a largest tumor size of < 5 cm and most patients underwent partial hepatectomy (71%). The majority of operations were open (82%) versus laparoscopic(17%) or robotic (1%). In addition, 30% of patients underwent intraoperative ablation while 45%had another concomitant operation including cholecystectomy (28.8%), bowel resection (20.2%),or partial pancreatectomy (3.4%). Overall 30-d morbidity and mortality was 29% and 1.3%,respectively. On multivariate analysis, American Society of Anesthesiologists class ≥ 3, open approach, formal hemi-hepatectomy or trisectionectomy, and prolonged operative time were associated with higher 30-d morbidity. Concomitant procedures including intraoperative ablation, small bowel resection, or pancreatectomy were not independently associated with higher morbidity.
Research conclusions
In this contemporary population-based analysis, we demonstrated that hepatic resection can be performed with relatively low postoperative morbidity and mortality for patients with NELM.Concomitant operations such as cholecystectomy, bowel resection, pancreatectomy, and liver ablation can safely be performed and do not contribute to increased morbidity. Careful patient selection, minimizing operative time, and utilizing minimally invasive approaches may help reduce postoperative morbidity. While multiple therapeutic options exist for NELM, given the excellent long-term outcomes observed in the literature and the satisfactory short-term outcomes demonstrated in the current study, surgical resection should remain the standard of care when feasible.
Research perspectives
This study highlights the current population-based indications for liver resection for patients with neuroendocrine liver metastases and confirms satisfactory short-term outcomes. In light of these findings, future research should focus on expanding the indications for hepatic resection particularly given the increasing number of liver-directed and systemic therapy options available. Future prospective studies should evaluate the optimal sequencing of liver-directed therapies including neoadjuvant and adjuvant strategies to improve long-term outcomes.
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Clinical course of suspected small gastrointestinal stromal tumors in the stomach
- Mammalian target of rapamycin inhibitors after post-transplant hepatocellular carcinoma recurrence: Is it too late?
- Management of complicated acute appendicitis in children: Still an existing controversy
- Feasibility of robotic assisted bladder sparing pelvic exenteration for locally advanced rectal cancer: A single institution case series
- Short term outcomes of minimally invasive selective lateral pelvic lymph node dissection for low rectal cancer
- Newly developed self-expandable Niti-S MD colonic metal stent for malignant colonic obstruction