Endoscopic ultrasonography elastography in the diagnosis of intrapancreatic ectopic spleen:A case report
2020-05-13NanGeSiYuSun
Nan Ge, Si-Yu Sun
Nan Ge, Si-Yu Sun, Department of Gastroenterology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
Abstract
Key words: Intrapancreatic accessory spleen;Endoscopic ultrasonography;Elastography;Case report
INTRODUCTION
The identification of incidental pancreatic lesions is increasing due to advancements in imaging.Diagnosis remains a challenge for clinicians, with intrapancreatic accessory spleen (IPAS) posing a unique dilemma.IPAS mimics a pancreatic neoplasm on imaging studies, and due to the lack of radiological diagnostic criteria,patients undergo unnecessary distal pancreatectomy.Endoscopic ultrasonography(EUS) is one of the most reliable and efficient diagnostic modalities for pancreatic diseases.However, no EUS criteria have been established for IPAS.The use of EUSelastography may increase diagnostic accuracy.Herein, we present the EUSelastography image of IPAS.
CASE PRESENTATION
Chief complaints
A 50-year-old male patient was referred from the surgery department for an EUS evaluation after a computed tomography scan showed a 1.4-cm round hypervascular enhanced mass in the tail of the pancreas, which indicated a neuroendocrine neoplasm (Figure 1).
History of present illness
Initially, the mass was found following a computed tomography examination during his regular medical examination.The patient did not complain of any symptoms.
History of past illness
He has no specific history of past illness.
Personal and family history
He has no specific personal or family history.
Physical examination upon admission
The patient did not have positive signs on physical examination.
Imaging examinations
EUS revealed a 1.2 cm × 1.3 cm, round, well-defined homogenous hypoechoic mass in the pancreatic tail with no other endosonographic pancreatic abnormalities (Figure 2).
EUS elastography was performed and it was found that the lesion covered no more than 25% of the region of interest.To assess the quality and reproducibility of the elastography image, the image was frozen and the stored cine loop was reviewed frame by frame.A consistent color pattern obtained in a number of consecutive frames indicating a good, reliable technique.
The lesion showed a heterogeneous, predominantly green pattern with slight yellow and blue lines, indicating a soft texture (Figure 3).
Real-time tissue quantitative elastography with strain ratio (SR) measurement was also performed.Region of interest A was placed within the pancreatic tail mass and region of interest B in the adjacent parenchyma.An SR (B/A) of 0.74 indicated the softer elasticity of the lesion compared with the surrounding normal pancreatic tissue(Figure 4).
FINAL DIAGNOSIS
The patient was finally diagnosed with IPAS.
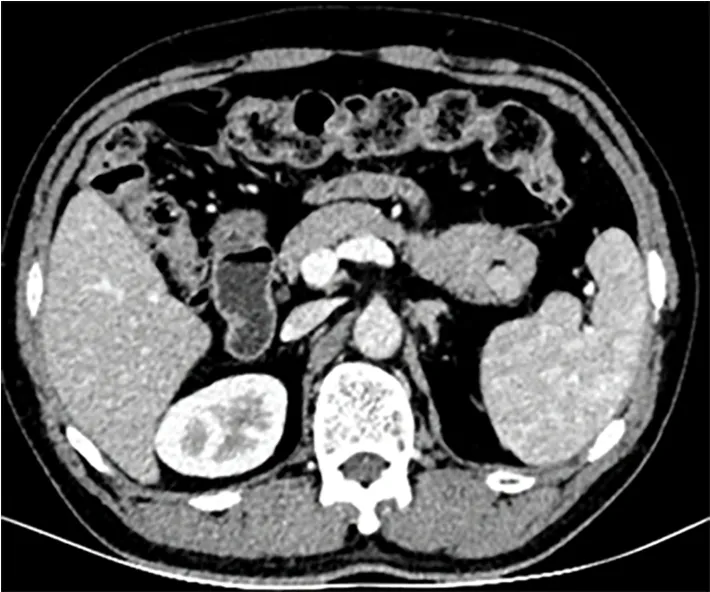
Figure 1 Computed tomography image of the intrapancreatic accessory spleen.
TREATMENT
The patient underwent distal pancreatectomy as initial CT indicated a neuroendocrine neoplasm.
OUTCOME AND FOLLOW-UP
Pathological evaluation of the resected tissue showed a 1.3-cm nodule with a complete capsule in the pancreatic tissue, and the nodule was composed entirely of spleen tissue.The final diagnosis was IPAS.The patient had no adverse effects after surgery.
DISCUSSION
Accessory spleen is a congenital failure of splenic bud fusion during embryogenesis,which is revealed in about 10%-30% of autopsies[1].In most cases, accessory spleens are located near the splenic hilum.The second most common site is the pancreatic tail(17%).IPAS can mimic intrapancreatic tumors, such as neuroendocrine neoplasms[2-4].IPAS is often misdiagnosed as a neuroendocrine neoplasm and treated with distal pancreatectomy.However, asymptomatic IPAS does not require medical treatment, or even surgical resection.
It is important to provide accurate preoperative differential diagnostics to prevent patients undergoing unnecessary surgery.
EUS has high resolution and is considered one of the most reliable and efficient diagnostic modalities for pancreatobiliary diseases[5-7].
Elastography is a new technique for tissue characterization, providing a noninvasive modality for imaging the mechanical properties of tissue[8].EUS elastography is able to better characterize lesions by tissue stiffness evaluation in various locations which are only accessible from the gastrointestinal tract.Elastography can be adjunct to the EUS examination due to its ease of use,noninvasiveness, and low cost.
EUS elastography for the evaluation of pancreatic tissue was first reported in 2006.The pooled sensitivity and specificity of EUS elastography from 15 studies were 93%and 63%, respectively[9].Most malignant pancreatic lesions appear stiff in elastography[10].It is also reported that in patients with small solid pancreatic lesions,EUS elastography can play an important role in ruling out malignancy if the lesion appears soft[11].
Based on qualitative elastographic evaluation, up to 4 well-defined patterns have been described that characterize solid pancreatic lesions and contribute to their classification:A homogeneous green pattern present commonly in the normal pancreas;a heterogeneous, predominantly green pattern with slight yellow and red lines present only in inflammatory pancreatic masses;a heterogeneous,predominantly blue pattern with small green areas and red lines and a geographic appearance present mainly in pancreatic malignant tumors (including pancreatic adenocarcinoma);and a homogeneous blue pattern present only in pancreatic neuroendocrine malignant lesions[12].Giovanniniet al[13], using this qualitative evaluation, reported that the sensitivity and specificity for malignancy were 100% and 67%, respectively.In our case, the lesion showed a heterogeneous, predominantly green pattern with slight yellow and blue lines on qualitative elastographic evaluation, which may exclude pancreatic malignant tumors or neuroendocrine malignant lesions.
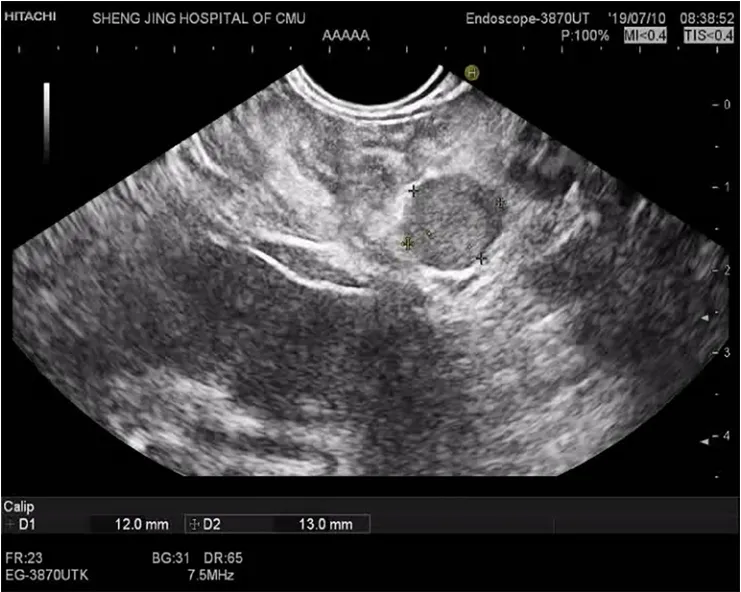
Figure 2 Endoscopic ultrasonography image of the intrapancreatic accessory spleen.
SR calculation is based on standard qualitative EUS elastography data[14].Two different areas (A and B) are selected for quantitative elastographic analysis.Area A is selected including as much of the target lesion as possible without including the surrounding tissues.Area B is selected within a soft reference area outside the target lesion.The SR is calculated as the quotient of B/A.In the past few years, several studies have been conducted to determine the accuracy of SR for detecting malignancies.Different cut-off values have been defined, from 3.7 to 24, with sensitivities ranging from 67% to 98%, and specificity ranging from 45% to 71%[15-20].In our case, an SR of 0.74 indicated the soft texture of the lesion, which is seldom found in pancreatic malignant tumors or neuroendocrine malignant lesions[12].When we reviewed the video of the EUS examination, we noticed that this pancreatic tail lesion also had an echogenicity similar to the adjacent spleen tissue.
Recently, Bhutaniet al[21]reported that the “bridge sign” in EUS images may differentiate IPAS from a pancreatic neuroendocrine tumor, which could save the patient an EUS-fine needle aspiration, diagnostic confusion, surgery, anxiety, and healthcare dollars.Therefore, when combined with EUS-elastography, IPAS may not be misdiagnosed by EUS in the future.Moreover, unnecessary surgery and other invasive intervention may be avoided, similar to the current irreplaceable role of EUS diagnosis of gastric ectopic pancreas.
CONCLUSION
IPAS is a relevant differential diagnosis in patients with suspected pancreatic neuroendocrine tumors of the pancreatic tail, which should be considered before surgery is undertaken.Non-invasive differentiation between IPAS and pancreatic neuroendocrine tumors can be provided using EUS-elastography.
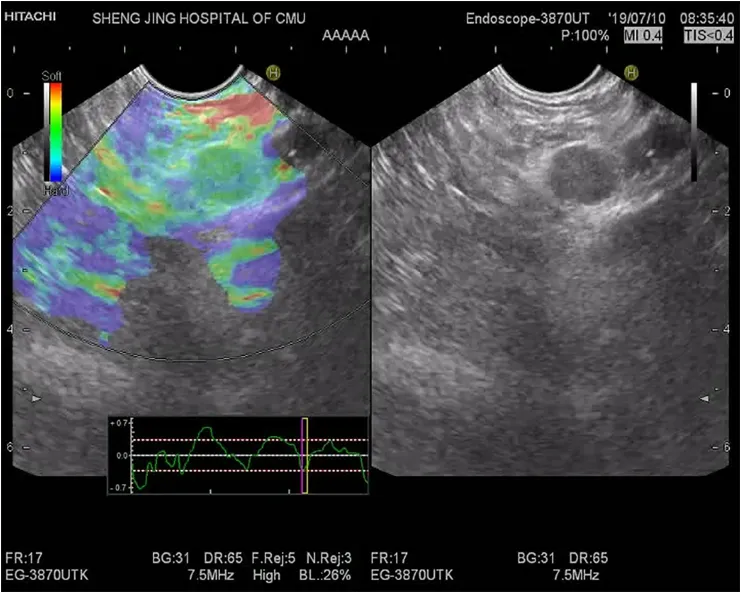
Figure 3 Qualitative elastographic evaluation image of the intrapancreatic accessory spleen.
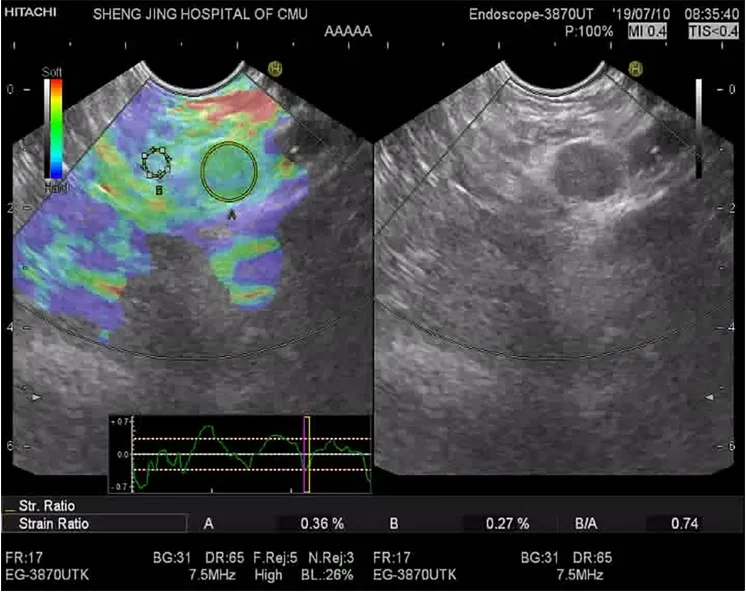
Figure 4 Strain ratio evaluation of the intrapancreatic accessory spleen.
杂志排行
World Journal of Clinical Cases的其它文章
- Rare primary lymphoepithelioma-like carcinoma of the renal pelvis
- Portal hypertension in a patient with biliary hamartomas:A case report
- Mesonephric adenocarcinoma of the uterine cervix with rare lung metastases:A case report and review of the literature
- Giant ventral hernia simultaneously containing the spleen, a portion of the pancreas and the left hepatic lobe:A case report
- Application of curved ablation in liver cancer with special morphology or location:Report of two cases
- COVlD-19 managed with early non-invasive ventilation and a bundle pharmacotherapy:A case report