Bladder perforation caused by long-term catheterization misdiagnosed as digestive tract perforation: A case report
2020-04-08BinWuJingWangXuJianChenZhongChengZhouMingYuanZhuYiYuShenZhengXiangZhong
Bin Wu, Jing Wang, Xu-Jian Chen, Zhong-Cheng Zhou, Ming-Yuan Zhu, Yi-Yu Shen, Zheng-Xiang Zhong
Bin Wu, Jing Wang, Xu-Jian Chen, Zhong-Cheng Zhou, Ming-Yuan Zhu, Yi-Yu Shen, Zheng-Xiang Zhong, Department of Hepatobiliary Surgery, The Second Affiliated Hospital of Jiaxing University, Jiaxing 314000, Zhejiang Province, China
Abstract BACKGROUND Spontaneous bladder rupture is relatively rare, and common causes of spontaneous bladder rupture include bladder diverticulum, neurogenic bladder dysfunction, gonorrhea infection, pelvic radiotherapy, etc. Urinary bladder perforation caused by urinary catheterization mostly occurs during the intubation process.CASE SUMMARY Here, we describe an 83-year-old male who was admitted with 26 h of middle and upper abdominal pain and a history of long-term catheterization. Physical examination and computed tomography of the abdomen supported the diagnosis of diffuse peritonitis, most likely from a perforated digestive tract organ.Laparoscopic exploration revealed a possible digestive tract perforation. Finally, a perforation of approximately 5 mm in diameter was found in the bladder wall during laparotomy. After reviewing the patient’s previous medical records, we found that 1 year prior the patient underwent an ultrasound examination showing that the end of the catheter was embedded into the mucosal layer of the bladder. Therefore, the bladder perforation in this patient may have been caused by the chronic compression of the urinary catheter against the bladder wall.CONCLUSION For patients with long-term indwelling catheters, there is a possibility of bladder perforation, which needs to be dealt with quickly.
Key Words: Bladder perforation; Catheterization; Misdiagnosed; Case report
INTRODUCTION
Bladder perforation is commonly seen in trauma or iatrogenic injury[1], such as transurethral surgery or pelvic intraoperative injury[2,3]. Spontaneous bladder rupture is relatively rare, and common causes of spontaneous bladder rupture include bladder diverticulum, neurogenic bladder dysfunction, gonorrhea infection and pelvic radiotherapy, among others[4]. A urinary bladder perforation caused by urinary catheterization mostly occurs during the intubation process. Here, we describe a patient who had a bladder perforation combined with peritonitis due to the long-term indwelling of the catheter.
CASE PRESENTATION
Chief complaints
An 83-year-old male patient came to our hospital for emergency treatment due to 26 h of middle and upper abdominal pain.
History of present illness
The patient had mid-upper abdominal pain 26 h ago, a persistent pain, severe with nausea but no vomiting. There was no waist and back pain, no chest tightness,shortness of breath, but the patient felt palpitations and fatigue. The patient has had chills since abdominal pain occurred, and the degree of abdominal pain has been increasing since the onset. We observed that the patient had a catheter inserted, and there was about 50 mL of yellow urine in the urine bag.
History of past illness
After a careful medical history inquiry, the patient was found to have been bedridden for a long period of time and suffered from many diseases, including hypertension,cardiac pacemaker implantation, history of atrial fibrillation, chronic obstructive pulmonary disease, prostatic hyperplasia and catheter indwelling status. The patient was diagnosed with benign prostatic hyperplasia 8 years ago due to symptoms of impaired urination, but he refused surgery. Three years ago, the patient could not rule out urination because of prostate hyperplasia, so he chose catheterization. For so many years, patients have been living with urinary catheters, so urinary tract infections often occur.
Physical examination
When the patient came to the hospital, his temperature was 37.2°C, heart rate was 56 bpm, respiratory rate was 19 breaths per minute, blood pressure was 197/70 mmHg and oxygen saturation was 97%. Physical examination revealed slightly swollen abdomen and no obvious prominent lumps. Abdominal palpation showed tense abdominal muscles, a platy abdomen and obvious tenderness in the whole abdomen accompanied by rebound pain. Percussion of the abdomen indicated the presence of fluid in the abdominal cavity. Auscultation of the abdomen indicated that the sound of bowel movement in the abdominal cavity was slightly weakened.
Laboratory examinations
Routine blood tests showed that the patient’s leukocyte count did not increase significantly (7.38 × 109/L), and the percentage of neutrophils was 91.2% with an increased hypersensitive C-reactive protein (132.81 mg/L). The patient’s red blood cell count was normal (4.92 × 109/L), but the platelet count was low (80 × 109/L). The significant increase in troponin (50 ng/L) and brain natriuretic peptide (630.53 pg/mL)indicated that the function of the patient’s heart was poor. Prothrombin, d-dimers and partial thromboplastin times were normal.
Imaging examinations
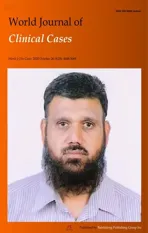
Computed tomography of the abdomen revealed a small amount of free gas under the diaphragm and edema in part of the small intestine and intestinal wall with surrounding exudation. There was gas accumulation in the middle and upper abdomen and intestinal cavity, a small amount of effusion around the right liver,multiple cystic foci in the liver and cirrhosis. The distal end of the common bile duct showed calculi with multiple gallbladder calculi. The bladder wall was thickened with multiple bladder diverticulum and gas accumulation (Figure 1).
FINAL DIAGNOSIS
The on duty physician first considered a diagnosis of diffuse peritonitis most likely due to a perforation of the digestive tract based on the above physical examination features and imaging data.
TREATMENT
Due to the advanced age of the patient with many basic diseases, the patient was at high risk for surgical treatment. After consultation with the patient’s family, the patient underwent emergency laparoscopic exploration. During the operation, dark red fluid accumulation was observed around the liver (Figure 2A) and a large amount of purulent fluid and pus adhesions were observed in the abdominal cavity (Figure 2B and C) when the laparoscope was inserted into the abdominal cavity, indicating that a digestive tract perforation was more likely. We performed exploratory laparotomy in the hope of finding the location of the perforation.
OUTCOME AND FOLLOW-UP
Finally, a hole of approximately 5 mm in diameter was found in the bladder wall(Figure 3). We repaired the hole using this method to suture all layers of bladder wall with 2-0 absorbable thread. We replaced a new catheter (18F Foley catheter) and kept it in the bladder to drain urine. Finally, we washed the abdominal cavity with normal saline, and closed the abdominal cavity with an indwelling drainage tube. It is a pity that the patient chose to continue the indwelling catheter because of poor cardiopulmonary function and unable to withstand partial prostatectomy. After more than a month, the patient recovered and left the hospital.
After reviewing the patient’s previous medical records, we found that 1 year prior,the patient underwent an ultrasound examination showing that the end of the catheter was embedded in the mucosal layer of the bladder (Figure 4). Therefore, the bladder perforation in this patient may have been caused by the chronic compression of the urinary catheter against the bladder wall. This bladder perforation may not occur if the ultrasound results were taken seriously and appropriate action had been taken by the physician.
DISCUSSION
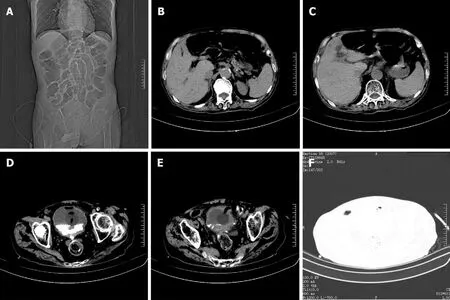
Figure 1 Computed tomography image of the patient’s abdomen before surgery. A: The catheter was indwelling, and the intestinal cavity was dilated;B: A small amount of free gas in the abdominal cavity; C: A small amount of effusion around the liver and spleen; D and F: Air collected in the bladder; E: The bladder wall was thickened, and the end of catheter was sighted in the bladder wall.
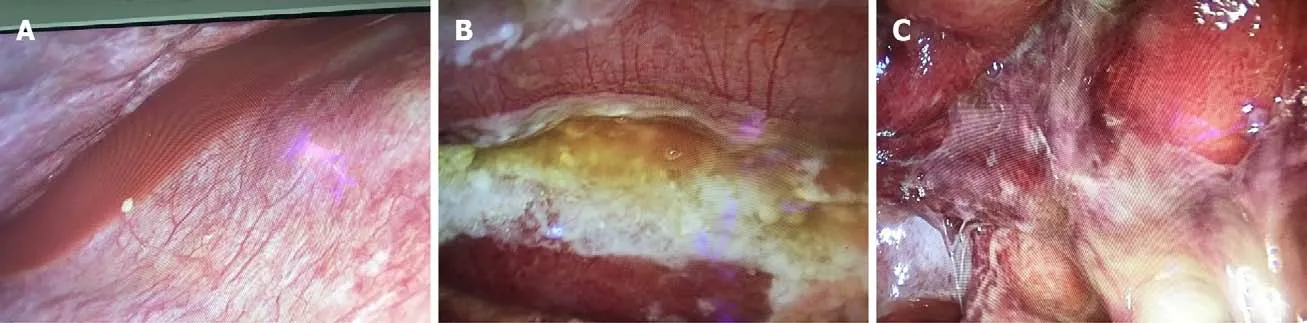
Figure 2 Images from the laparoscopic exploration. A: Dark red fluid was found accumulated around the liver; B and C: A large amount of purulent fluid and purulent moss can be seen in the abdominal cavity and intestine.
In this case, the patient had a bladder perforation combined with peritonitis due to a long-term indwelling urinary catheter. Although it was not a spontaneous rupture of the bladder, it is rare in clinical practice. With the aging of the population, there is an increasing number of elderly and high-risk patients with long-term indwelling urinary catheters. Long-term indwelling urethral catheters are associated with many risks,including urinary tract infection, catheter shedding, difficult extubation, urethral stricture and bladder mucosal damage, among others. Serious cases lead to urethral perforation, which is extremely rare[5]. This is because the balloon catheter is left in the bladder normally. Long-term continuous catheterization causes the bladder to be nonfilled, which reduces the bladder volume. The top of the catheter becomes embedded in the bladder mucosa, resulting in local ischemia, mucosal damage and chronic inflammation, which can lead to bladder structure abnormalities, bladder wall necrosis and perforation.
In this case, an ultrasound examination showed that the urethral catheter end was embedded into the mucosal layer of the bladder 1 year before. It is not clear whether this injury was the site of the perforation. It should be noted that patients who require long-term indwelling catheterization tend to be frail elderly patients with poor reactivity and insensitivity to pain. In the early stage, the bladder perforation is small,the pressure in the bladder is low and the speed and volume of urine outflow are small. Therefore, the patient often has no obvious symptoms, the disease progresses slowly and it is easy to delay treatment resulting in diffuse peritonitis, which is lifethreatening[6,7].
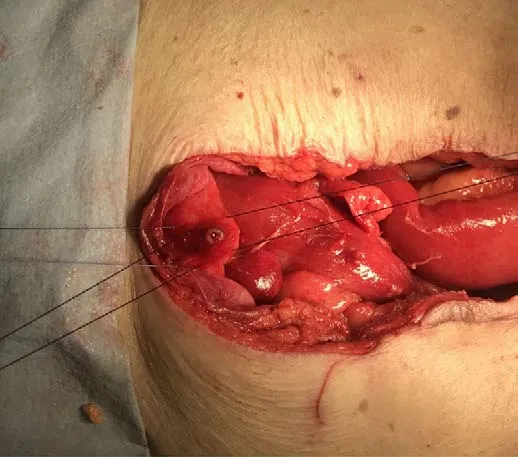
Figure 3 Intraoperative photograph of the patient. A perforation is seen in the upper wall of the bladder with a diameter of approximately 5 mm.

Figure 4 Ultrasound image from a year prior. Ultrasonic image showing the insertion of the urinary catheter terminal into the mucosal layer of the bladder.
In this case, there was still a large amount of urine outflow through the catheter, and diffuse peritonitis had occurred indicating that the bladder perforation of this patient was a chronic process. Therefore, it is difficult to diagnose such cases and led to a misdiagnosis of digestive tract perforation. Scheinet al[8]considered the diagnosis of spontaneous bladder perforation to be challenging and usually made during open surgery[8]. A patient with T1 paraplegia had a bladder perforation due to intermittent self-catheterization reported by Martinet al[9]. This case highlighted the fact that a preoperative diagnosis of bladder perforation in T1 paraplegics with no abdominal sensation is very difficult[9], and the delay in diagnosis and treatment is the main cause of death in patients with bladder perforation[10,11].
Some researchers have suggested that cystostomy should be performed in patients with a long-term indwelling catheter. The possible complications of long-term indwelling catheters can be avoided. However, the proportion of patients with cystostomy is very low clinically, which may be related to the high age of most patients and the high risk of operation. Some have also proposed that the urethral catheter should be intermittently closed in the process of catheterization so that the bladder is in the filling state for most of the time thus reducing the pressure of the urethral catheter on the bladder mucosa.
Regular replacement of urinary catheters can reduce urinary tract infections and avoid compression of the bladder mucosa in the same area, but the optimal time to replace urinary catheters is still unclear and needs to be confirmed by more clinical studies. The use of a catheter with a smooth, flexible end can also reduce injury to the bladder wall. When the patient has mild symptoms or the bladder mucosa is found to be slightly injured by ultrasound examination, timely treatment should be provided to avoid misdiagnosis and delay the disease[12]. In this case, if a preoperative ultrasound examination[13]or cystography[14]is performed, then it may be helpful to locate the perforation during surgery. Of course, the possibility of a bladder perforation should be considered in patients with this kind of long-term indwelling catheter combined with peritonitis.
CONCLUSION
For patients with long-term indwelling catheters, there is a possibility of bladder perforation, which needs to be dealt with quickly.
杂志排行
World Journal of Clinical Cases的其它文章
- Relationship between non-alcoholic fatty liver disease and coronary heart disease
- Remission of hepatotoxicity in chronic pulmonary aspergillosis patients after lowering trough concentration of voriconazole
- Endoscopic submucosal dissection as alternative to surgery for complicated gastric heterotopic pancreas
- Observation of the effects of three methods for reducing perineal swelling in children with developmental hip dislocation
- Predictive value of serum cystatin C for risk of mortality in severe and critically ill patients with COVID-19
- Sleep quality of patients with postoperative glioma at home