Predictive factors for early clinical response in community-onset Escherichia coli urinary tract infection and effects of initial antibiotic treatment on early clinical response
2020-04-09YoungJunKimJeongMiLeeJaeHoonLee
Young Jun Kim,Jeong-Mi Lee,Jae-Hoon Lee
Young Jun Kim,Department of Internal Medicine,Wonkwang University College of Medicine,Iksan 54538,South Korea
Jeong-Mi Lee,Department of Public Health,Wonkwang University College of Medicine,Iksan 54538,South Korea
Jae-Hoon Lee,Department of Internal Medicine and Institute of Wonkwang Medical Science,Wonkwang University College of Medicine,Iksan 54538,South Korea
Abstract BACKGROUND Urinary tract infection(UTI)is a common disease.It often requires hospitalization,and severe presentations,including sepsis and other complications,have a mortality rate of 6.7%-8.7%.AIM To evaluate the predictive factors for early clinical response and effects of initial antibiotic therapy on early clinical response in community-onset Escherichia coli(E.coli)urinary tract infections(UTIs).METHODS This retrospective study was conducted at Wonkwang University Hospital in South Korea between January 2011 and December 2017.Hospitalized patients(aged ≥ 18 years)who were diagnosed with community-onset E.coli UTI were enrolled in this study.RESULTS A total of 511 hospitalized patients were included.66.1% of the patients had an early clinical response.The mean length of hospital stay in patients with an early clinical response were each 4.3 d shorter than in patients without an early clinical response.In the multiple regression analysis,initial appropriate antibiotic therapy(OR = 2.449,P = 0.006),extended-spectrum β-lactamase(ESBL)-producing E.coli(OR = 2.112,P = 0.044),improper use of broad-spectrum antimicrobials(OR =0.411,P = 0.006),and a stay in a healthcare facility before admission(OR = 0.562,P= 0.033)were the factors associated with an early clinical response.Initial broadspectrum antibiotic therapy was not associated with an early clinical response.CONCLUSION ESBL producing E.coli,and the type of residence before hospital admission were the factors associated with an early clinical response.Appropriateness of initial antibiotic therapy was a predictive factor for an early clinical response,but broadspectrum of initial antibiotic therapy did not impact early clinical response.
Key Words:Escherichia coli;Urinary tract infections;Adult;Community acquired infections
INTRODUCTION
Urinary tract infection(UTI)is a common disease.It often requires hospitalization,and severe presentations,including sepsis and other complications,have a mortality rate of 6.7%-8.7%[1-3].It was reported that poor clinical response after 72 h of antibiotic therapy was related to clinical failure[4].It is necessary to evaluate the clinical response after 72 h of antibiotic therapy in patients with UTIs.There has been an increase in the incidence of community-onset UTIs due to extended-spectrum β-lactamase(ESBL)producingEscherichia coli(E.coli)[5,6].These findings have increased the use of initial broad-spectrum antimicrobials in patients with UTIs.However,use of broad-spectrum antimicrobials result in nosocomial acquisition of antimicrobial-resistant bacteria or occurrence ofClostridium difficile infections[7].
In this study,we investigated the predictive factors for early clinical response in community onsetE.coliUTIs and the impact of severe presentations and initial antibiotic therapy on this early clinical response.
MATERIALS AND METHODS
This retrospective study was conducted at Wonkwang University Hospital in South Korea between January 2011 and December 2017.Hospitalized patients(aged ≥ 18 years)who were diagnosed with community-onsetE.coliUTI were enrolled in this study.Patients who were transferred to another hospital during treatment and those who had other concurrent infectious diseases were excluded.Community-onset UTI was defined as an infection that was diagnosed within 48 h of hospital admission.UTIs with anatomical urinary tract modifications,including any urinary diversion procedure,obstruction,pregnancy,or renal transplant,were defined as complicated UTIs[2].Septic shock was defined as sepsis with hypotension(systolic blood pressure less than 90 mmHg or 40 mmHg less than the patient’s baseline blood pressure)for at least 1 h despite adequate fluid resuscitation[8].A concurrent bacteremia was defined as the isolation ofE.coliwith identical antibiotic susceptibility patterns from both urine and blood cultures simultaneously.
Acute renal failure was defined as an increase in the serum creatinine levels by more than 300% than the baseline values or serum creatinine ≥ 4.0 mg/L with an acute increase of at least 0.5 mg/dL[9].An early clinical response was defined as meeting the following criteria 72 h after initial antibiotic therapy:defervescence,recovery from hypotension,decrease in white blood cell count compared to baseline values,and improvement of urinary tract symptoms or signs.Initial antibiotic therapy was defined as antimicrobials received within 24 h after admission.Initial antibiotic therapy was considered appropriate ifE.coliwas susceptible to initial antimicrobials based onin vitroantimicrobial susceptibility testing using Clinical Laboratory and Standards Institute guidelines.Improper broad-spectrum antibiotic therapy was defined as use of carbapenem,fourth-generation cephalosporin,piperacillin/tazobactam or cefoperazone/sulbactam to third-generation cephalosporin-susceptibleE.coli.
We compared participants’ medical and laboratory data usingχ2or Fisher’s exact tests for categorical variables,and independentt-tests or Mann–Whitney tests for continuous variables.A backward stepwise multiple logistic regression analysis was performed to evaluate the effect of independent variables on early clinical response.APvalue of <0.05(two-sided)was considered statistically significant.SPSS version 22.0 for Windows(SPSS Inc.,Chicago,IL,United States)was used for the statistical analyses.This study was approved by the institutional review board(WKUH 2020-03-023).
RESULTS
A total of 511 patients were included in this study.The mean age of the patients was 63 ± 17.8 years.Among them,89.1% of the patients were women,23.7% resided in a healthcare-associated facility before admission,and 66.1% had an early clinical response.The mean length of hospital stay for patients with an early clinical response was 6.8 days,4.3 d shorter than for patients without an early clinical response.The mean time to defervescence in patients with an early clinical response was 36.9 h,64 h earlier than in patients without an early clinical response.About a quarter[23.1%(118/511)]of patients initially presented with septic shock.Initial septic shock more frequently occurred in patients without an early clinical response than in patients with an early clinical response[28.3%(49/173)vs20.4%(69/338),P =0.045].Concurrent bacteremia was observed in 45%(230/511)of patients.The patients without an early clinical response more frequently had concurrent bacteremia than the patients with early clinical response[51.4%(89/173)vs41.7%(141/338),P =0.039].Acute renal failure were more frequent in patients without an early clinical response;however it was not statistically significant[13.4%(23/173)vs8.6%(29/338),P =0.121].Renal and perirenal abscesses occurred in 6.7%(34/511)of patients but had no significant effect on early clinical response.Patients with an early clinical response more frequently received initial appropriate antibiotic therapy than patients without an early clinical response[90.8%(307/338)vs81.5%(141/173),P =0.002].Initial broad-spectrum antibiotic therapy was more frequently used in patients without an early clinical response than in patients with an early clinical response[32.9%(57/173)vs16.3%(55/338),P<0.001].The rate of improper use of broad-spectrum antimicrobials was higher in patients without an early clinical response than in patients with one[32.9%(57/173)vs13.6%(46/338),P<0.001](Table 1).In the multiple regression analysis,initial appropriate antibiotic therapy(OR = 2.449,95%CI:1.294-4.637,P =0.006)),ESBL-producingE.coli(OR = 2.112,95%CI:1.020-4.374,P =0.044),a stay in a healthcare facility before admission(OR = 0.562,95%CI:0.331-0.954,P =0.033)and improper broad-spectrum antibiotic therapy(OR = 0.411,95%CI:0.220-0.765,P =0.006)were factors associated with an early clinical response(Table 2).
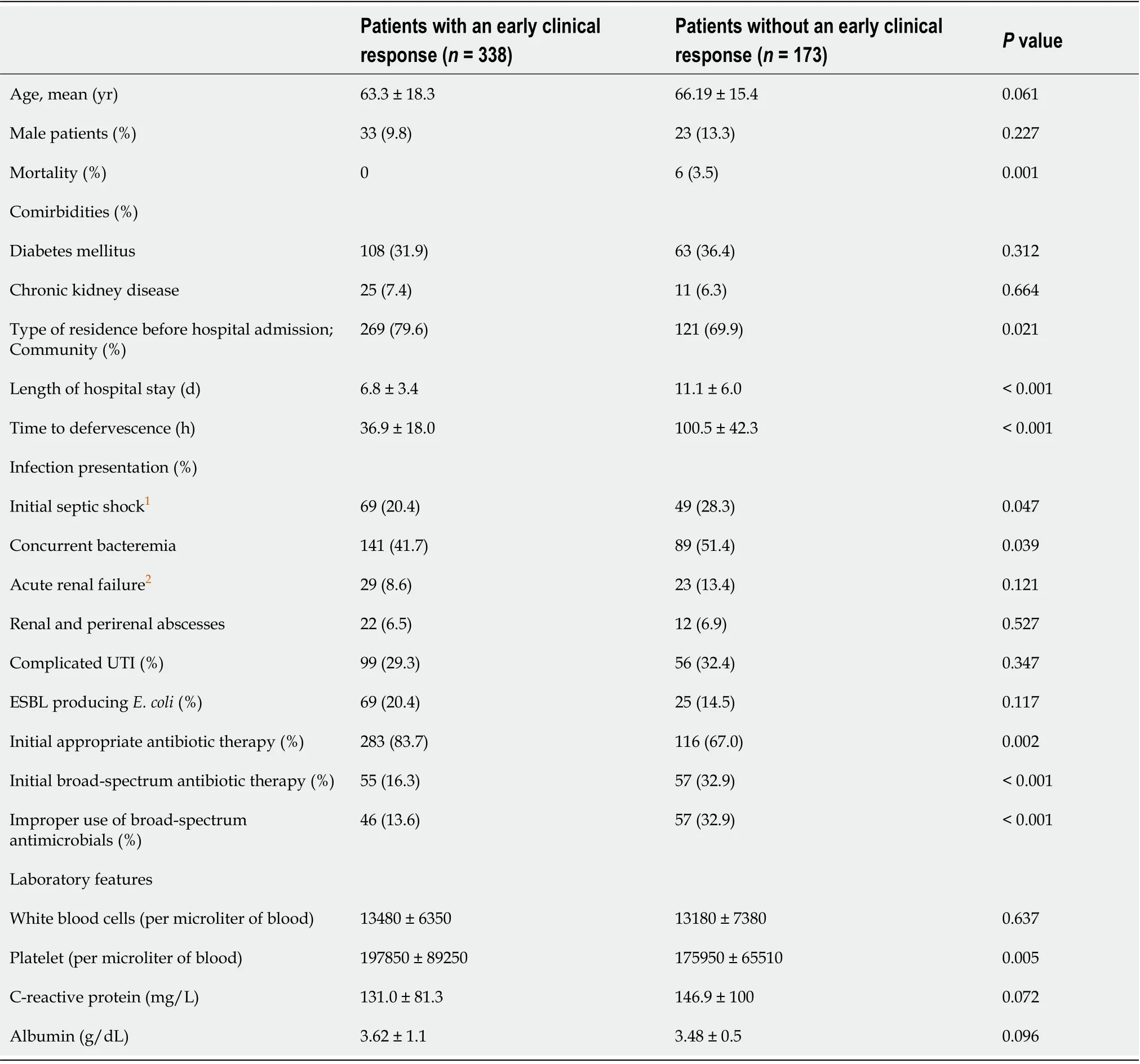
Table 1 Characteristics of patients with community-onset urinary tract infection caused by Escherichia coli
DISCUSSION
In this study,66.1% of the patients with community-onsetE.coliUTIs had an early clinical response.The patients with early clinical response had a 4.3 day shorter stay,and a 64 h shorter time to defervescence.The overall mortality rate was 1.2%;the deceased were all patients without an early clinical response.Severe presentations,including initial septic shock,concurrent bacteremia and acute renal failure complications,were associated with high morbidity and mortality[3,10,11].In this study,initial septic shock and concurrent bacteremia were significantly higher in patients without an early clinical response;however,initial septic shock,concurrent bacteremia,and acute renal failure were not associated with an early clinical response.Inappropriate antibiotic therapies to treat UTIs had poorer clinical outcomes,such as a lower cure rate,longer hospital stays[12],and higher relapse rates[13].As expected,our study observed that patients who received initial,appropriate antimicrobials had a 2.4 fold increase in developing an early clinical response.ESBL-producingE.coliis a major obstacle to initial,appropriate UTI antibiotic therapy and an important reason for the use of initial broad-spectrum antimicrobials.In this study,more than 20% of patientsreceived an initial broad-spectrum antibiotic therapy.However,initial broad-spectrum antibiotic therapy did not correlated with an early clinical response(OR = 0.614.95%CI:0.330-1.141,P =0.123).Moreover,63.4% of cases of initial broad-spectrum antibiotic therapy were considered unnecessary based onin vitroantimicrobial susceptibility testing.This finding suggests that the use of broad-spectrum antimicrobials must be limited to patients suspected of having UTIs caused by multidrug resistantE.coli.The clinical features and the antibiotic susceptibility pattern of the causative pathogens differ from patients residing in a healthcare facility and those living at home[14].In this study,the proportion of patients with an early clinical response was significantly different according to the type of residence before admission,and residence in a healthcare facility before admission was a poor predictive risk for an early clinical response.A previous study reported that ESBL production alone was not associated with adverse treatment outcomes in patients with community-associated UTIs[15].Similarly,our study showed that ESBL producingE.coliwas not a poor predictive factor for an early clinical response.
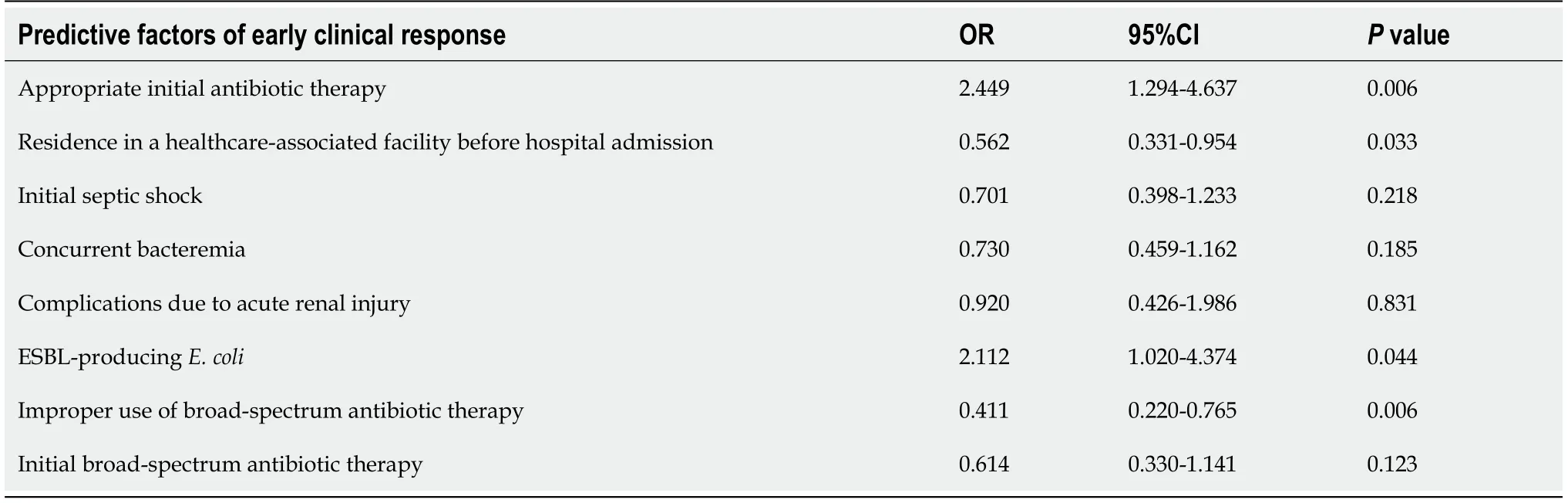
Table 2 Identification of predictive factors of early clinical response in using multiple logistic regression analysis
CONCLUSION
This study has some limitations.First,it is a retrospective study performed in a single university hospital.Second,this study included a high proportion of patients with severe UTIs,which may limit the generalization of our results to UTIs in outpatient clinics.The patients with an early clinical response in community-onsetE.coliUTIs had a shorter length of stay and a faster time to defervescence.Residence in a healthcare facility before admission was significantly related to a poor early clinical response.Appropriate initial antibiotic therapy was significantly related to an early clinical response.But,initial broad-spectrum antibiotic therapy or improper use of broad-spectrum antimicrobials was not associated with an early clinical response.And,severe presentations such as initial septic shock,concurrent bacteremia,and acute renal failure,were not associated with an early clinical response in communityonset UTIs.
ARTICLE HIGHLIGHTS
Research background
Urinary tract infection(UTI)often requires hospitalization,and patients with severe presentations,including sepsis and other complications,have a mortality rate of 6.7%-8.7%.It is necessary to evaluate the clinical response of patients with UTIs after 72 h of antibiotic therapy as poor clinical response after 72 h of antibiotic therapy has been related to clinical failure.There has been an increase in the incidence of communityonset UTIs due to extended-spectrum β-lactamase(ESBL)-producingEscherichia coli(E.coli).These findings have increased the use of initial broad-spectrum antimicrobials in patients with UTIs.However,use of broad-spectrum antimicrobials result in nosocomial acquisition of antimicrobial-resistant bacteria or occurrence ofClostridium difficileinfections.
Research motivation
The assessment of predictive factors for early clinical response may be helpful in the treatment of community-onset UTIs.
Research objectives
The primary aim of this study was to evaluate the clinical significance of early clinical response in community-onsetE.coliUTIs and the impact of severe presentations and initial antibiotic therapy on this early clinical response.
Research methods
This retrospective study was conducted at Wonkwang University Hospital in South Korea between January 2011 and December 2017.Hospitalized patients(aged ≥ 18 years)who were diagnosed with community-onsetE.coliUTI were enrolled in this study.Patients who were transferred to another hospital during treatment and those who had other concurrent infectious diseases were excluded.
Research results
A total of 511 hospitalized patients were included.Among them,66.1% of the patients had an early clinical response.Patients with an early clinical response had a shorter length of hospital stay(4.3 d)and an earlier defervescence(64 h)than those without an early clinical response.An appropriate initial antibiotic therapy(OR = 2.449,P =0.006),ESBL-producingE.coli(OR = 2.112,P =0.044),and a stay in a healthcare facility before admission(OR = 0.562,P =0.033)were the factors associated with an early clinical response.However,the initial broad-spectrum antibiotic therapy or initial severe presentations such as initial septic shock,concurrent bacteremia,and acute renal failure did not impact early clinical response.
Research conclusions
Patients with an early clinical response to community onsetE.coliUTI had a shorter length of hospital stay and an earlier defervescence.Appropriate initial antibiotic therapy was a good predictive factor for an early clinical response.However,initial broad-spectrum antibiotic therapy or initial severe presentation did not impact early clinical response.Physicians need to restrictively use initial broad-spectrum antimicrobials to treat patient suspected of having multi-drug resistant pathogens.
Research perspectives
Initial appropriate antibiotic therapy was a good predictive factor for an early clinical response.However,both the initial use of broad-spectrum antimicrobials and improper broad-spectrum antibiotic therapy did not improve the early clinical response in patients with community-onset UTI.The study results suggest that initial broad-spectrum antimicrobials should be used to treat patients suspected with multidrug resistant pathogenic infection,instead of patients with septic shock,concurrent bacteremia,and acute renal failure.
杂志排行
World Journal of Clinical Cases的其它文章
- Role of monoclonal antibody drugs in the treatment of COVID-19
- Review of simulation model for education of point-of-care ultrasound using easy-to-make tools
- Liver injury in COVID-19:A minireview
- Transanal minimally invasive surgery vs endoscopic mucosal resection for rectal benign tumors and rectal carcinoids:A retrospective analysis
- Impact of mTOR gene polymorphisms and gene-tea interaction on susceptibility to tuberculosis
- Establishment and validation of a nomogram to predict the risk of ovarian metastasis in gastric cancer:Based on a large cohort
