Provincial clustering of malaria in Iran between 2005 and 2014
2020-05-10VahidMoqarabzadehAhmadAliEnayatiAhmadRaeisiFatemehNikpourJamshidYazdaniCharati
Vahid Moqarabzadeh, Ahmad Ali Enayati, Ahmad Raeisi, Fatemeh Nikpour, Jamshid Yazdani Charati
1Department of Biostatistics & Epidemiology, School of Health, Mazandaran University of Medical Sciences, Sari, Iran
2Medical Entomology, Mazandaran University of Medical Sciences, Sari, Iran
3Department of Medical Entomology and Vector Control, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
4Department of Environmental Chemical Pollutants and Pesticides, Institute for Environmental Research, Tehran University of Medical Sciences, Tehran, Iran
5Department of Biostatistics, Health Sciences Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran
ABSTRACT Objective: To reveal the provincial clustering of malaria in Iran between 2005 and 2014 based on the epidemiologic factors and the climatic indicators affecting the disease.Methods: This was a descriptive-analytical study using malaria and meteorological data from the Malaria Elimination Programme of the Ministry of Health and Medical Education and National Meteorological Organization. After standardization, the aggregate data was used to produce 10-year means for each province. The data analysis included grouping the provinces with respect to factors using hierarchical clustering method and Kruskal-Wallis test to examine the difference between clusters using SPSS ver.23.Results: The hierarchical clustering stratified the provinces’ in 5 clusters. Kruskal-Wallis H test revealed a significant difference in the incidence rate per 100 000 population (P=0.001), male gender (P=0.001), Iranian nationality (P=0.001), Afghan nationality (P=0.003), Pakistani nationality (P=0.001), urban residence (P=0.006), rural residence (P=0.004), autochthonous cases (P=0.007), average minimum temperature (P=0.001), average maximum temperature (P=0.007), average relative humidity (P=0.011), average pressure level (P=0.038), prevailing wind direction (P=0.023), average wind speed (P=0.031) and average precipitation sum (P=0.002) among the clusters.Conclusions: The results of this study and stratification of the provinces could help health policy makers to better manage malaria by allocating resources accordingly.
KEYWORDS: Malaria; Cluster analysis; Iran
1. Introduction
Malaria is an infectious disease transmitted by Anopheles mosquitoes. WHO Global Malaria Report indicates that in 2016, approximately 216 million malaria cases and 429 000 death were reported worldwide. About 90% of the cases are in Africa and 2% in the Eastern Mediterranean Region. Iran observed a reduction of 49% in the indigenous malaria cases transmission in 2016 compared to that of 2015[1].
Declining pattern of malaria transmission in Iran has been consistent with malaria incidence decrease, moving from West to East and from North to South. The transmission risk for Plasmodium (P.) falciparum was significantly lower than that of P. vivax and moreover the incidence rate of P. falciparum in endemic areas decreased faster than incidence rate of P. vivax[2].
Despite all the problems and challenges in malaria endemic areas in Iran, malaria incidence declined in these areas[3-5]; however, no disease has incurred such financial burden, irreversible costs, and loss of life in Iran as malaria. Three provinces, namely, Sistan-Baluchistan, Kerman and Hormozgan had the most reported cases of local transmission of the disease in recent years[4-8].
Cross-border infection especially from Afghanistan and Pakistan has created challenges in controlling malaria in Iran[9]. Despite the declining trend of malaria cases in recent years, paying attention to local transmission event, especially in the border provinces is highly significant[6], thus malaria elimination interventions focus on highrisk groups and based on the incidence peaks[10].
Malaria Local Transmission Elimination Program was approved in 2010 by the government of Iran. This program has been designed in two phases, a pre-elimination phase until 2014 and the disease elimination stage until 2025. The goals of the program have been to eliminate the local transmission of P. falciparum until 2018, P. vivax until 2022 and to obtain the elimination certificate from the World Health Organization until 2025[5,11,12].
Many factors influence malaria transmission and incidence rate. Taking the most important factors into account and recognizing the potential factors, and grouping the provinces based on the influencing factors in the areas where these factors are homogeneous seem necessary for determining the required interventions and measures in order to control and eliminate local transmission of the disease as quickly as possible. There is not much information and documentation available about the structure of the probable groups on the factors affecting the transmission of malaria. Therefore, the present study was designed pursuing the goal to discover the existing structure in the country provinces’ grouping during 2005-2014 based on the epidemiologic factors and the climatic indicators affecting the disease. Accurate grouping of the provinces regarding the influencing factors can highly improve elimination planning by malaria program with respect to the homogeneous provinces in terms of the disease incidence, sufficient budget allocation for the homogeneous groups and the identification of the potential incidence areas.
2. Material and methods
2.1. Study area
Iran is located in southwest Asia (the Middle East) with an area of 1 858 195 km2, neighboring Afghanistan and Pakistan in the East, Turkmenistan in the Northeast, the Caspian Sea in the Mid North, Azerbaijan and Armenia in the Northwest and Turkey and Iraq in the West. In the South, the Persian Gulf and the Oman Sea are between Iran and the Persian Gulf states. Iran is considered as one of the countries of the Eastern Mediterranean Region in the World Health Organization division, with 31 provinces and based on 2015 census, its population was reported to be 78.77 million.
2.2. Malaria data
Malaria data used in this study were collected during 10 years from 2005 to 2014 (21 March 2005 to 20 March 2014) from Iran Malaria Elimination Program of the Center of Diseases Control, Ministry of Health and Medical Education. The aggregate data include the incidence level per province, the frequency of parasite type, gender frequency, nationality frequency, residence frequency and the transmission epidemiology frequency of the infected people. The population data by year and province was extracted from the website of Iran Statistics Center.
2.3. Meteorological and demographic data
The meteorological data during 2005 to 2015 for each province was obtained from Iran Meteorological Organization. The data consisted of average minimum temperature, average maximum temperature, and average humidity level, average pressure of the station, prevailing wind direction, average wind speed and average annual precipitation sum.
2.4. Data preparation
Malaria data were determined as the incidence and percentage (parasite type, gender, nationality, residence and epidemiology) by each province for 10 years. The meteorological data for this analysis was estimated as the mean climatic indicators by each province during 10 years.
2.5. Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee of Mazandaran University of Medical Sciences with grant number of IR.MAZUMS.REC.96.2953 and written informed consent agreement obtained from all participant.
2.6. Statistical analysis
This was a descriptive analytical study. Data analysis was performed in two steps. In the first step, the data was grouped using hierarchical clustering method based on the epidemiological and climatic variables. The provinces grouped in each cluster are homogeneous with each other as much as possible and clusters or groups differ from each other as much as possible[13].
Since the clustering technique is of non-monitored analysis classes, the number of the groups is determined using the squared-proximity size of the Euclidean distance as well as the mental pattern using a dendrogram[14].
In the second step, characteristics of identified clusters were described using median (IQR) (because of normal distribution assumption of data was violated). In addition for comparing identified clusters, Kruskal-Wallis H nonparametric tests were applied.
All descriptive techniques and statistical tests were performed using SPSS ver.23 software and the significance level for all tests was considered 0.05.
ArcGIS9.2 was used to map the provinces in the clusters identified by the hierarchical clustering method.
3. Results
3.1. Malaria incidence in Iran during 2005-2014
The total incidence rate of malaria in 100 000 persons during 2005-2014 was 10.486 (total number of cases 60 875) with the highest burden in Sistan and Bluchestan, Hormozgan and Kerman Provinces respectively. The malaria incidence had a decreasing trend during this period and dropped from 26.483 in 2005 to 1.041 in 2014 per 100 000 persons, showing a decline of 96.07%.The statistical analysis results of the average incidence level per 100 000 persons is shown in Figure 1.
3.2. Provincial clustering of malaria incidence in Iran
The parasite type ratio, gender ratio, nationality ratio, residence ratio, epidemiology ratio, average minimum temperature, average maximum temperature, average relative humidity, average temperature pressure, prevailing wind direction level, average wind speed and average annual precipitation sum were given in dendrogram (Figure 2).
Based on the dendrogram, according to the Ward’s method and considering the squares Euclidean distance based on the existing variables and their standardization, five clusters were defined with 3, 11, 13, 3 and 1 province(s) respectively. The 1st cluster is an endemic area of malaria. The 2nd cluster consists of industrial provinces and metropolises. Provinces with cold weather and very low local transmission of malaria are in the 3rd cluster. The Northern provinces of Iran, provinces that are climatically humid and with heavy rainfall, are in the 4th cluster, and finally the 5th cluster (Ilam), is the only cluster with one province in which no malaria positive cases were reported (Table 1).

Figure 1. Map of Iran with clusters of provinces for malaria based on the hierarchical clustering method using meteorological and epidemiological factors between 2005 and 2014. Sequentioal scheme shows incidence rate data for each cluster as a color from low to high, accenting the lowest as a light shade (5th Cluster) and the highest as a dark shade (1st Cluster). MAR: Markazi, ALB: Alborz, FAR: Fars, YZD: Yazd, SEM: Semnan, ISF: Isfahan, BUS: Bushehr, KHU: Khuzestan, TEH: Tehran, KHR: Khorasan Razavi, QOM: Qom, S & B: Sistan and Bluchestan, KER: Kerman, HOR: Hormozgan, ILAM: Ilam, MAZ: Mazandaran, GOL: Golestan, GIL: Gilan, QAZ: Qazvin, K&B: Kohgiluyeh and Boyer-Ahmad, LOR: Lorestan, CH & B: Chahar Mahaal and Bakhtiari, KUR: Kurdestan, HAM: Hamadan, ARD: Ardabli, KHN:Khorasan North, AZE: Azerbayjan East, KHS: Khorasan South, AZW: Azerbayjan West, KSH: Kermashah, ZAN: Zanjan.

Figure 2. Hierarchical clustering dendrogram of the 31 provinces of Iran based on Ward’s method. MAR: Markazi, ALB: Alborz, FAR: Fars, YZD: Yazd, SEM: Semnan, ISF: Isfahan, BUS: Bushehr, KHU: Khuzestan, TEH: Tehran, KHR: Khorasan Razavi, QOM: Qom, S & B: Sistan and Bluchestan, KER :Kerman, HOR: Hormozgan, ILM: Ilam, MAZ: Mazandaran, GOL: Golestan, GIL: Gilan, QAZ: Qazvin, K&B: Kohgiluyeh and Boyer-Ahmad, LOR: Lorestan, CH & B: Chahar Mahaal and Bakhtiari, KUR: Kurdestan, HAM: Hamadan, ARD: Ardabli, KHN: Khorasan North, AZE: Azerbayjan East, KHS: Khorasan South, AZW: Azerbayjan West, KSH: Kermashah, ZAN: Zanjan.
3.3. Comparison of malaria incidence identified clusters
Clusters of provinces based on the mean 10 years epidemiological and meteorological factors identified by colors are shown in the map of Iran (Figure 1).
According to the results, the incidence level per 100 000 (P=0.001), male gender (P=0.001), Iranian nationality (P=0.001), Afghan nationality (P=0.003), Pakistani nationality (P=0.001), urban residence (P=0.006), rural residence (P=0.004), autochthonous cases (P=0.007), average minimum temperature (P=0.001), average maximum temperature (P=0.007), average relative humidity (P=0.011), average pressure level (P=0.038), prevailing wind direction (P=0.023) and average precipitation sum (P=0.002) showed statistically significant difference using Kruskal-Wallis test (Table 1).
In addition, the mean incidence level in the 1st cluster, including three malaria endemic provinces, is much higher than the other 4 clusters. In all clusters, the P. vivax cases were the highest followed by P. falciparum and mix infection. In all clusters, percentage of men predominates women. The infected individuals in the 1st, 3rd and 4th clusters are mainly Iranian, while in the 2nd cluster, around two thirds of them are of Afghan nationality. In the 1st cluster, about two thirds of the positive cases belong to villages, on the contrary, this ratio is exactly the opposite in the 2nd cluster. In the 3rd and 4th clusters, the urban and rural infection rates did not show any significant difference. The average 10-year local and introduced cases rates in the 1st cluster are at the same level, while in the 2nd, 3rd and 4th clusters, the highest average belongs to the introduced cases (Table 1).
Climatic characteristics of the 1st cluster include high temperature, low humidity, high dominant wind direction and low mean of annual precipitation. The 3rd cluster identified by its cold provinces. Northern provinces of Iran, provinces with high annual average precipitation sum, high humidity average and the highest average pressure level are in the 4th cluster (Table 1).
4. Discussion
Clustering in the present research has been done using the ratio of the epidemiological factors and the mean meteorological factors, and five clusters with 3, 11, 13, 3 and 1 provinces were determined. In all clusters, P. vivax was the most prevalent species in malaria infected cases, and males had higher infection rate than females, being equal with the disease pattern all over Iran. Gender does not influence malaria infection directly, and the high percentage of male infection can be due to working outdoors, attending higher risk environments and also their clothing type[4,15,16]. The results suggest that in the 1st cluster, the average incidence rate per 100 000 persons is significantly higher than this indicator in other clusters, while in the remaining, the average incidence rate is lower than two per 100 000 persons. The 1st cluster includes malaria endemic provinces with relatively high incidence rates, the infection rates in females significantly differ from the females in other clusters. In this cluster, rural infection rates and in females are higher compared with other clusters because in villages, women participate in daily activities along with men, thus increasing the probability to get infected for female increases. The high incidence rate of Pakistani nationality in this cluster can be attributed to legal and illegal immigrants from neighboring Pakistan. The higher infection rate of rural residents is also due to the suburban and rural nature of the disease. Of the climatic factors, higher average minimum and maximum temperatures, higher prevailing wind direction and average lower annual precipitation sum can be mentioned in this cluster.
Based on the literature, malaria incidence rate is higher in the Southern and Southwestern areas of Iran in recent years and the local transmission were higher in these provinces. In the other studies, the disease prevalence rates in Southern Iran were higher in villages than cities, consistent with the results of our study[10,17-20]. The majority of these areas are climatically warm and humid, and the temperature is the most important climatic factor affecting malaria incidence in the Southern and Southeastern endemic areas of Iran. Moreover, the analyses demonstrated that precipitation factor is inversely associated with the disease incidence rate[18,21,22]. Males showed a high infection rate in the 1st cluster, the proportion of infected women in this cluster was higher than that in other clusters, in accord with a similar study[22]. Although malaria endemic level is relatively low in Iran compared with some malaria endemic countries in the Eastern Mediterranean Region, there is a high risk of malaria transmission in Southern and Southeast parts of the country[23].
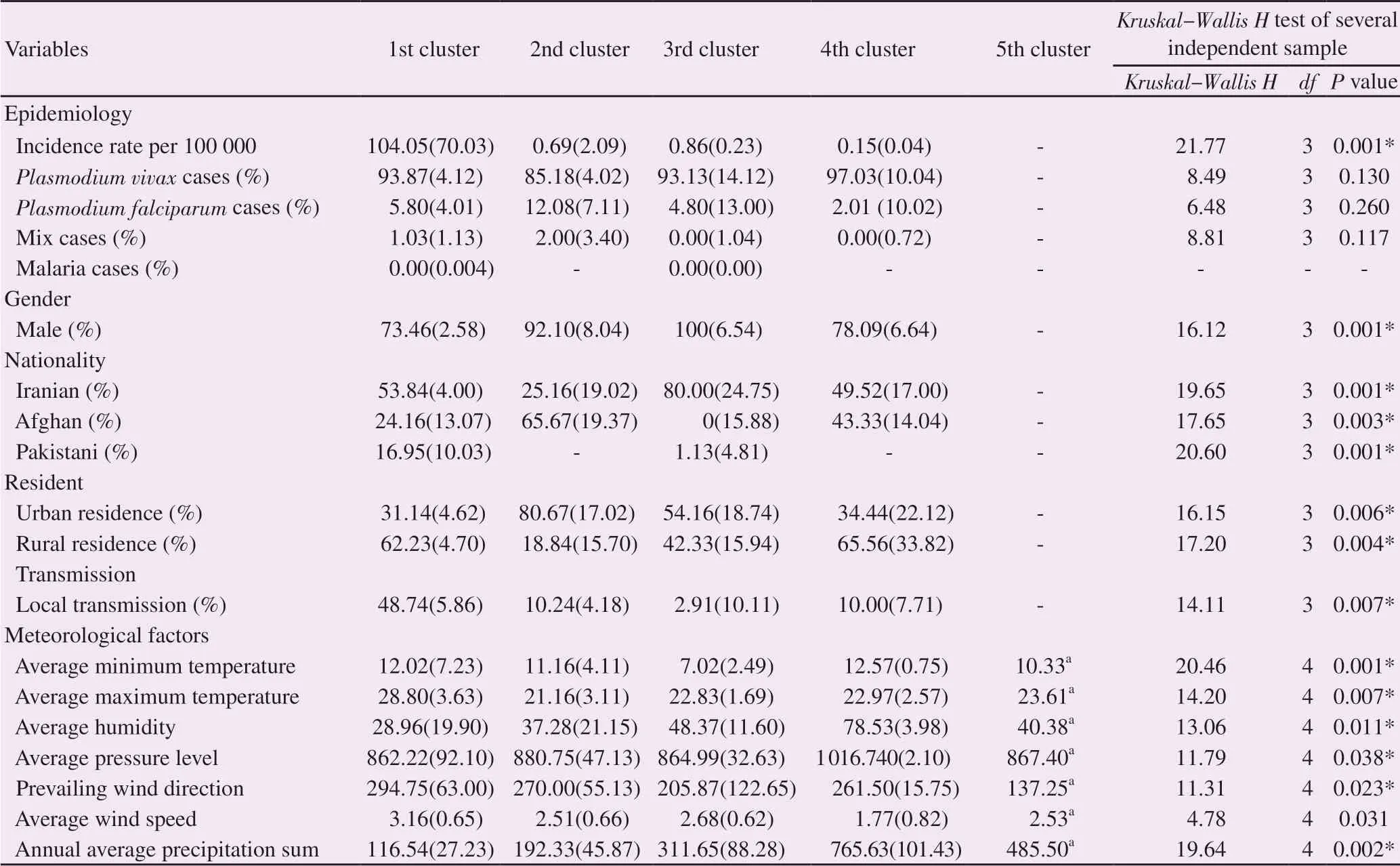
Table 1. Comparing identified malaria provincial clusters in Iran by meteorological and demographic characteristics between 2005 and 2014.
The 2nd cluster in which more industrial and touristic provinces are located, the mean incidence rate is around 2 per 100 000 persons. Approximately 85% of the malaria cases in this cluster are of the introduced type, indicating malaria being non-endemic in these provinces, finding in accord with the result of similar studies[24,25]. Also, the high percentage of non-Iranian malaria cases is around 75% the majority of which are of Afghan nationality (61.48%). The majority of the provinces of the 2nd cluster are either industrialized or touristic with close proximity to the endemic provinces, conditions causing higher immigration of work force (Afghan nationals as well as from the endemic provinces) to these provinces, some of the reasons behind high non-Iranian infection cases in this cluster, a finding that is compatible with other studies[24-28]. In this cluster, about 80% of the infection cases are city dwellers and most of the cases in this cluster are of the introduced type the reason of which can be attributed to higher work opportunities and the presence of more Afghan workers in the cities and also more tourist attractions in the cities[15,24]. Average high minimum and maximum temperature, low relative humidity, relatively high prevailing wind direction and low average annual precipitation sum are among the climatic factors of this cluster.
The incidence rate in the 3rd cluster is negligible, average percentage of P. vivax cases is higher than other clusters and males are infected more than females compared with the rest of the clusters, these findings match the results of the studies conducted in the provinces in this cluster[29,30]. The majority of the infection cases of this cluster (75%) are of Iranian nationality and urban and rural infection rates revealed no significant difference, the results are consistent with some studies[31] and inconsistent with some others[32]. The majority of the infection cases in this cluster (89.31%) are of the introduced type, being consistent with the results of studies previously performed in this cluster[33]. This cluster has the lowest average minimum and maximum temperature and generally colder with the lowest average pressure level compared with other clusters, thus, it can be stated that the majority of the provinces in this cluster have low climatic potential for the disease prevalence compared with other clusters.
Despite the potential climatic conditions for high incidence of malaria, the 4th cluster making up the Northern Iran strip provinces experienced declining incidence trend of the disease in decades as a result of malaria control program. Successful disease control, high socioeconomic conditions and higher income level compared to other endemic provinces are among the reason for the very low incidence of the disease in this cluster. The majority of the cases in this cluster are P. vivax, approximately half of the infected cases are of Iranian nationality and the other half of Afghan nationality. The ratio of infection rates in urban and rural residents is almost 4, the majority of which are of the introduced type. In terms of the climatic conditions, this cluster has the highest humidity with the highest pressure level, with far higher average annual precipitation, all consistent with those results of similar studies in the provinces of this cluster[34].
Cluster 5 includes only Ilam Province and during the study period, this province had the average incidence of zero and recognized as a malaria free province, that is why it is located in a separate cluster. This province is similar to the provinces of the 3rd cluster in terms of the climatic conditions.
In the research by Halimi et al., malaria prevalence in Iran was studied in relation with the climatic conditions and four ratings of the highest potential, high potential, moderate potential and low potential for activity and proliferation of Anopheles mosquitoes were determined. In the current study, besides the climatic conditions, the epidemiologic status of the provinces was taken into account, one reason why the fundamental differences were observed in the provinces in the two studies[35].
Malaria transmission is under the influence of diverse climatic, demographic, biological, physical and socioeconomic factors. In general, this study suggested that malaria is an important endemic disease in Iran and its elimination requires continued national determination and dedication accompanied by strong political will considering the neighborhood with two endemic countries (Afghanistan and Pakistan) and emigration from these countries.
The present study has provided a new clustering for malaria in terms of the epidemiological and climatic variables. Using these results, health authorities and policymakers can intervene in highrisk areas with prioritizing the resources in order to obtain the final goal of malaria elimination. In addition, as the highest infection rate belongs to P. vivax and acquiring malaria elimination certificate depends on eliminating the local transmission of P. vivax, it is important to focus more on the control of P. vivax transmission pattern as much as possible.
Conflict of interest statement
The authors declare that they have no competing interests.
Acknowledgments
This article is part of the results of the first author’s dissertation for fulfillment of a master degree in Biostatistics from Department of Biostatistics and Epidemiology, School of Public Health, Mazandaran University of Medical Sciences, Sari, Iran. The authors are very grateful to Iran Meteorological Organization and Center of Diseases Control, Ministry of Health and Medical Education for their providing access to their data. This study was financially supported by the deputy for Research, Mazandaran University of Medical Sciences.
Authors’contributions
VM, AAE and JYC Conceived the study design, prepared the data set for analysis, performed the analysis, Produced map, interpreted the result ,drafted, revised and written the manuscript. AR and FN collated the data and revised the manuscript. All authors discussed the results and implication and commented on the manuscript at all stages and approved the final manuscript.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Epitope finding in 2019 novel coronavirus (2019-nCoV): The first world report
- COVID-19 international outbreak and the need for a suitable estimation model: A second-order polynomial equation with constant coefficients based on imported infected cases seems inadequate
- Antimalarial activity of the aqueous extract of Euphorbia cordifolia Elliot in Plasmodium berghei-infected mice
- Epidemiological, molecular characterization and risk factors of human brucellosis in Iran
- Expert consensus guidelines on clinical use of Xiyanping injection for acute infectious diseases
- Crimean-Congo hemorrhagic fever: etiology, diagnosis, management and potential alternative therapy