Clinical characteristics and treatment of acute epiglottitis: A retrospective study of 28 cases
2020-05-21SantoshKumarSwainBuluNahakPriyankaDebtaDepartmentofOtorhinolaryngologyIMSandSUMHospitalSikshaAnusandhanUniversityK8KalinganagarBhubaneswar75003OdishaIndia
Santosh Kumar Swain, Bulu Nahak, Priyanka DebtaDepartment of Otorhinolaryngology, IMS and SUM Hospital, Siksha “O” Anusandhan University, K8, Kalinganagar, Bhubaneswar-75003, Odisha, India
2Department of Oral Pathology and Microbiology, IDS and SUM Hospital, Siksha “O” Anusandhan University, K8, Kalinganagar, Bhubaneswar-751003, Odisha, India
ABSTRACT
KEYWORDS: Acute epiglottitis; Airway obstruction; Supraglottis; Odynophagia
1. Introduction
Acute epiglottis (AE) is a potentially life-threatening infective condition where inflammation occurs at the epiglottis and the adjacent structures, consequently leading to airway obstruction. The most common pathogen causing AE is Haemophilus influenza (H. influenza) type B (Hib). Previously AE was seen more frequently among children, but nowadays the incidence of AE among pediatric age is reduced due to massive immunization against Hib[1]. AE in immunocompromised patients may be due to a wider variety of micro-organisms than immunocompetent patients, so besides impaired immunity, other risk factors for AE are elderly age, male sex, preexisting epiglottic cyst, obesity and impaired immunity of the host[2]. In addition, impaired immunity and epiglottic cysts have been reported to increase the risk for recurrent episodes of AE[3]. Adult patients with AE often have preexisting medical conditions such as diabetes mellitus, hypertension and alcohol abuse, which usually weaken the immunity of the patients and lead to susceptibility of the infections like AE[4]. The management of AE requires early diagnosis and treatment in order to avoid possible complications. Further, airway management and antibacterial treatment of the causative agent are vital for effective management. The aim of this study was to report the clinical profiles and management of the acute AE at a tertiary care teaching hospital in eastern India.
2. Participants and methods
2.1. Ethics approval
This study was approved by the Institutional ethical committee (IEC) with the reference number of IEC/IMS/SOA/21/2015, and informed consent was obtained from each patient.
2.2. Study design and participants
This retrospective study was conducted between January 2016 and October 2019 at a tertiary care teaching hospital in eastern India. This study was based on clinical observation of patients with AE. There were 28 patients of AE participated in this study. The diagnosis of AE was on the basis of the clinical presentations and direct visualization of the larynx with the help of the flexible fiberoptic laryngoscope. Clinical presentations, investigations, and treatment were documented in each case. All the clinical details of the participating patients were reviewed retrospectively. The clinical data like age, gender, clinical presentations, comorbidities, investigations, medical treatment, and intensive care unit requirements were assessed. The outcomes of the treatment in AE were also taken into consideration.
3. Results
In this study, the diagnosis of AE was based on the clinical history and otorhinolaryngological examination, and then the diagnosis was confirmed by nasopharyngolaryngoscopic examination which showed swollen cherry red appearance epiglottis in all patients (100%) (Figure 1). A total of 28 patients of AE participated in this study. Among them, 17 (60.71%) were male and 11 (39.29%) were female. The age ranged from 4 years to 62 years with a mean age of 23.45 years. Out of the 28 patients, 4 patients (14.29%) were confirmed cases of diabetes mellitus. The common symptoms presented by the patients included sore throat/throat pain (100%), odynophagia/painful swallowing (100%), fever in 19 cases (67.86%), a muffled voice in 16 cases (57.14%), pharyngo-cervical pain in 13 cases (46.43%), drooling of saliva in 12 cases (42.86%) and breathing difficulties in 4 cases (14.29%). Out of 4 cases of airway obstruction, 3 patients were associated with diabetes mellitus. The median duration from the onset of symptoms to the consultation to the physician is 3 d. The mean hospital stay was 5.1 d. Before hospitalization, 11 patients (39.29%) had already taken antibiotics. Out of the 28 patients, 6 patients (21.43%) showed edema of the hypopharynx, and 4 cases (14.29%) showed edema of the uvula. X-ray of the soft tissue of the neck (lateral view) showed swollen epiglottis (thumbprint sign) in all the cases of this study (Figure 2).
11月13日7版上方照片说明“一年一度的上马已成为申城一道亮丽的风景”,用“一年一度的‘上马'已成为……”为佳。
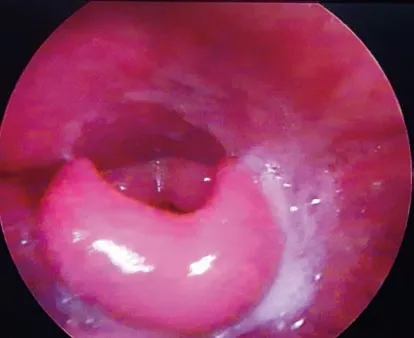
Figure 1. Endoscopic picture of the larynx showing congested and edematous epiglottis.

Figure 2. X-ray of the neck (lateral view) showing ‘thumbprint sign’ indicating inflamed and edematous epiglottis (yellow arrow).
Fiberoptic nasopharyngolaryngoscopy showed grossly swollen congested/reddish epiglottis in all cases, including 14 cases (50%) of extension of inflammation to the arytenoids, 11 cases (39.29%) of false vocal cords, and 7 cases (25%) of aryepiglottic folds. The temperature of the patients was ranging from 37.5 ℃ to 39.5 ℃ with a mean temperature of 38.2 ℃. Out of the 28 patients, 7 patients showed a high temperature exceeding 39 ℃. In pharyngeal cultures, 23 (82.14%) showed the existence of Hib, and the remnant showed no bacterial growth. In routine blood tests, the most constant finding was leucocytosis with neutrophilia, although it was only found in 16 (57.14%) patients. Blood culture was done in all cases of this study where only 3 cases showed positive culture for Haemophilus influenza and the rest were negative for any bacteria.
All the patients were treated with intravenous cefotaxime with appropriate doses along with corticosteroids and oxygen. Twelve patients were treated with intravenous corticosteroids. Four patients showed signs of respiratory distress, so they were transferred to the ICU. Out of the 4 patients in ICU, 3 underwent intubation and 1 underwent surgical tracheostomy for securing airway. All 4 patients received ventilator support along with the bag and mask en route to the hospital. Out of the four children, two were transported in an upright position. Besides ventilator support, the rest of the patients got oxygen with racemic epinephrine inhalation. Three of the patients underwent oro-tracheal intubation. One of them failed and then underwent emergency tracheostomy. One patient underwent cricothyroidotomy in the emergency department after orotracheal intubation safely proceeded. For the 4 ICU patients, the mean duration of ventilation support was 32 h (range from 16 h to 82 h). The treatment included intravenous administration of second or thirdgeneration cephalosporins along with corticosteroids and oxygen therapy. The choice of antibiotics changed to newer generation of cephalosporins. Cefotaxime was the frequently prescribed antibiotics in our cases of AE. The remaining 24 non-ventilatory support patients showed clinical improvement after one week of treatment. Out of 28 patients, 18 patients had intravenous lines. There was no catastrophic deterioration of breathing during the transports of the patients. Catastrophic deterioration of breathing was not documented one month after the treatment as well. All the patients were discharged without any squeal, and no deaths happened in this study.
4. Discussion
4.1. Clinical prof iles
AE is a life-threatening clinical entity and often associates with symptoms like sore throat and fever, followed by breathing difficulty[5]. The incidence of AE in adults is significantly higher than children in present-day and continues rising. The average age for adult groups is around 45 years with a male to female ratio as 1.8:1 to 4:1[6]. Similarly, more AE cases were seen in males than females in the present study. This fatal disease of the infected larynx may lead to sudden airway obstruction due to laryngeal edema which needs emergency treatment. Besides airway obstruction, other potentially serious complications possibly occur due to inflammatory response to the supraglottic region, so that AE also is a clinical entity of bacterial infection to the supraglottic structures, leading to the clinical symptoms such as sore throat, odynophagia, muffled speech/hot potato voice, fever, drooling of saliva and stridor. The patient may show signs of sepsis in the case of severe infections. Among the pediatric age groups, H. influenza is almost the invariable etiology associated with AE[7]. Other commonly identified pathogens in AE are group A streptococci and Streptococcus pneumoniae. Previously, 75% to 90% of the cases were due to Hib, but after the introduction of the vaccination against Hib in 1985, the incidence of AE significantly decreased[5]. In the adult age groups, however, H. influenza is not the sole pathogen for supraglottic infection, Streptococcus pneumoniae, hemolytic streptococci, and Staphylococcus aureus are also seen in the throat or blood culture samples[8]. So, although the Hib vaccinations significantly declined the incidence of AE among pediatric groups, the incidence continues increasing among adults[4]. In post-vaccination era, the annual incidence of pediatric acute epiglottitis declined to 0.3 to 0.7 per 100 000 patients[9].
The clinical presentations of AE include odynophagia, sore throat, fever, breathing difficulties and tenderness of anterior neck[10]. In this study, sore throat and odynophagia were seen in all cases of AE. Unlike in adult patients, the examination of the larynx with an indirect laryngoscope or laryngeal fibroscope is usually avoided in pediatric patients as these maneuvers often trigger an acute obstruction of the laryngeal airway[11]. AE may be associated with edemas in other parts such as uvula, tongue, oral cavity and hypopharynx[12]. It has been documented that AE is more commonly found in summer, early spring and late autumn[13,14]. But other study shows no predilection of time or season[15]. The most common duration from onset to visiting the physician is 2 to 3 d[16]. In our study, the duration of 3 d (median) was noted. AE is sometimes a self-limiting disease with an increased chance of developing a rapid and fulminant course. An epiglottic abscess is considered as an uncommon sequel of the AE. As the manipulation of the oropharynx and nasopharynx might provoke complete airway occlusion, so a conservative airway protocol is required in cases of mild and moderate symptoms, and anticipate airway obstruction during managing AE is an important part of patient care. If a patient presents with breathing difficulties, he or she often lean forwards with outstretched arms into a tripod position, which helps to reduce chocking sensation as swollen and edematous epiglottis move forward. This tripod position is an impending sign for airway obstruction in AE[17]. There are other four predictors for impending airway obstruction such as drooling, history of diabetes mellitus, rapid onset of the clinical symptoms and abscess formation[18]. In our study, airway obstruction indicated the relationship with diabetes mellitus. Additionally, adults have less likelihood of sudden airway obstruction in comparison to children. The complications of AE are retropharyngeal abscess, cervical necrotizing fasciitis, sepsis and sudden airway obstruction with pulmonary edema[19]. In this study, no such complications are found. The mortality rate in AE is reported to be 6% to 7% among adult groups in comparison to 1.6% in the pediatric groups[20]. The difference between adults and pediatric groups is probably due to the high rate of misdiagnosis and inappropriate treatment among adults[13].
4.2. Diagnosis
Diagnosis methods include direct laryngoscopic examinations and imaging. Direct manipulation of the larynx should be avoided as it can lead to rapid airway compromise. In AE cases, the direct fiberoptic laryngoscopic examination of the larynx shows inflamed edematous epiglottis. In some cases, direct laryngoscopy shows diffuse erythematous swelling of the epiglottis, aryepiglottic folds and pooling of saliva in the pyriform sinus. Radiographic imaging like lateral neck X-ray and CT scan can be helpful for the diagnosis of the AE especially among patients showing signs of airway obstruction. In AE cases, the lateral view of the X-ray of neck shows a classical “thumbprint sign” that is the evidence of swollen epiglottis. However, the use of fiberoptic nasopharyngolaryngoscopy must follows a more confirmatory and faster way for assessing the laryngeal airway, as the imaging may be delayed during evaluation of the patients. So after the patient becomes stable or in sub-acute presentations, the imaging may be indicated for evaluation of the AE and its differential diagnosis[21]. However, the gold standard investigation is direct expert laryngoscopy[10,22]. In addition, CT scan will show diffuse thickening of the epiglottis and aryepiglottic folds in AE cases,.
4.3. Treatment
When the patient is suspected of AE, it is necessary to refer the patient for a high dependency unit like a resuscitation room along with emergency airway equipment nearest to the patient’s trolley. The patient will be started with immediate airway, breathing, and circulation with a high flow of oxygen and intravenous access. Arterial blood gas analysis, full blood count and blood cultures help to take decisions towards the requirement for intubation and the following treatment, but they are not often helpful to confirm the diagnosis immediately. Blood cultures were taken from all of our patients among which 25 cases (89.28%) did not show any growth of the bacteria, and these findings are consistent with the study by Berger et al.[23] where 16 out of 17 patients did not show any growth of the bacteria. Otherwise, patients of AE show leucocytosis with a higher white blood cell (WBC) count. Therefore, WBC count may serve as an effective screening parameter for the diagnosis of AE.
The essence of management of AE is to safeguard the patient’s airway and decrease the incidence of airway obstruction. The treatment of AE includes intravenous broad-spectrum antimicrobial agents with additional corticosteroids for reducing inflammation and edema of the supraglottic[24]. The second and third-generation cephalosporins (ceftazidime or cefotaxime) along with corticosteroids, omeprazole and/or oxygen therapy are often administrated in common AE cases. The third generation intravenous cephalosporins are administered in ICU patients who are not allergic to beta-lactams. In addition, supplementation of hydration and 30% humidified oxygen should be administered through a facemask to ease labored breathing. Corticosteroids are often administered for reducing the edema and inflammation of the supraglottic and airway obstruction. Intubation or tracheostomy may be required in the case of AE with stridor due to the collapsed airway. In the case of abscess formation along with AE, surgical drainage or debridement is also required. Isolated necrosis of the supraglottic may be seen in some cases, and early debridement of the necrotic tissue along with medical treatment are needed in this situation[24]. During the hospital stay, arterial oxygen saturation of the patient should be continuously monitored with finger pulse oxymetry. According to the treatment protocol of AE, glottic and supraglottic airway should be assessed by an otolaryngologist through a flexible fiberoptic laryngoscopy and find out whether the airway is patent or compromised. The decision for securing the airway is made on the basis of the clinical symptoms and airway appearance. In the case of respiratory difficulties like stridor, oxygen desaturation, cyanosis and sitting erect, airway intervention is required immediately. In some situations where patients lack symptoms and signs of airway obstruction but with narrowed airway at least of 50%, the fiberoptic laryngoscope is also needed. The causes for the latter protocol are due to the fickle nature of the disease which can land on imminent respiratory distress at any time. When the condition is feasible, patients of AE should be shifted to the operating room for endotracheal intubation to maintain the airway. If endotracheal intubations fail after repeated attempts, tracheostomy or cricothyrotomy should be performed. After securing the airway, patients are usually transferred to the ICU. Those patients of AE with patent laryngeal airway will be hospitalized with closely supervised by an otolaryngologist and trained staff nurse.
5. Conclusion
AE is an infectious condition, which requires early diagnosis and prompt treatment to avoid life-threatening complications, like airway obstruction. Introduction of the flexible fiberoptic nasopharyngolaryngoscope turns the visualization of the larynx and assessment of possible compromised airway into a more accurate task than just relying on soft tissue lateral X-ray of the neck. In this study, we examined 28 patients of AE who were admitted and managed promptly without any complications.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contribution
S.K.S.: Concept, study design, patient datas, data collections, data analysis and drafting; B.N.: Data collection and data analysis; P.D.: Data collection, data analysis and drafting.
猜你喜欢
杂志排行
Journal of Acute Disease的其它文章
- Knowledge, attitude, and practice towards coronavirus disease 2019 (COVID-19) among medical students: A cross-sectional study
- Factors affecting outcomes of surgically treated patients with cranial extradural hematoma: A cross-sectional study
- Aberration detection of pertussis from the Mazandaran province, Iran, from 2012 to 2018: Application of discrete wavelet transform
- Identification of Panton-Valentine leukocidin virulence gene in methicillinresistant Staphylococcus aureus isolated from clinical specimens of burn patients in Zare Hospitals of Sari, Iran
- Successful treatment of hepatic hydrothorax: A case report
- Suicide attempt of an overt hypothyroid patient with levothyroxine: A case report
