Massive gastrointestinal bleeding caused by a Dieulafoy’s lesion in a duodenal diverticulum: A case report
2020-04-08ZhiWeiHeLingZhongHuiXuHuaShiYangMeiWangXiaoCongLiu
Zhi-Wei He, Ling Zhong, Hui Xu, Hua Shi, Yang-Mei Wang, Xiao-Cong Liu
Zhi-Wei He, Ling Zhong, Hui Xu, Hua Shi, Yang-Mei Wang, Department of Gastroenterology and Hepatology, Ziyang First People’s Hospital, Ziyang 641300, Sichuan Province, China
Xiao-Cong Liu, Department of Gastroenterology and Hepatology, Chengdu Second People's Hospital, Chengdu 610017, Sichuan Province, China
Abstract BACKGROUND Dieulafoy’s lesion is a rare vascular abnormality characterized by a small abnormally dilated artery that runs a tortuous course in the submucosa. There is usually no ulcer present in Dieulafoy’s lesions and the overlying mucosa is most often normal. Bleeding caused by a Dieulafoy’s lesion is usually urgent, massive,life-threatening and prone to recurrence. Dieulafoy’s lesions have been reported throughout the digestive tract although the majority of them have been found in the upper digestive tract especially the stomach and duodenum. However, a Dieulafoy’s lesion occurring inside a duodenal diverticulum is very rare.CASE SUMMARY A 74-year-old Asian male with epigastric pain, hematemesis and melena was admitted to our clinic. Before admission, the patient had vomited 500 mL of dark red blood, and passed 200 g of black tarry stool. Conservative management was first undertaken as the patient had not been fasting. However, hemorrhage recurred and the patient went into shock. Urgent endoscopy was performed and a diverticulum of 1.8 cm × 1.2 cm × 0.8 cm was found on the anterior wall of the descending duodenum. The diverticulum was covered with a blood clot. After the clot was removed, an artery stump was observed in the diverticulum with a diameter of 2-3 mm. Two titanium hemostatic clips were inserted to clamp the vessel stump. The patient was discharged 7 d post-endoscopy and followed for 6 mo with no recurrence.CONCLUSION This case was diagnosed with a Dieulafoy’s lesion inside a duodenal diverticulum which has rarely been reported. Hematemesis was stopped by clamping the vessel stump with titanium clips. No complications occurred.
Key Words: Dieulafoy’s lesion; Duodenal diverticulum; Gastrointestinal bleeding;Endoscopy; Hemostatic clip; Case report
INTRODUCTION
Dieulafoy’s lesion is a rare vascular abnormality characterized by a small artery with an abnormally dilated caliber that runs a tortuous course in the submucosa. Bleeding is thought to be caused by a submucosal artery causing pressure necrosis of the overlying submucosa and mucosa in the absence of an ulcer. Bleeding caused by Dieulafoy’s lesions is usually urgent, massive, life-threatening and prone to recurrence. Dieulafoy’s lesions have been reported throughout the digestive tract although the majority of them were found in the upper digestive tract, including the stomach and duodenum. However, a Dieulafoy’s lesion occurring inside a duodenal diverticulum is very rare. Here, we report a case of massive hematemesis caused by a Dieulafoy’s lesion which was located inside a duodenal diverticulum.
CASE PRESENTATION
Chief complaints
A 74-year-old man was admitted to our clinic with epigastric pain, hematemesis and melena.
History of present illness
The patient complained of epigastric pain for 3 d. One day before he was admitted, the patient had hematemesis consisting of 500 mL of dark red liquid, followed by 200 g of black tarry stool. The patient felt dizzy, weak and had palpitations.
History of past illness
The patient denied a history of hypertension, diabetes, and other relevant illness. He also denied ever taking any medications including non-steroidal anti-inflammatory agents, anticoagulants and herbals.
Family history
The patient denied any positive family history.
Physical examination
Upon admission, his temperature was 36.5°C, heart rate was 97 bpm, blood pressure was 100/76 mmHg, and respiration rate was 20 breaths/minute. The patient was conscious, anemic looking, and bowel sounds were active.
Laboratory examinations
Blood analysis revealed an erythrocyte count of 2.92 × 1012/L, hemoglobin of 91 g/L,and platelet count of 152 × 109/L. Fecal occult blood test was (+). Coagulation test revealed normal prothrombin time and international normalized ratio.
Imaging examinations
Abdominal CT scan (no contrast was used) upon admission showed no obvious abnormalities of the liver, gallbladder, biliary tract, spleen and pancreas.
Treatment upon admission
After admission, the patient had nothing per os, and received intravenous fluid resuscitation and proton pump inhibitors. As the patient had eaten 2 h before admission, urgent endoscopy was postponed.
Progression of the disease and further diagnostic work-up
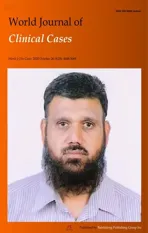
In the evening, the patient had 2 bouts of melena with a total weight of approximately 600 g, followed by increased heart rate (108 bpm), decreased blood pressure (88/50 mmHg) and hemoglobin (56 g/L). Red blood cell transfusion was given, and then urgent upper gastrointestinal endoscopy was performed. Endoscopy revealed a huge diverticulum (about 1.8 cm × 1.2 cm × 0.8 cm) in the anterior wall of the descending duodenum (close to the papilla) with a massive blood clot inside (Figure 1). A vessel stump with a diameter of 2-3 mm was exposed after removal of the clot (Figure 2).
FINAL DIAGNOSIS
The final diagnosis was massive upper gastrointestinal bleeding caused by a Dieulafoy’s lesion inside a duodenal diverticulum.
TREATMENT
Two titanium clips were inserted to clamp the vessel stump (Figure 3). No active bleeding was observed after washing. Oral feeding with a cool liquid diet was initiated on the 1stday post-endoscopy.
OUTCOME AND FOLLOW-UP
No more hematemesis occurred, and melena stopped 3 d after endoscopy. The patient was discharged from hospital on the 7thday, and followed for 6 mo with no recurrence.
DISCUSSION
Dieulafoy’s lesion is a rare cause of digestive tract hemorrhage. It is a rare vascular abnormality characterized by a small abnormally dilated artery that runs a tortuous course in the submucosa[1]. Dieulafoy’s lesions are believed to be congenital, but they have been reported to occur more frequently with advancing age[2]. Dieulafoy’s lesions account for 1%-5.8% of acute gastrointestinal bleeding[3,4], but they often present with urgent and massive bleeding usually leading to shock, and even death. They also have a high rate of recurrence. Sometimes, the bleeding may cease spontaneously due to a drop in blood pressure and/or the formation of a blood clot. The arterial stump may retract and remain hidden beneath the mucosa making it very difficult to detect by endoscopy, or even surgery. Thus, a Dieulafoy’s lesion can be life-threatening.
Endoscopy has been reported to be the most effective method in diagnosing up to 70% of Dieulafoy’s lesions[2]. The endoscopic findings of Dieulafoy’s lesions are characterized by an isolated protruding vessel usually surrounded by normal mucosa or less commonly a small round or oval superficial ulcer[5,6]. The diameter of the vessel stump is usually between 1-3 mm[7]. The lesion may be actively bleeding including spurting or oozing, otherwise, it might be covered by a blood clot[5].
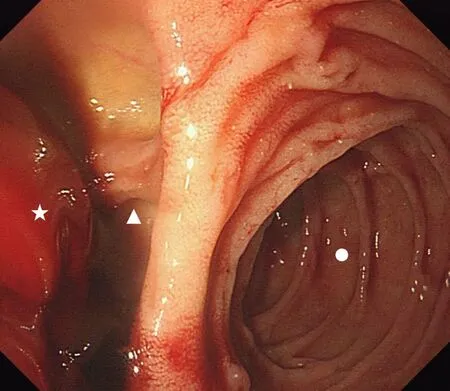
Figure 1 Endoscopic view of the diverticulum located in the descending duodenum. Circle: Descending duodenum; Triangle: Diverticulum;Pentagram: Blood clot.
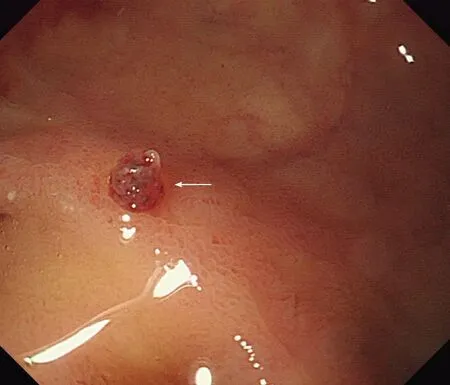
Figure 2 Endoscopic view of the isolated protruding artery of Dieulafoy disease after washing away the blood clot. Arrow: Artery stump.
Dieulafoy’s lesions have been reported throughout the digestive tract with 8% in the esophagus, 71% in the stomach, 15% in the duodenum, 1% in the intestine, 2% in the colon, 2% in the rectum and 1% in gastric anastomosis[3]. Santos reported a case of a Dieulafoy’s lesion located in the gallbladder in 2020[1]. It is also reported that Dieulafoy’s lesions have been found outside the gastrointestinal tract, such as in the bronchus[8,9]. However, Dieulafoy’s lesions occurring inside a duodenum diverticulum are rare, with only 4 cases reported previously[10-13]. In the current case, the diverticulum was located in the descending duodenum where lesions are difficult to observe. There were no signs of inflammation or ulcer in the diverticulum, and the only clue was the blood clot. The exposed arterial stump could easily have been missed if the endoscopist had ignored the clot or did not wash away the clot to observe the inside of the diverticulum.
Figure 3 Two titanium clips were inserted to clamp the vessel stump.
Due to urgent, massive, arterial bleeding, it is often difficult to stop the hemorrhage using common conservative therapies. Treatment by endoscopy has become the preferred and most effective way of managing a Dieulafoy’s lesion, with a reported success rate of over 90%[3]. Commonly used endoscopic hemostatic procedures include electrocoagulation, thermocoagulation, local epinephrine injection, sclerotherapy,banding, and hemoclips[7,14]. Mechanical hemostasis is considered to be more effective than injection or thermal treatment[14], and hemoclips are easier to manipulate compared to banding. The clips close the vessel stump, and a subsequent inflammation reaction forms granulation tissue which seals off the vessel. The clips fall off after 1-3 wk.
CONCLUSION
We report the case of an adult patient with massive hemorrhage of the digestive tract caused by a Dieulafoy’s lesion inside a duodenal diverticulum discovered and treated by endoscopy. Hemostasis was achieved by endoscopic placement of hemostatic clips.There were no complications. The patient was followed for 6 mo without recurrence.
杂志排行
World Journal of Clinical Cases的其它文章
- Relationship between non-alcoholic fatty liver disease and coronary heart disease
- Remission of hepatotoxicity in chronic pulmonary aspergillosis patients after lowering trough concentration of voriconazole
- Endoscopic submucosal dissection as alternative to surgery for complicated gastric heterotopic pancreas
- Observation of the effects of three methods for reducing perineal swelling in children with developmental hip dislocation
- Predictive value of serum cystatin C for risk of mortality in severe and critically ill patients with COVID-19
- Sleep quality of patients with postoperative glioma at home