Appendicitis-mimicking presentation in fishbone induced microperforation of the distal duodenum: A case report
2020-06-11DanielLimChengMawHo
Daniel Lim, Cheng-Maw Ho
Abstract
Key words: Fish bone; Duodenal microperforation; Acute appendicitis mimic; Case report; Observer error
INTRODUCTION
Fishbones are one of the most common forms of ingested foreign bodies. While most ingested fishbones are asymptomatic, some can lodge themselves within the gastrointestinal (GI) tract and cause a microperforation[2]. Depending on its location,they can cause local inflammation and haematoma formation[3,4]. This case is particularly relevant due to the possible epidemiological link between the Chinese population and the increased prevalence of ingested fishbones, as suggested by Arulanandamet al[5]who attributed this to an increase in consumption of unfilleted fish and the common practice of deboning fish using their mouths.
Acute appendicitis is common and classically presents with migrating lower abdominal and right iliac fossa pain with the accompanying symptoms of pyrexia and general malaise. The current diagnostic approach incorporates a combination of clinical suspicion, haematological findings, the exclusion of other differentials,ultrasound and radiological investigations to diagnose acute appendicitis[6]. Increasing use of computer tomography (CT) imaging and employment of the Alvardo criteria in clinical practice has further increased the diagnostic accuracy of clinicians, achieving a positive diagnosis rate of 80%-95%[7]. However, misdiagnosis, such as fishboneinduced injury can still occur, as seen by the following case.
This case report is primarily written to highlight a unique case of a patient who presented with a fishbone-induced microperforation of the upper GI tract that accurately mimicked the symptoms of acute appendicitis, the diagnostic difficulty that the team experienced and the management pathway that was undertaken in the treatment of this patient. No proposed scientific question was formulated through the abovementioned case.
CASE PRESENTATION
Chief complaints
This 79-year-old Chinese male presented with a one-day history of lower abdominal pain and pyrexia.
History of present illness and past illness
The pain initially presented at the peri-umbilical region and later migrated to his right lower quadrant. He reported no associated dysuria, nausea, vomiting, hematemesis or melena and has a known past medical history of hypertension, type 2 diabetes mellitus and hyperlipidaemia. He was recently admitted for bronchoscopy and biopsy of a left bronchial mass a week prior to this episode. This was later found to be a bronchial carcinoid tumour.
Physical examination
On examination, he had generalized lower abdominal tenderness with maximal tenderness around the periumbilical and right lower quadrant. His abdomen was otherwise soft with mild guarding, active bowel sounds and no rigidity. His vitals were slightly deranged, with a tachycardia (heart rate 110 beats/min), tachypnea(respiratory rate 22 times/min), mild hypertension (132/78 mmHg) and pyrexia (38.4°C) Otherwise, his oxygen saturations remained normal (96%) on room air and he had no acute confusion or neurological deficit.
Laboratory and imaging examinations
He had a raised white cell count of 16.98 × 103/mm3with raised neutrophils. Creactive protein (0.98 mg/L) and other parameters were within the normal range. CT of the abdomen and pelvis with contrast excluded any renal calculi and revealed the presence of a dilated tubular structure with mild fat stranding with increased enhancement (Figure 1). This structure and the associated inflammatory changes were presumed to be an inflamed appendix. As the symptoms and radiological evidence fit,a preliminary diagnosis of acute appendicitis was made.
阮小棉把报纸折成飞机,坐在楼顶掷出去。她不相信这样的爱情,那都是作家和剧作家们编出来骗人的东西。楼顶的风很大,把她的裙子鼓起来,袖子也鼓起来,她用手拢一下袖口,扎住,就变成了很复古的宫廷灯笼袖。她小时候就有一件那样的小纱裙,粉红色,大大的裙摆,灯笼袖。每个女孩子都有童年,童年里谁都可以成为公主。
Initial intervention and course
The patient underwent a laparoscopic appendectomy the following day. An intact and mildly erythematous appendix was resected and some clear ascitic fluid was drained from within the peritoneum.
During the immediate postoperative phase, the patient suffered an acute deterioration and had increasing oxygen requirements. There were also concomitant acute changes of consolidation seen on his chest radiograph. These prompted concerns of possible unresolved sepsis. A further review of his CT scans revealed an additional finding of a fine fishbone of 1.4 cm in length. This had caused a microperforation at the inferior border of the 3rdsegment of the duodenum, resulting in the formation of an abscess and associated fat stranding along the right pararenal fascia (Figures 2 and 3).
FINAL DIAGNOSIS
Further review of his CT scan suggested that the preliminary diagnosis was inaccurate, and that the patient most likely had a fishbone induced microperforation of his duodenum that resulted in the formation of a small retroperitoneal abscess.
TREATMENT
Based on his deteriorating clinical condition at that time, a decision to undergo an exploratory laparotomy was made. In the interim, the patient was started on broadspectrum intravenous antibiotics (Meropenam). The laparotomy was performed 12 h after the appendectomy. The localized retroperitoneal abscess was drained and 10 mL of pus was aspirated. However, despite thorough examination of the duodenum, both the exact site of perforation and the fishbone were unable to be identified and retrieved. Manual pressure was then applied at the presumed site of the microperforation based on the CT scan to reintroduce the bone back into the intestinal lumen. The area was subsequently washed out and a retroperitoneal drain was inserted.
OUTCOME AND FOLLOW-UP

Figure 1 Computed tomography abdomen and pelvic with contrast showing distended tubular structure(demonstrated by the arrow) that was presumed to be the appendix.
Post-operatively, the patient was transferred to the intensive care unit for 2 d. A feeding jejunostomy was inserted for enteral feeding and to prevent the recurrence of a retro-peritonitis. He did not require any inotropic support and required decreasing amounts of ventilatory support to manage his oxygen requirements. His oxygen saturations improved, and the changes noted in his chest radiograph rapidly resolved(Figure 4). His pain was well controlled with analgesia and he was stepped down to the wards where he recovered well. His antibiotics was then converted to an oral form(levofloxacin) and his retroperitoneal drain was removed. Regular oral feeding was re-introduced and the patient remained well with further complications. He was subsequently discharged after a total of 11 d in hospital. On follow-up, the patient remained well and did not develop any long-term complications related to his ingested fishbone. He then had his jejunostomy tube removed and required no further follow-up from the team.
Subsequent pathological examination of the resected appendix showed minimal infiltration of neutrophils. This effectively excluded acute appendicitis as the main diagnosis for this episode. His cultures from the abscess isolated intestinal coliforms and confirmed that the infection was from a GI source. Detailed cross-examination of the entire case revealed that his initial oxygen desaturation were secondary to pulmonary haemorrhage that occurred from traumatic suctioning during anaesthesia and was the cause of his acute changes on his chest radiographs. This was incidental and was not related to his intrabdominal sepsis.
DISCUSSION
Fishbone microperforation of the distal GI tract is rare but is increasingly reported across various centres in the last 10 years[8-10]. However, due to its ambiguous presentation, the diagnosis can often be missed, leading to increased complications[11].This scenario may be further complicated by the possible subacute presentation of fish-bone induced microperforation and the individual patient’s lack of awareness of fishbone ingestion[9]. Specifically, this patient’s ingestion of the fish bone was attributed to his consumption of fish soup a week ago as a traditional remedy following his recent biopsy for his bronchial carcinoid tumour and he had not noticed the ingestion of any fishbone.
Typically, fish bones lodge themselves within the aerodigestive tract, and occasionally at the distal GI tract, near the terminal ileum and caecum[12-14]. Only a few cases of duodenal, jejunal and proximal ileal microperforations were reported and these usually resulted in damage to local structures like the pancreas and the development of peritonitis[9,15].
What defines this case was the way this patient presented. He presented with the classical symptoms of pyrexia, raised inflammatory markers and migratory epigastric to right lower quadrant abdominal pains that is commonly associated with acute appendicitis. Furthermore, the positive radiological findings of a distended appendiceal structure seemed to agree with the clinical presentation and further supported the initial diagnosis of acute appendicitis. In addition, due to the lack of patient awareness of fishbone ingestion and the small number of similar cases reported, the fish bone was not noticed during the initial interpretation of the scan.Therefore, the final diagnosis of a duodenal microperforation with a retroperitoneal abscess raised unexpected great attention.
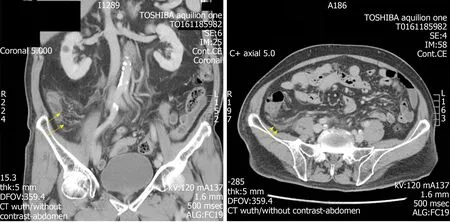
Figure 2 Axial and coronal views of prominent fat stranding in the right lower quadrant (arrows).
While the exact pathophysiology remains unclear, we believed that the initial microperforation caused the presentation of periumbilical pain. Due to the retroperitoneal nature of the distal duodenum, it is postulated that intestinal content must have seeped within the retroperitoneal space into the right pararenal fascia,forming the retroperitoneal abscess. This resulted in the development of localized“retro-peritonitis” which corresponded to his right lower quadrant pain. This disease process is the likely reason behind the migratory nature of his pain. Furthermore, we believe that the retroperitoneal nature of the site of microperforation and subsequent abscess formation accounted for the inability to visualize any intra-peritoneal pathology during the initial laparoscopy.
The management of such microperforation can take either a medical or surgical approach. Medical treatment is usually done via the endoscopic retrieval of the fish bone, alongside intravenous antibiotic administration and can be considered in patients who present without major complications[10,16]. This was not suitable in this patient due to his deteriorating clinical condition at the time and concerns regarding progressing sepsis. As a result, a surgical approach was considered. This usually includes a midline laparotomy with identification and closure of the area of perforation via primary repair, the removal of the fishbone and the aspiration of any abscess or fluids within the abdominal or retroperitoneal space, with post-operative antibiotics and monitoring[10].
In this case, the inability to identify and remove the fishbone during the laparotomy did not appear to have an impact on the recovery of the patient and he improved clinically. It is therefore hypothesized that the fishbone dislodged itself form the initial area of microperforation and had passed through the entirety of the patient’s GI tract without any further incident[2]. This is further supported by the uneventful post-operative course and the lack of any further complications pertaining to the retained fishbone. As a result, further investigation and management such as endoscopy w not necessary unless any complications or indications arose.
The importance of accurate imaging and interpretation was also highlighted by this case. Radiographs, although often performed early, are not helpful due to the possibility of radiolucency of fish bones. As a result, CT investigations are increasingly used, and this helps reduce the gap between these common abdominal symptoms and the diagnostic uncertainty. We believe that this case highlights a form of observer error, specifically that of the satisfaction-of-search error, given the similarity of the patient’s symptoms to acute appendicitis and the ambiguous appearance of the appendix in the scan[17]. In such errors, As reported by Bathlaet al[3],the use of CT scans as diagnostic investigations are reliably sensitive in finding the lodged fish bone, with missed diagnoses often attributed to a lack of observer awareness. This was seen in this case and was similarly highlighted in other studies[3,18]. Fish bones were usually identified as either linear or curvilinear calcifications within the GI tract with associated inflammatory changes like fat stranding and/or a pneumoperitoneum[19]. Such changes of fat stranding were noted along the area of inflammation in this patient’s CT scan. Thus, the effective use and meticulous interpretation of CT imaging, along with detailed history tracing and correlation, can play a large role in narrowing the diagnostic dilemma when dealing with these conditions.
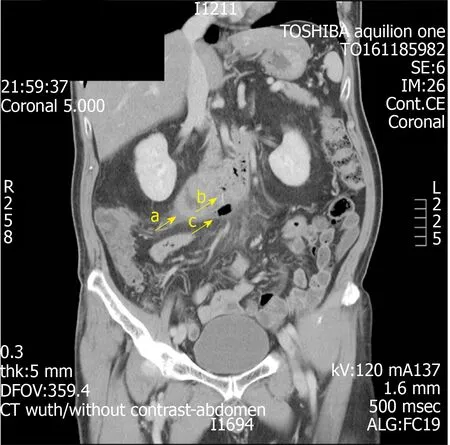
Figure 3 Computed tomography scan showing identified fishbone in the third segment of the duodenum measuring 1.4 cm long with associated air within the retroperitoneal space (arrow a). Local abscess was noted(arrow b). Area of gas out with the GI tract (arrow c).
CONCLUSION
This case report showcases the large diagnostic difficulty faced by clinicians when managing patients with upper GI microperforations, particularly those with symptoms that can mimic common conditions such as acute appendicitis. It displays the diagnostic and management process behind a patient with a fishbone-induced upper GI perforation can present with the classical symptoms of acute appendicitis and provides an additional differential diagnosis that can be considered. In addition,this case provides clinicians with a good example of the satisfaction-of-search error that can occur when interpreting straightforward presentations and emphasizes the importance of accurate radiological reporting and its roles in patient management and minimising patient morbidity. Concurrently, this case report also highlights the effectiveness of using CT imaging to identify fishbone embedment in patients with such symptoms and previous history of fishbone ingestion.
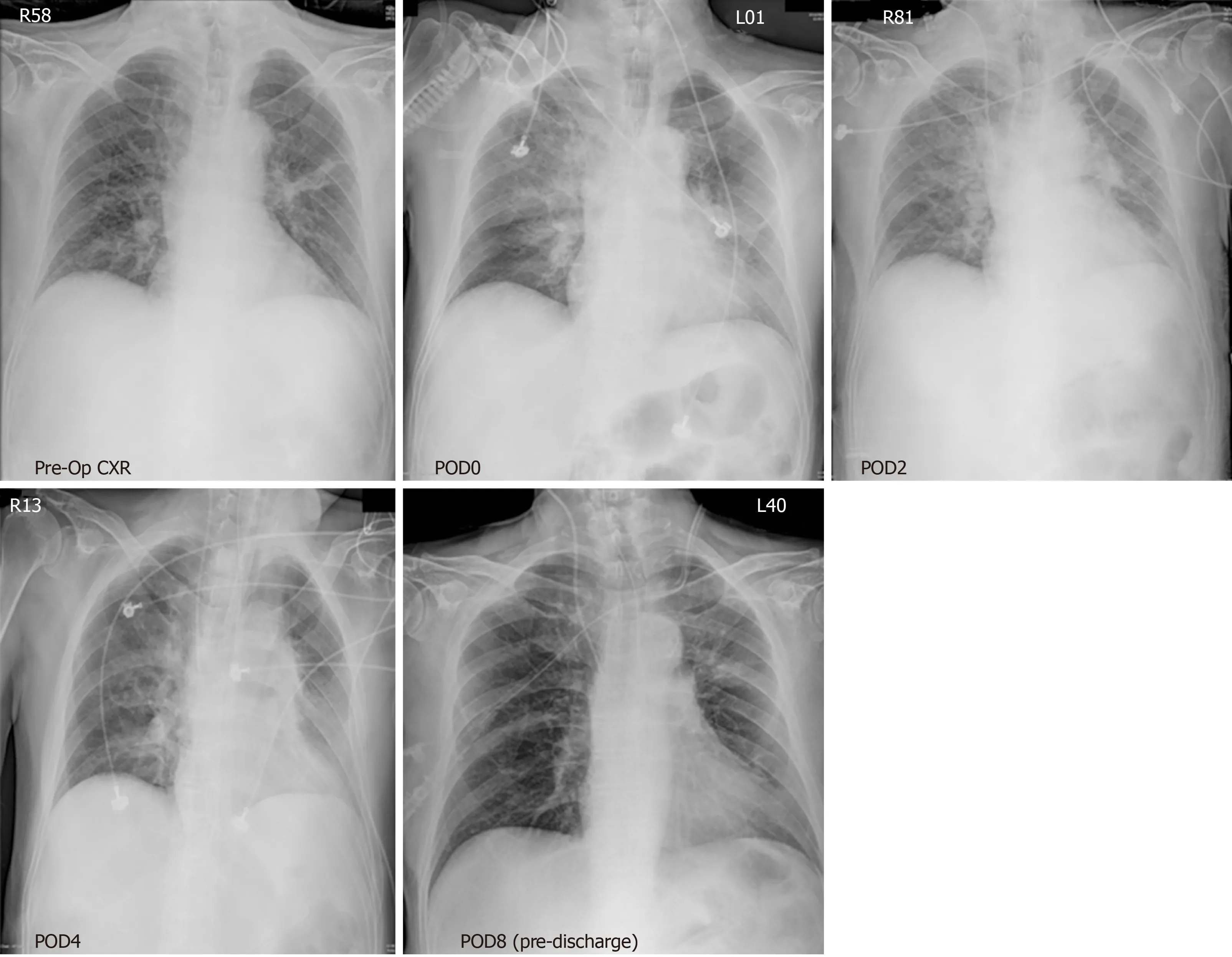
Figure 4 Serial chest radiographs showed acute consolidation and rapid resolution in his right lobe during the span of his inpatient stay. View from top left to bottom right. POD: Post-operative day.
ACKNOWLEDGEMENTS
Thanks to all our colleagues in the General Surgery and Radiology departments at National Taiwan University Hospital for their support and collaboration in the challenging diagnosis and management of this patient.
猜你喜欢
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Retrospective cohort study of statin therapy effect on resected colorectal liver metastases
- Hyponatremia is associated with more severe biliary disease
- Splenic injuries secondary to colonoscopy: Rare but serious complication
- Left hepatic trisectionectomy for perihilar cholangiocarcinoma with a right-sided round ligament: A case report
