Twenty-year survival after iterative surgery for metastatic renal cell carcinoma:A case report and review of literature
2020-04-09EmilioDeRaffeleMariateresaMirarchiRiccardoCasadeiClaudioRicciEugenioBrunocillaFrancescoMinni
Emilio De Raffele,Mariateresa Mirarchi,Riccardo Casadei,Claudio Ricci,Eugenio Brunocilla,Francesco Minni
Emilio De Raffele,Dipartimento dell'Apparato Digerente,Policlinico S.Orsola-Malpighi,University of Bologna,Bologna 40138,Italy
Mariateresa Mirarchi,Dipartimento Strutturale Chirurgico,Ospedale SS Antonio e Margherita,Tortona(AL)15057,Italy
Riccardo Casadei,Claudio Ricci,Francesco Minni,Dipartimento di Scienze Mediche e Chirurgiche(DIMEC),Alma Mater Studiorum,Policlinico S.Orsola-Malpighi,University of Bologna,Bologna 40138,Italy
Eugenio Brunocilla,Dipartimento di Medicina Specialistica,Diagnostica e Sperimentale(DIMES),Alma Mater Studiorum,Policlinico S.Orsola-Malpighi,University of Bologna,Bologna 40138,Italy
Abstract BACKGROUND The therapeutic approach of metastatic renal cell carcinoma(RCC)represents a real challenge for clinicians,because of the variable clinical course;the recent availability of numerous targeted therapies that have significantly improved overall oncological results,but still with a low percentage of complete responses;and the increasing role of metastasectomy(MSX)as an effective strategy to achieve a durable cure,or at least defer initiation of systemic therapies,in selected patients and in the context of multimodality treatment strategies.CASE SUMMARY We report here the case of a 40-year-old man who was referred to our unit in November 2004 with lung and mediastinal lymph nodes metastases identified during periodic surveillance 6 years after a radical nephrectomy for RCC;he underwent MSX of multiple lung nodules and mediastinal lymphadenectomy,with subsequent systemic therapy with Fluorouracil,Interferon-alpha and Interleukin 2.The subsequent clinical course was characterized by multiple sequential abdominal and thoracic recurrences,successfully treated with multiple systemic treatments,repeated local treatments,including two pancreatic resections,conservative resection and ablation of multiple bilobar liver metastases,resection and stereotactic body radiotherapy of multiple lung metastases.He is alive without evidence of recurrence 20 years after initial nephrectomy and sequential treatment of recurrences in multiple sites,including resection of more than 38 metastases,and 5 years after his last MSX.CONCLUSION This case highlights that effective multimodality therapeutic strategies,including multiple systemic treatments and iterative aggressive surgical resection,can be safely performed with long-term survival in selected patients with multiple metachronous sequential metastases from RCC.
Key Words:Renal cell carcinoma;Metastases;Surgery;Thermal ablation;Radiation;Case report;Systemic therapy
INTRODUCTION
Renal cell carcinoma(RCC)accounts for 3% to 5% of all adult malignancies[1],with an increasing incidence in the last decades,but with a concomitant progressive improvement of survival rates[2-4].Metastatic RCC(mRCC)has been for long characterized by a dismal prognosis,which has however dramatically improved in the last decades because of the recent development of multiple novel therapeutic agents[5,6].Approximately 20%-40% of patients have synchronous metastases at the time of diagnosis,while 20%-40% develop recurrent disease after potentially curative resection of localized RCC[4,6,7].
In patients with recurrence after nephrectomy,systemic immunotherapies,mainly with interferon(IFN)and interleukin-2(IL-2),have been for long the only available treatment approaches,with modest improvement of oncological results,frequent severe toxicity,and with persistent complete responses(CR)in less than 5%-10%[3,4,6,8].A better understanding of the pathogenesis of the RCC over the past decades has however determined a substantial evolution in the systemic treatment of mRCC,based on the use of therapeutic agents that affect specific targets of molecular pathways of RCC;these include multikinase inhibitors(sorafenib,sunitinib,pazopanib,axitinib,cabozantinib and lenvatinib);mammalian target of rapamycin(mTOR)inhibitors(everolimus and temsirolimus);bevacizumab,a monoclonal antibody against the vascular endothelial growth factor;and immunomodulatory agents,including inhibitors of immune checkpoint pathways(nivolumab,ipilimumab,atezolizumab,avelumab,pembrolizumab)[3,4,8].Most of these agents,alone or in combination,have been shown to prolong survival and improve overall oncological results,although CR is achieved in less than 10% of patients with mRCC[8].
As a consequence,metastasectomy(MSX)is increasingly considered,even though only a minority of patients seem to be eligible to local treatments,including surgical resection[9,10].There is growing evidence that potentially curative resection of the primary tumour and metastatic sites,when technically feasible,may represent the optimal strategy to achieve durable cure or at least to defer initiation of systemic therapies,in the context of multimodality treatment of mRCC[5,6,9,11-15].Moreover,it is well known that aggressive surgical approach with repeated MSX may increase survival in selected patients developing recurrent metastases from RCC[16-19].
We report here a patient with multiple thoracic and abdominal recurrences starting from 6 years after radical nephrectomy for clear-cell RCC(ccRCC),who was successfully treated with multiple systemic treatments,repeated surgical resection of lung,liver and pancreas metastases,and multiple local treatments of lung and liver metastases.He is alive without evidence of recurrence 20 years after initial nephrectomy and 5 years after his last MSX.To our knowledge,this is the first report of such a case.We also review the current literature on the role of MSX and of iterative surgery in the management of mRCC.
CASE PRESENTATION
Chief complaints
A 40-year-old Caucasian man was referred to our unit in November 2004 with a nodule measuring 15 mm in the inferior lobe of the right lung and multiple enlarged right mediastinal lymph nodes measuring up to 45 mm,identified by performing a periodic surveillance contrast-enhanced computerized tomography(CECT)scan 6 years after a radical left nephrectomy for ccRCC(Table 1).
History of present illness
In December 1998,because of the appearance of sudden macroscopic hematuria with pain,the patient was diagnosed with renal neoplasm without distant metastases.An open left radical nephrectomy was performed and the patient was discharged 6 d later,after an uneventful postoperative course.Pathological examination revealed an infiltrating ccRCC measuring 95 mm × 55 mm × 50 mm,Fuhrman grade 3,without the involvement of the lymph nodes and the perirenal adipose tissue,with negative surgical margins.Adjuvant systemic therapy was not indicated and the patient was followed up regularly.The complete medical history of the patient is summarized in Figure 1 and Table 1.
History of past illness
The patient had a free previous medical history.
Physical examination
The patient was in excellent physical conditions and asymptomatic.
Laboratory examinations
The laboratory data on admission,including renal function tests,were normal.The International Metastatic RCC Database Consortium(IMDC)Risk Score was 0.
Imaging examinations
The CECT scan suggested the occurrence of a lung metastasis(LuM)with metastatic right mediastinal lymph nodes.A positron emission tomography with 18F-labeled fluoro-2-deoxyglucose associated with computed tomography(18F-FDG-PET/CT)documented slight FDG uptake within the mediastinal lymph nodes,without evidence of further distant metastases.A computed tomography guided biopsy of an enlarged mediastinal lymph node confirmed the recurrence of the ccRCC.
Treatment and outcome of lung recurrence
In December 2004 the patient underwent right thoracotomy;intraoperative palpation of the right lung parenchyma revealed multiple nodules,which were removed with multiple wedge resections,along with radical ipsilateral mediastinal lymphadenectomy.The postoperative course was uneventful and the patient was discharged 10 d after surgery.Pathological examination showed one parenchymal nodule measuring 15 mm and 8 additional nodules,measuring 1-3 mm,of metastatic G3 ccRCC;mediastinal lymph nodes metastases(LyM)were also present.Postoperative adjuvant systemic therapy from January to April 2005,consisted of fluorouracil,interferonalpha(IFN-α),and IL-2(Table 1).From May 2005 to March 2006 the patient received maintenance systemic therapy with IL-2,3 MU subcutaneously thrice a week.
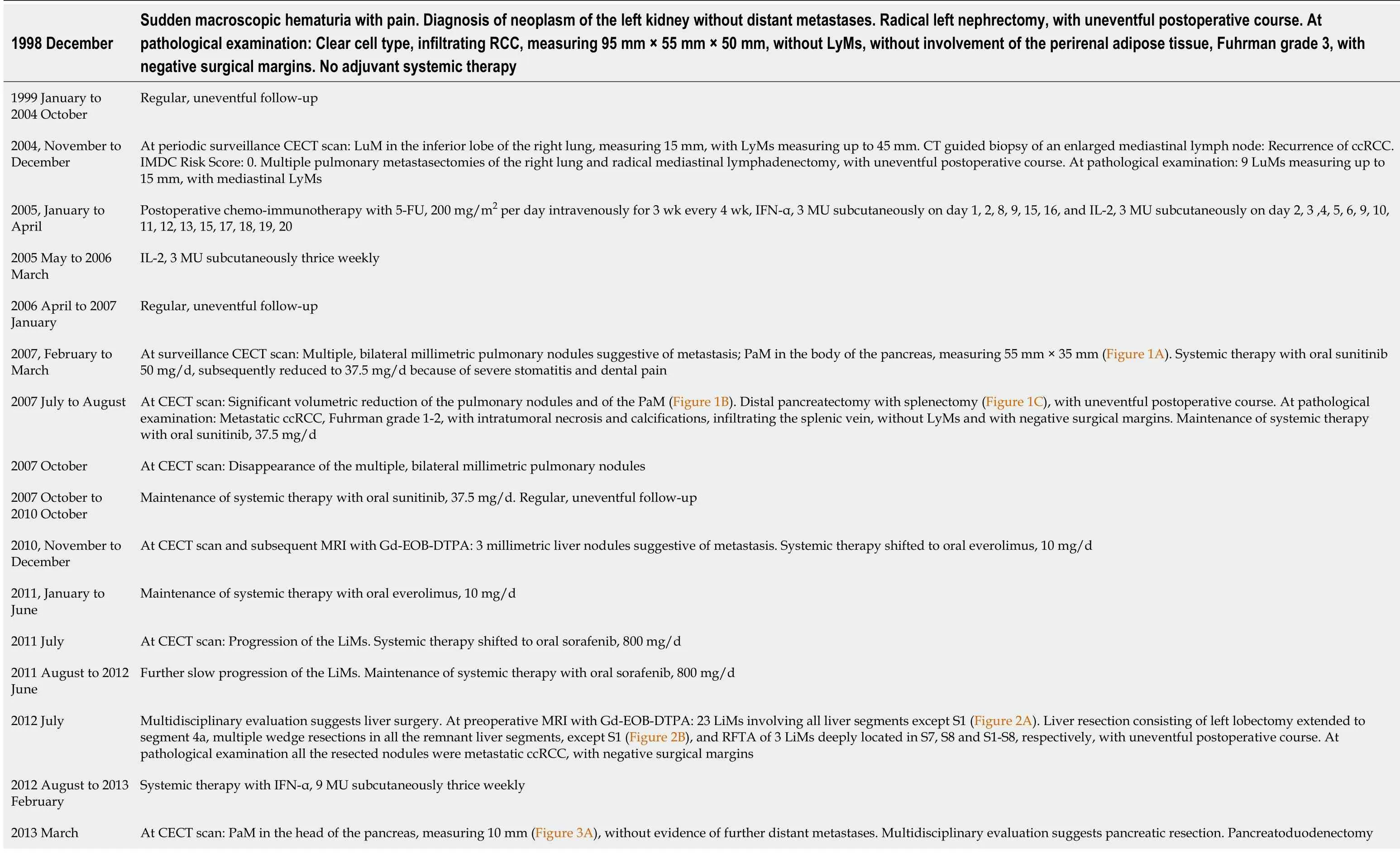
Table 1 Timeline of interven tions and outcomes
RCC:Renalcell carcinoma;LyMs:Lymph nodesmetastases;CECT:Contrast-enhanced computerized tomography;LuMs:Lungmetastasis;CT:Computedtomography;ccRCC:Clear-cel l renal cel lcarcinoma;IMDC:International Metastat icRCC Database Consortium;5-FU:Fluorouracil ;IFN-α:Interferon-alpha;IL-2:Interleukin-2;PaM:Pancreatic metastasis;MRI:Mag neticre sonan ce imaging;Gd-EOB-DTP A:Gadolinium ethoxyb enzy ldimeg lumine;LiMs:Liv er metastase s;RFTA:Radiofrequency therma lablation;SBRT:Stereo tactic body radiotherapy.
Treatment and outcome of lung and pancreas recurrence
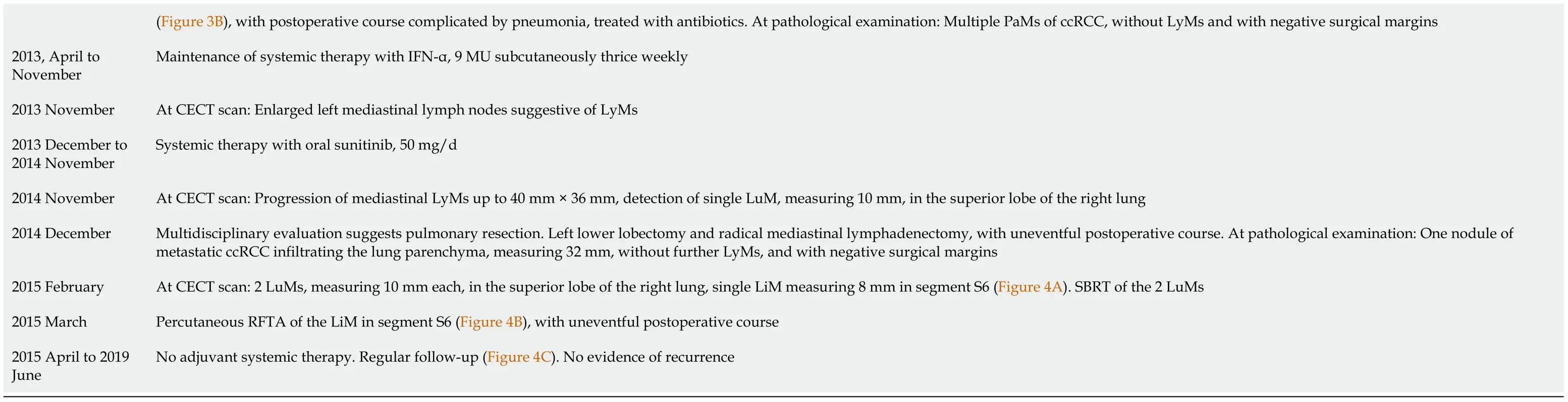
The subsequent follow-up was uneventful until February 2007,when the periodic surveillance CECT evidenced multiple,bilateral millimetric pulmonary nodules suggestive of metastasis,and a metastatic nodule measuring 55 mm × 35 mm in the body of the pancreas,with upstream main pancreatic duct dilatation and parenchymal atrophy(Figure 2A).Systemic therapy with oral sunitinib 50 mg/d was started(Table 1).The CECT performed 5 mo later demonstrated a significant volumetric reduction of the multiple pulmonary nodules and of the pancreatic metastasis(PaM),which shrunk to 41 mm × 27 mm(Figure 2B).After a multidisciplinary evaluation,in July 2007 the patient underwent distal pancreatectomy with splenectomy(Figure 2C),with the guide of intraoperative ultrasonography(IOUS),as previously described[20].The postoperative course was uneventful and the patient was discharged 11 d after surgery.Pathological examination revealed a metastatic ccRCC,Fuhrman grade 1-2,with intratumoural necrosis and calcifications,infiltrating the splenic vein,without nodal involvement(40 lymph nodes examined),and with negative surgical margins.Systemic therapy with oral sunitinib was maintained(Table 1).At the CECT scan 3 mo later the multiple,bilateral millimetric pulmonary nodules had disappeared.
Treatment and outcome of liver recurrence
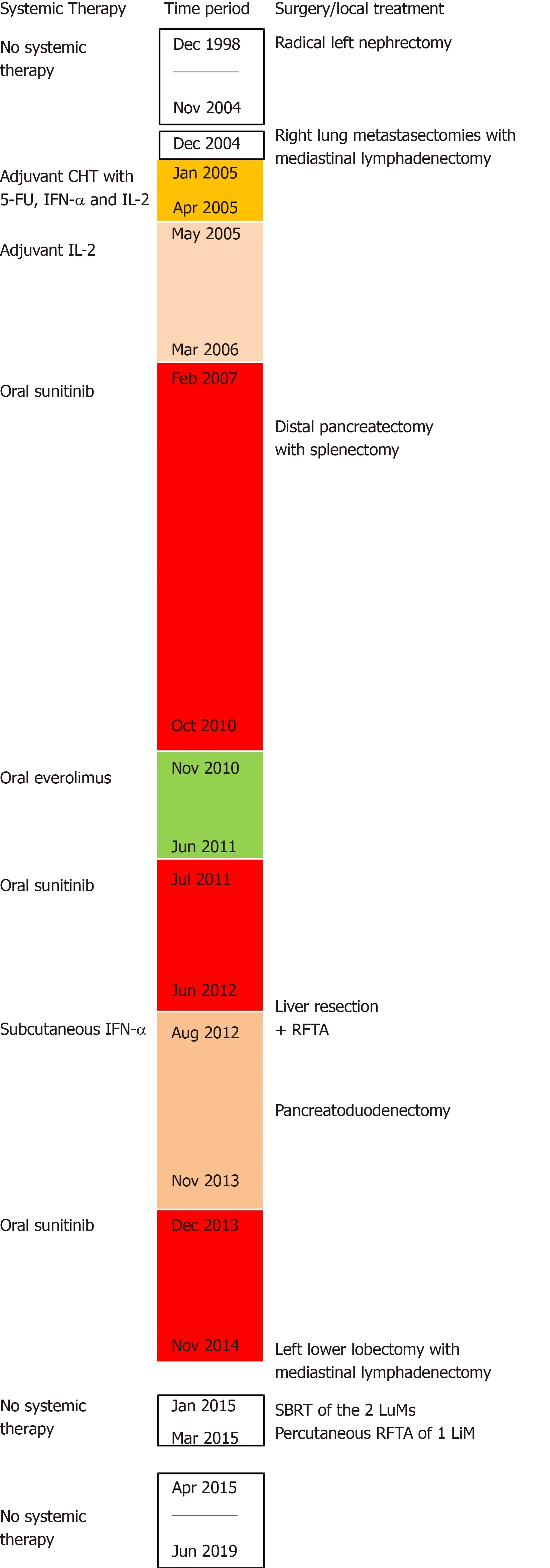
Figure 1 Timeline of systemic therapies,surgical procedures and local treatments.CHT:Chemotherapy;5-FU:Fluorouracil;IFN-α:Interferon-alpha;IL-2:Interleukin 2;RFTA:Radiofrequency thermal ablation;SBRT:Stereotactic body radiotherapy;LuM:Lung metastasis;LiM:Liver metastases.
The subsequent follow-up was uneventful until November 2010,when the periodic surveillance CECT and the subsequent magnetic resonance imaging(MRI)with gadolinium ethoxybenzyl dimeglumine(Gd-EOB-DTPA),demonstrated 3 millimetric liver nodules,suggestive of liver metastases(LiM).Systemic therapy was then shifted to oral everolimus 10 mg/d.Eight months later,MRI with Gd-EOB-DTPA documented a progression of the metastatic liver disease.Systemic therapy was then shifted to oral sorafenib 800 mg/d.Further follow-up was characterized by a slow progression of the metastatic liver disease.In June 2012,MRI with Gd-EOB-DTPA demonstrated 23 nodules involving all liver segments except S1(Figure 3A).Considering the excellent clinical conditions of the patient,the slow progression of the liver disease and the resistance to multiple systemic treatments,a multidisciplinary evaluation suggested liver resection(LR).One month later the patient was operated(Table 1):IOUS showed 24 intrahepatic nodules;IOUS-guided conservative LR was performed with the usual technique[21],with intermittent hepatic pedicle clamping of 87 min(Figure 3B);three nodules deeply located in segments S7,S8 and S1-S8,respectively,underwent radiofrequency thermal ablation(RFTA).The postoperative course was substantially uneventful and the patient was discharged 13 d after surgery.Pathological examination revealed that all the resected nodules were metastatic ccRCC,with negative surgical margins.Systemic therapy with IFN-α,9 MU subcutaneously thrice weekly,was started.
Treatment and outcome of pancreas recurrence
Eight months later,a CECT scan documented a metastatic nodule measuring 10 mm in the head of the pancreas(Figure 4A),without evidence of liver recurrence or further distant metastases.After a multidisciplinary evaluation,in March 2013 the patient underwent pancreatoduodenectomy(Figure 4B).The postoperative course was complicated by pneumonia treated with antibiotics;the patient was discharged 14 d after surgery.Pathological examination revealed multiple intrapancreatic nodules of metastatic ccRCC,without nodal involvement,and with negative surgical margins.Systemic therapy with IFN-α,9 MU subcutaneously thrice weekly was maintained.
Treatment and outcome of lung and mediastinal lymph nodes recurrence
In November 2013,a CECT scan demonstrated enlarged left mediastinal lymph nodes suggestive of LyMs(Table 1).Thus,systemic therapy was then again shifted to oral sunitinib 50 mg/d;however,the subsequent follow-up demonstrated a slow progression of the mediastinal LyMs.A CECT scan in November 2014 confirmed the presence of mediastinal LyMs measuring up to 40 mm × 36 mm,and detected a nodule suggestive of a metastasis,measuring 10 mm,in the superior lobe of the right lung.Considering the excellent clinical conditions of the patient,a multidisciplinary evaluation addressed towards the surgical resection of the LyMs and the subsequent stereotactic body radiotherapy(SBRT)of the small LuM.In December 2014 the patient underwent left lower lobectomy and radical ipsilateral mediastinal lymphadenectomy.The postoperative course was uneventful and the patient was discharged 4 d after surgery.Pathological examination showed one 32 mm nodule of metastatic ccRCC infiltrating the lung parenchyma,without further nodal involvement(17 mediastinal lymph nodes examined),and with negative surgical margins.
Treatment and outcome of lung and liver recurrence
Two months later,a CECT scan detected two adjacent nodules,measuring 10 mm each,in the superior lobe of the right lung,and a liver nodule measuring 8 mm in segment S6(Figure 5A),without evidence of further distant metastases.SBRT of the adjacent LuMs was performed,followed by percutaneous RFTA of the LiM in segment S6(Figure 5B),with uneventful postoperative course.Adjuvant systemic therapy was not indicated and the patient was regularly followed up(Figure 5C).
FINAL DIAGNOSIS
The patient developed multiple metachronous metastases from ccRCC.Lung and mediastinal lymph nodes metastases were identified during periodic surveillance 6 years after a radical nephrectomy for an infiltrating ccRCC,Fuhrman grade 3.Pathological examination showed multiple LuMs of G3 ccRCC with LyMs.The subsequent clinical course was characterized by multiple sequential abdominal and thoracic recurrences of G1 to G3 ccRCC.
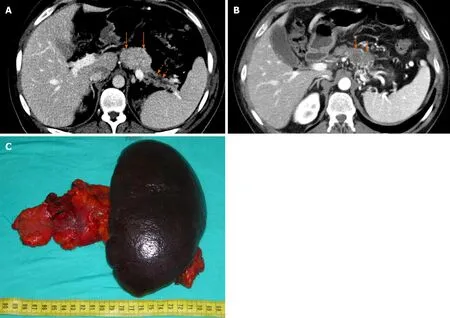
Figure 2 Treatment and outcome of pancreas recurrence.The contrast-enhanced computerized tomography(CECT)shows a pancreatic metastasis(PaM)measuring 55 mm × 35 mm(A)in the body of the pancreas(orange full arrows),with upstream main pancreatic duct dilatation(orange dotted arrows)and parenchymal atrophy.The CECT performed 5 mo later,after systemic therapy with oral sunitinib,demonstrates a significant volumetric reduction of the PaM(B),which shrunk to 41 mm × 27 mm(orange full arrows).The patient underwent distal pancreatectomy with splenectomy(C).
TREATMENT
The first lung recurrence was treated with multiple wedge resections and mediastinal lymphadenectomy.Subsequently,the patient was successfully treated with multiple systemic treatments and repeated local treatments,including two pancreatic resections,conservative resection and ablation of multiple bilobar liver metastases,resection and stereotactic body radiotherapy of multiple lung metastases.
OUTCOME AND FOLLOW-UP
At present,the patient is 54-year old,in excellent clinical conditions and without evidence of tumour recurrence more than 20 years after the beginning of his renal cancer,and 5 years after the last successful treatment of metastatic disease(Table 1).
DISCUSSION
RCC represents the 6th most common malignant tumour in men,and the 10th most common malignant tumour in women[1].Despite an increasing incidence in the last decades,overall survival(OS)rates have progressively improved,at least in Western countries,as a consequence of progressive declines in tumour size and stage due to earlier diagnosis[2-4],and refinements in surgical technique[3,6,22,23],reaching 5-year OS rates of 74% in the United States[4].Metastatic ccRCC has been for long characterized by a dismal prognosis,with a historic median survival of 12 mo,which has however dramatically improved in the last decades because of the recent availability of multiple novel agents;nevertheless,complete responses with systemic therapies remain occasional[6].Approximately 20%-40% of patients have synchronous metastases at the time of diagnosis,while 20%-40% of patients develop recurrent disease after potentially curative resection of localized RCC,within 5 years in most cases[4,6,7,11].A minority of patients experiences disease recurrence 5 years or more after nephrectomy,with usually less aggressive disease and long survival after recurrence[24];in 10% of patients,RCC recurs after more than 10 years after surgery[25].Metastases from RCC are often multifocal[6].The most common sites are lungs,bone,lymph nodes,adrenal glands,liver,brain,contralateral kidney and pancreas[4,6,7,26].
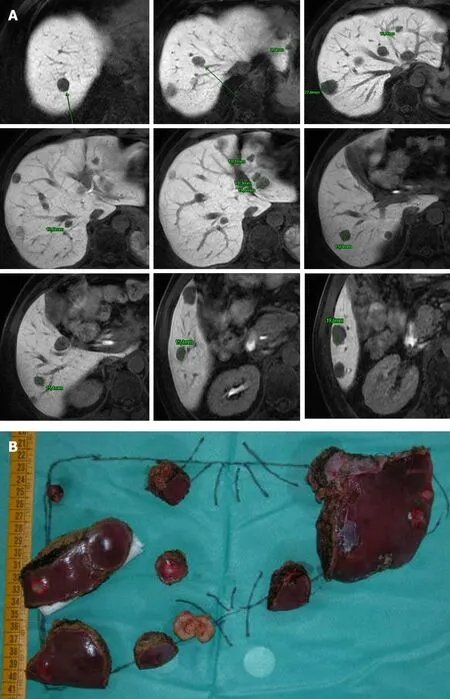
Figure 3 Treament and outcome of liver recurrence.The magnetic resonance imaging with gadolinium ethoxybenzyl dimeglumine demonstrates multiple liver metastases involving all liver segments except segment S1(A).The patient underwent intraoperative ultrasonography-guided conservative liver resection(LR)(B),with intermittent hepatic pedicle clamping of 87 min.LR consisted of left lobectomy extended to segment 4a,with gentle detachment of a metastatic nodule from the left portal vein and the middle hepatic vein,respectively;multiple wedge resections in all the remnant liver segments,except S1;and radiofrequency thermal ablation of 3 nodules deeply located in segments S7,S8 and S1-S8,respectively.
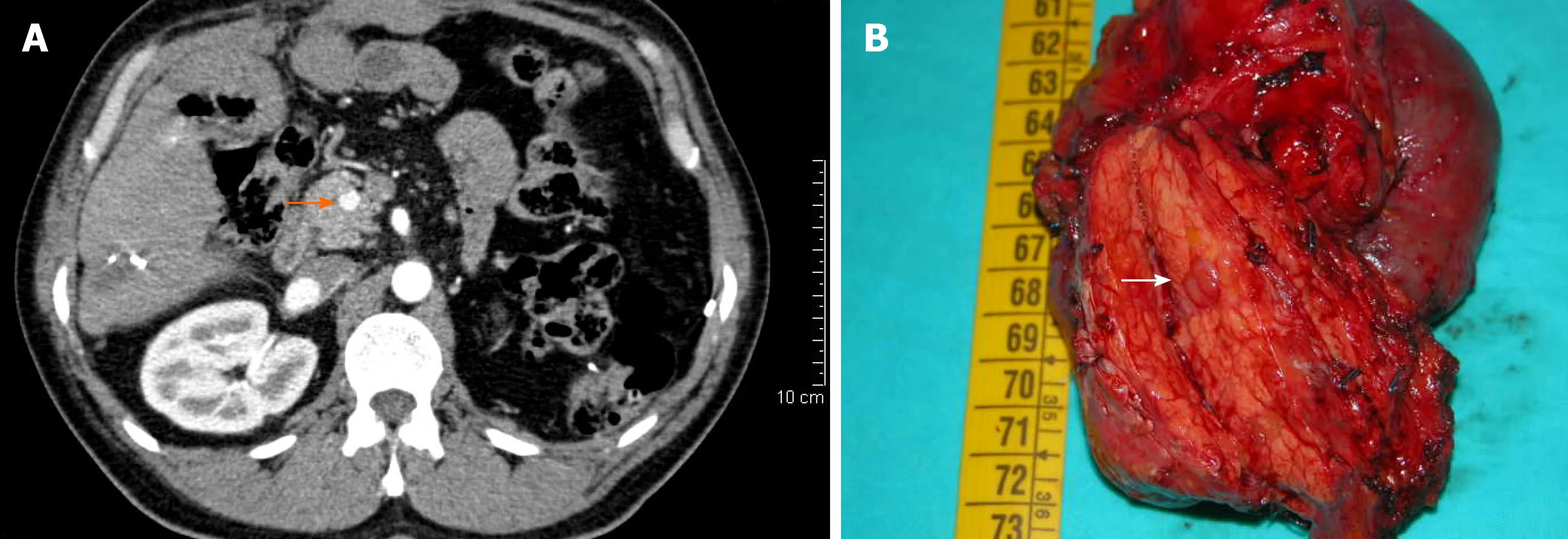
Figure 4 Treatment and outcome of further pancreas recurrence.The contrast-enhanced computerized tomography scan shows a pancreatic metastasis(PaM)measuring 10 mm in the head of the pancreas(orange full arrow)(A).The patient underwent pancreatoduodenectomy(B);the PaM is indicated in the specimen(white full arrow).Pathological examination revealed multiple intrapancreatic nodules of metastatic clear-cell renal cell carcinoma,without nodal involvement,and with negative surgical margins.
The likelihood of disease recurrence is however extremely variable among patients,being determined by numerous,and only partially known,host and tumour factors.Well-established prognostic factors for localized RCC include the size of the primary tumour;the extent of disease spread;the tumour histology;the presence of microvascular invasion and of collective system invasion;a high tumour grade and the presence of necrosis at histology;several clinical factors such as male sex,advanced age,poor performance status(PS),and symptomatic presentation[7,27].Similarly,multiple pathological and clinical variables have prognostic relevance in mRCC patients proposed for the available systemic therapies[27,28];these include the tumour histology;the number,size and site of metastases[28],with liver and bone metastases having the worst prognosis[29,30];the tumour shrinkage after treatment with targeted agents[28].Various integrated scoring systems that aim to optimize prognostication and treatment strategies are based on some of these prognostic factors,comprehending the Memorial Sloan Kettering Cancer Center(MSKCC)and the IMDC prognostic scores[4,7,27,28].
RCC is an immunogenic tumour characterized by a remarkable infiltration of immune cells.Systemic immunotherapies,mainly with IFN and IL-2,have long been the only available treatment for mRCC,with modest improvement of oncological results,frequent severe toxicity,and persistent CR in less than 5-10% of patients receiving high-dose IL-2[3,4,6,7].However,a better understanding of the pathogenesis of the ccRCC has determined a substantial evolution in the systemic treatment of mRCC,based on the use of therapeutic agents that affect specific targets of molecular pathways of RCC[3,4,8],and led to improved overall oncology outcomes,but with CR in less than 10% of patients[8].As a consequence,potentially curative MSX is increasingly considered,whenever possible,in the context of multimodal treatments of mRCC,even though only a minority of patients,about 25% of those with metachronous metastases and probably less than 10% of those with synchronous metastases,seem to be eligible to local treatments,including surgical resection[9,10].
Recent guidelines for patients with mRCC recommend MSX of potentially resectable metastases[2,12,13,31],although criteria for selection are heterogeneous[12].MSX is usually suggested in patients with good PS,solitary or oligometastases,and primary tumours with favourable risk,after multidisciplinary evaluation[2,31].Nevertheless,there is growing evidence that potentially curative resection of the primary tumour and metastatic sites,when technically feasible,may represent a promising strategy to achieve durable cure or at least to defer initiation of systemic therapies,in wellselected patients with good performance status and favourable risk.Actually,the overall utilization of MSX,in the context of multimodality treatment of mRCC,has progressively increased in recent years[2,5,6,9,11,12-15].In a recent population-based analysis,surgical resection of RCC metastases has been associated with rates of overall complication,major complication(Clavien III-IV)and in-hospital mortality of 45.7%,25.1% and 2.4%,respectively[32].A perioperative mortality of 0.9% to 2.3% has been reported in other series[6].Nevertheless,multiple studies demonstrate a long-term survival advantage after complete metastasectomy(CMSX)of ccRCC metastases to parenchymal organs,vseither incomplete or no MSX,and also patients with metastases to multiple sites may benefit from CMSX[5].In a wide series of 887 patients who developed multiple metastases after nephrectomy for RCC between 1976 and 2006[19],125(14%)underwent complete surgical resection of all metastases;CMSX was associated with a significant prolongation of median CSS,also in case of synchronous and/or multiple metastases.The systematic review of Dabestaniet al[9]has noticeably confirmed that OS and CSS rates of RCC metastatic to multiple sites are significantly longer after CMSX,compared with incomplete or no MSX.In a more recent systematic review of 2267 patients,958 who received CMSX and 1309 without CMSX[5],CMSX significantly reduced the overall mortality;the median OS ranged between 36.5 and 142 mo after CMSXvs8.4 and 27 mo without CMSX;6 of the 8 studies evaluated in the systematic review included 36% to 56% of patients with metastases to multiple organ sites.Another systematic review based on 56 studies[14],reported that the median OS ranged from 36 to 142 mo for patients undergoing MSX,compared to 8-27 mo for those without MSX;the most relevant prognostic factor for OS was CMSX;lung MSX seemed to show the best survival benefit.The favourable impact of MSX has been confirmed also in patients treated in the targeted therapy era[10].In a recent nationwide series from United States including 6994 patients with mRCC who underwent cytoreductive nephrectomy from 2006 to 2013[15],a total of 1976 patients(28.3%)underwent surgical resection of metastatic lesions;the median OS was 24.1 mo for MSX patientsvs18.9 mo for patients without MSX(P<0.001),and the 1-,2-,and 5-year OS rates for MSXvsno MSX patients were 68.4%,50.0%,and 24.4%vs64.1%,43.0%,and 19.5%,respectively(P<0.001);the survival advantage of MSX was confirmed also among patients treated with targeted therapies,where the 1-,2-,and 5-year OS rates for MSXvsno MSX patients were 67.8%,45.3% and 19.4%vs65.9%,39.4%,and 15.2%,respectively(P= 0.008).In addition,also incomplete MSX followed by targeted therapy has been recently suggested to give some advantage in OS and progression-free survival,compared to targeted therapy alone[10,11].The simultaneous occurrence of metastases in the liver and lungs seems to be the worst combination in terms of long-term prognosis[33].
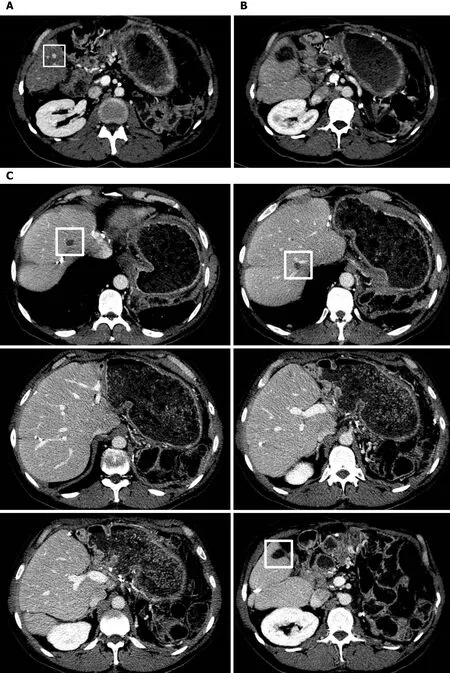
Figure 5 Treatment and outcome of further liver recurrence.The contrast-enhanced computerized tomography(CECT)scan demonstrates a liver metastases(LiM)measuring 8 mm in segment S6(white square)(A).The patient underwent successful percutaneous radiofrequency thermal ablation(RFTA),as shown in the postoperative CECT(B).The CECT scan 18 mo later demonstrates the absence of further LiMs,with the areas of intraoperative RFTA in segments S8 and S7,respectively,and the area of percutaneous RFTA in segment S6,delineated by white squares(C).
Patients with mRCC are usually managed by combining local treatments and systemic therapy.The sequencing of MSX and systemic treatments is however still debated.In selected patients,especially in case of limited metastatic disease,MSX may reduce systemic therapy and the associated toxicities,either delaying its initiation or withdrawing treatment for a while[6].Neoadjuvant targeted therapy before MSX has been suggested by some authors[34,35].The overall impact of adjuvant systemic therapy with targeted or immunomodulatory agents after CMSX is still uncertain,and multiple studies are underway[6,36].In a small multicenter RCT of 69 patients with metastatic ccRCC pretreated with nephrectomy,postoperative sorafenib after radical MSX of ≤ 3 lesions had no impact on the oncological outcome[37].
Different techniques of tumour focal ablation,including RFTA,microwave ablation,and cryoablation,either percutaneous image-guided or intraoperative,are wellestablished minimally invasive treatment modalities in selected RCC patients,with specific indications according to the features of the single tumours[38].At present,despite higher local recurrence rates,local ablation of primary RCC is considered a reasonable alternative to surgery in appropriately selected patients,because is easy to use,with fewer complication rates,shorter hospital stay,faster convalescence and lower overall costs[6,39].Moreover,RFTA is diffusely accepted as an effective minimally invasive modality in the treatment of metastases located to the liver and the lungs[40,41].Also SBRT may be useful in the management of both primary and metastatic RCC[6],including LuMs[42].
Lungs represent the most common site of metastasis from ccRCC[26],with an incidence of 30% to 50% in patients with mRCC[43].Largest case series of lung metastasectomy(LuMSX)reported 5-year survival rates of 37% to 54% for potentially curative resection of solitary or oligometastatic LuMs in selected patients[9].These findings have been confirmed in recent systematic reviews[14,15,44].Systematic lymph node dissection along with LuMSX has been suggested to achieve potentially curative surgery and better loco-regional control of the thoracic disease[44,45].In the case presented here,LuMs recurred obstinately,and were treated twice with LuMSX and systematic lymph node dissection,and once with SBRT,while their responsiveness to systemic therapies was variable.
LiMs are present in about 20% of patients with mRCC[26,30],are multiple in 75% and associated with extrahepatic disease in 85-90% of patients,respectively[46].LiMs have been traditionally associated with poor oncological outcomes,also in patients receiving targeted systemic therapies[30,46].Nevertheless,there is an increasing consensus toward performing LiMSX[47-49],since the overall oncological outcomes of LiMSX in selected patients seem to be not inferior to those reported after LR for colorectal LiMs[46,49].The number of liver nodules does not affect the oncological outcomes in most studies[47-49].RFTA of LiMs may represent an alternative to LiMSX in selected patients[40,47].In our patient,complete LiMSX was achieved with multiple limited IOUS-guided resections,with the minimum sufficient oncological margin,and 3 RFTA,to preserve as much nontumourous liver parenchyma as possible along with major intrahepatic vessels.This strategy is termed "conservative" or "parenchymalsparing",and has the advantage of limiting the risk of posthepatectomy liver failure even in patients with extensive liver disease,but also of increasing the chance of liver re-resection in case of recurrence[50].A single recurrent LiM occurred 31 mo later and underwent percutaneous RFTA.
The pancreas is an uncommon site for metastasis from RCC[51],with an incidence between 2% and 5%[25].Typically,PaMs are isolated,occur many years after primary tumour resection,and have been associated with rather favourable oncological outcome[25,51-53].PaMs are multifocal in 20% to 45% of the cases[25];multifocality detection may occur only on pathological examination of resected specimens[54].Oncological outcomes support PaMSX,thus most authors suggest that surgical resection still represents the only potentially curative option for isolated PaMs,because of 4- and 5-year survival rates between 66% and 88%[52,53].In the case of radical resection,multifocal PaMs have OS rates similar to solitary metastases[25].In the case presented here,a single PaM occurred 98 mo after nephrectomy,with synchronous multiple bilateral LuMs and was treated with distal pancreatectomy with splenectomy;pancreatic multifocal recurrence occurred 68 mo after the first occurrence of PaM and 166 mo after nephrectomy,without further distant metastases,and was successfully treated with pancreatoduodenectomy and postoperative systemic immunotherapy.
Aggressive surgical approach with sequential MSX may further increase survival in selected patients developing recurrent metastases from RCC[16-19],even without systemic therapy[55].Moreover,in patients with recurrence after CMSX the 5-year OS rates after resection of second and third metastases are similar to those observed after the initial MSX[17-18].In this regard,the case presented is quite unique,since the patient was treated successfully with sequential MSXs,including an extensive LR and pancreatoduodenectomy within just 9 mo,and other local treatments for multiple recurrences,along with different sequential lines of systemic therapy.He is alive and in excellent conditions more than 20 years after the resection of the primary tumour,despite the presence of several adverse prognostic factors.
CONCLUSION
The treatment of advanced ccRCC has undergone impressive ameliorations over the last decades.Based on the available literature and our experience,MSX and the other local treatments seem to play a favourable role in delaying cancer recurrence and the indication to systemic therapies.Tumour biology and dynamics seem to represent the most important factors in predicting the outcome of these tumours.Metachronous metastases may occur late,so these patients should undergo perpetual regular followup with cross-sectional imaging.The patient reported here indicates that remarkable,even unexpected,oncological results can be selectively obtained with multimodality treatment,including different systemic therapies,repeated surgical resection and local treatments,of sequential recurrent metastases to multiple organ sites,also in presence of multiple adverse prognostic factors.
杂志排行
World Journal of Clinical Cases的其它文章
- Role of monoclonal antibody drugs in the treatment of COVID-19
- Review of simulation model for education of point-of-care ultrasound using easy-to-make tools
- Liver injury in COVID-19:A minireview
- Transanal minimally invasive surgery vs endoscopic mucosal resection for rectal benign tumors and rectal carcinoids:A retrospective analysis
- Impact of mTOR gene polymorphisms and gene-tea interaction on susceptibility to tuberculosis
- Establishment and validation of a nomogram to predict the risk of ovarian metastasis in gastric cancer:Based on a large cohort
