lmpact of Postdilation on lntervention Success and Long-Term Major Adverse Cardiovascular Events (MACE) among Patients with Acute Coronary Syndromes
2020-03-25TuranErdoanMDHakanDumanMDMustafaetinMDSavazerMDkselinierMDEceUstaMDMustafaUstaMDTuncayMD
Turan Erdoğan,MD ,Hakan Duman,MD ,Mustafa Çetin,MD ,Savaş Özer,MD ,Göksel Çinier,MD ,Ece Usta,MD ,Mustafa Usta,MD ,Tuncay Kırış,MD
1 Department of Cardiology,Faculty of Medicine,Recep Tayyip Erdoğan University,Rize,Turkey
2 Department of Cardiology,Recep Tayyip Erdoğan Education and Research Hospital,Rize,Turkey
3 Department of Cardiology,Kaçkar State Hospital,Rize,Turkey
4 Department of Cardiology,Atatürk Education and Research Hospital,İ zmir Katip Çelebi University,İ zmir,Turkey
Abstract
Keywords:postdilation;acute coronary syndromes;percutaneous coronary intervention
lntroduction
Acute coronary syndromes (ACS) are still a major cause of death worldwide despite recent advances in diagnostic and therapeutic tools.ST -segment elevation myocardial infarction (STEMI) merits particular attention since establishment of coronary perfusion as soon as possible is of utmost importance to prevent adverse cardiovascular events [1,2].Coronary angiography and subsequent percutaneous coronary intervention (PCI) ifinecessary is the method of choice for myocardial revascularization.Stent implantation has replaced balloon angioplasty in most cases as overwhelming evidence suggests that the former reduces the risk of restenosis.Challenges in stent implantation due to the characteristics of coronary arteries and atherosclerotic lesions caused operators to develop feasible strategies depending on the lesion location,diameter,and morphology.Dilation by use ofinoncompliant balloons after stent implantation is one of the most frequently used techniques to address these challenges [3].Because incomplete stent expansion is a major cause of stent thrombosis and in-stent restenosis,postdilation has been considered an important technique to help optimal stent implantation [4-6].Patients with ACS were found to be particularly prone to stent malapposition because of the presence of an inf ammatory milieu and coronary vasoconstriction.These findings suggested that postdilation with high pres sures in the context of ACS would reduce stent malapposition and improve outcomes.In contradiction,other studies demonstrated controversial results and some indicated a signal toward harm such that postdilation impaired final Thrombolysis in Myocardial Infarction (TIMI) flow,increased the risk of tar get vessel revascularization,and predicted adverse clinical outcomes [7-9].Myocardial blush grade (MBG) is considered to be a reliable indicator of tissue perfusion and is associated with reduced long-term mortality and morbidity in patients with ACS [10].Despite several studies evaluating the ef fect of postdilation on post-PCI angiographic parameters,there are no data to date on the impact of postdilation on MBG.Thus,we aimed to evaluate the ef fect of postdilation on MBG and long-term major cardiovascular outcomes.
Methods
Study Population
This study,with a prospective observational cohort study design,was conducted in the cardiology clinic in the Faculty of Medicine of Recep Tayyip Erdoğan University,Rize,Turkey.A total of 258 consecutive patients who presented with ACS (STEMI and non- ST-segment elevation myocardial infraction) and who underwent PCI during hospitalization between February 2017 and August 2017 were included in the study.The study was performed in accordance with the principles stated in the Declaration of Helsinki.The local ethics committee approved the study protocol.
Exclusion Criteria
Patients with previous coronary artery bypass graft operation,in-stent restenosis,chronic kidney disease,sepsis,pulmonary embolism,or cardiogenic shock and patients who were being medically treated were excluded from the study.
Demographic Data
Clinical characteristics,which consisted of multiple descriptors from each patient ’ s history and physical examination,of each patient were collected by physicians from cardiology clinics and were stored in the database of the coronary angio graphy laboratory at Recep Tayyip Erdoğan Education and Research Hospital.We recorded the baseline characteristics,including hypertension,presence of diabetes mellitus,smoking status,family history of premature coronary artery disease,and lipid parameters.
Selective Coronary Angiography and PCl Procedure
Diagnostic coronary angiography and PCI procedures for the study patients were performed by f ve different experienced interventional cardiologists,who were blinded to the other data.The use and administered dose ofinitroglycerin for intracoronary infusion and PCI-related preferences such as predilation,postdilation,stent length,and stent width were left to the discretion of the interventional cardiologist who performed the procedure.Medical treatments of the study patients were according to current guidelines.Three experienced investigators who were blinded to clinical parameters of the patients carefully reviewed the coronary angiograms for the measurements.
The timing of the selective coronary angiography and PCI were in accordance with current guidelines.Femoral artery puncture and the Judkins technique were performed in all cases.Multiple views were obtained in all patients,with visualization of the left anterior descending artery and left circumf ex coronary artery in at least four views and the right coronary artery in at least two views.Coronary angiograms were recorded in digital format for quantitative analysis.
On the f rst angiogram,we assessed the basal TIMI flow grade and collateral circulation of the culprit vessel.Variables obtained in the angiographic sequences such as TIMI flow grade,corrected TIMI frame count (cTFC),and TIMI myocardial perfusion grade were acquired immediately after PCI.
Epicardial blood flow was assessed by use of either TIMI flow grade [11] or cTFC [12],and myocardial perfusion was assessed by use of TIMI myocardial perfusion grade [11].To allow suff cient filling of the venous system and TIMI myocardial perfusion grading,cine filming was kept suff ciently long (> 10 s).
Thrombus burden was classif ed by the investigator prior to wire crossing based on the TIMI thrombus grade [13].
Coronary artery stenoses were classif ed as lesions of type A,B1,B2,and C [14].Lesion classif cation by the American College of Cardiology/American Heart Association system was based on 11 characteristics,including lesion length,lesion eccentricity,lesion tortuosity,lesion angle,lesion contour,calcif cation,total occlusion for less than 3 months,total occlusion for more than 3 months,ostial lesion,side branch involvement,and presence or absence of thrombus [14].
Medications
All patients were treated medically according to current guidelines [1].Patients were given loading doses of clopidogrel,ticagrelor,or prasugrel plus a loading dose of acetylsalicylic acid according to the preference of the invasive cardiologist who performed the procedure.
At the start of each procedure,10,000 IU heparin was administered intravenously.Coronary stenting directly,or followed by balloon angioplasty,was performed when patients were eligible.Stent and coronary artery diameters and predilation/postdilation details were recorded during PCI.After the procedure,patients were followed up in the coronary care unit until hemodynamic stabilization.
Laboratory Assays
Cardiac biomarker levels,including creatine kinase MB level,troponin I level,admission glucose level,and levels of inf ammatory markers,including leukocytes,were analyzed in the emergency department and used in the analyses as admission values.The lipid samples were drawn by venipuncture to perform routine blood chemistry tests after patients had fasted for at least 8 h.Glucose level,creatinine level,and lipid profile were determined by standard methods.White blood cell (leukocyte) counts were obtained with an automated cell counter (Gen-S,Coulter Corporation,Miami,FL,USA).Blood samples were obtained 4 h apart for the determination of peak creatine kinase MB and troponin levels.Troponin levels reference ranges was 0- 0.026.
Clinical Follow-up Parameters and Identif ciation of Major Cardiac Events
The follow-up period was 25 ± 1.7 months.Patient clinical data were obtained from physicians,from the data recording system of Recep Tayyip Erdoğan Education and Research Hospital,and by face-toface and/or telephone interviews.
Patients were followed up for any occurrence of major cardiac events (MACE),which included cardiovascular death,new heart failure,a cerebrovascular event,recurrent revascularization,reinfarction,and major bleeding.
Major bleeding was considered to be any intracranial bleeding (excluding microhemorrhages of 10 mm evident only on gradient-echo MRI),clinically overt signs of hemorrhage associated with a drop in hemoglobin level of 5 g/dL,or fatal bleeding (bleeding that directly results in death within 7 days) [15].
Statistical Analysis
Continuous variables were expressed as means ± standard deviations and categorical variables were presented as percentages.The variables were compared by a two-tailed Studentttest for continuous variables with a normal distribution or the Mann-WhitneyUtest for continuous variables with a nonnormal distribution.A chi-square test was used for the categorical variables.The effects of the various variables on MACE were calculated by Cox regression analysis.All statistical tests were two-tailed,and P < 0.05 was considered signif cant.All analyses were performed with SPSS version 15 (SPSS Inc.,Chicago,IL,USA).
Results
Study patients were followed up for 25 ± 1.7 months.During this period,65 patients (25.2%) had MACE.Among those patients,16 (24.6%) were female and the mean age was 67.38 years (standard deviation 1 1.98 years).Eighteen patients (7.0%) died,two (0.8%) had major bleeding,24 (9.3%) had decompensated heart failure,two had a cerebrovascular accident,two (0.8%) had a ventricular tachycardia episode,11 (4.3%) had stent thrombosis,15 (5.8%) had reinfarction,and 20 (7.8%) had revascularization.
Univariate analysis among patients who had undergone postdilation (n= 52,20.2%) and patients who had not undergone postdilation (n= 206,79.8%) revealed that stent length was longer (P < 0.001) and diabetes was more frequent (P = 0.089) among patients who had undergone postdilation,although the latter did not reach statistical signif cance (Table1).
We performed multivariate analysis to identify predictors of MACE during follow-up.Male sex (P = 0.047),MBG (P = 0.038),previous coronary artery disease (P = 0.030),and peak troponin level (P = 0.002) were found to be predictors of MACE (Table2).
No signif cant dif ference was noted between patients in whom postdilation had been performed and patients in whom postdilation had not been performed.There was no dif ference regarding MBG (P = 0.305),final TIMI flow grade (P = 0.218),and cTFC (P = 0.118) with use of clopidogrel,ticagrelor,or prasugrel in patients in whom postdilation had been performed.Postdilation was found to be neutral in predicting procedural success and long-term MACE.
Discussion
In the present study,we found that among patients who presented with ACS and had PCI during hospitalization,postdilation predicted neither shortterm PCI success as assessed by final TIMI flow grade,cTFC,and MBG nor MACE during followup.In addition,clopidogrel,ticagrelor,and prasugrel did not af fect outcomes in patients in whom postdilation had been performed.
In a previous study that included 405 patients with STEMI and treated by primary PCI,Tasal et al.[7] showed that postdilation did not reduce final TIMI flow and improved outcomes at 6 months.Compared with the present study,the number of patients in whom postdilation was performed was signif cantly higher (52 vs.20%) and only patients with STEMI were included.Similarly to our findings,no signif cant differences were noted between patients with postdilation and patients without postdilation regarding acute PCI success as assessed by final TIMI flow,cTFC,and MBG.However,they found that postdilation reduced the incidence of stent thrombosis and tar get vessel revascularization.No signif cant difference was noted between groups regarding the markers ref ecting myocardial damage and left ventricular ejection fraction,which was in accordance with our findings.In their study demonstrating that postdilation increased mortality,Zhang et al.[9] showed that postdilation did not increase the risk of coronary no reflow.Importantly,postdilation was performed in a higher proportion of patients (43.1%) than in our study.Furthermore,postdilation did not predict worse outcomes in the non- acute myocardial infarction subgroup.
Although Zhang et al.[9] demonstrated worse outcomes associated with postdilation,the causative mechanisms remained unknown.Other studies proposed that stent overexpansion secondary to balloon inf ation at very high pressures could be the underlying reason for adverse outcomes [16].Accordingly,Maekawa et al.[16] showed that although stent overexpansion reduced the risk of tar get vessel revascularization,but the incidence of heart failure in the overexpansion group was higher than that in the nonoverexpansion patients during intravascular ultrasound evaluation.Maekawa et al.suggested that distal microembolisms of thrombogenic material from the plaque that were stented with overexpansion were the possible cause.Similarly,Soylu et al.[8] showed that in patients with STEMI and treated by primary PCI,postdilation reduced final coronary flow evaluated by cTFC and TIMI scorein patients who did not have stent overexpansion.In contradiction to our results,in their retrospective study,which included 9000 STEMI patients,Fobert et al.[17] found that postdilation increased stent restenosis only in those patients in whom ticagrelor and prasugrel were not administered.On the other hand,a subsequent prospective study that included patients using ticagrelor and prasugrel showed the benef cial effect of postdilation on stent thrombosis and restenosis [18].
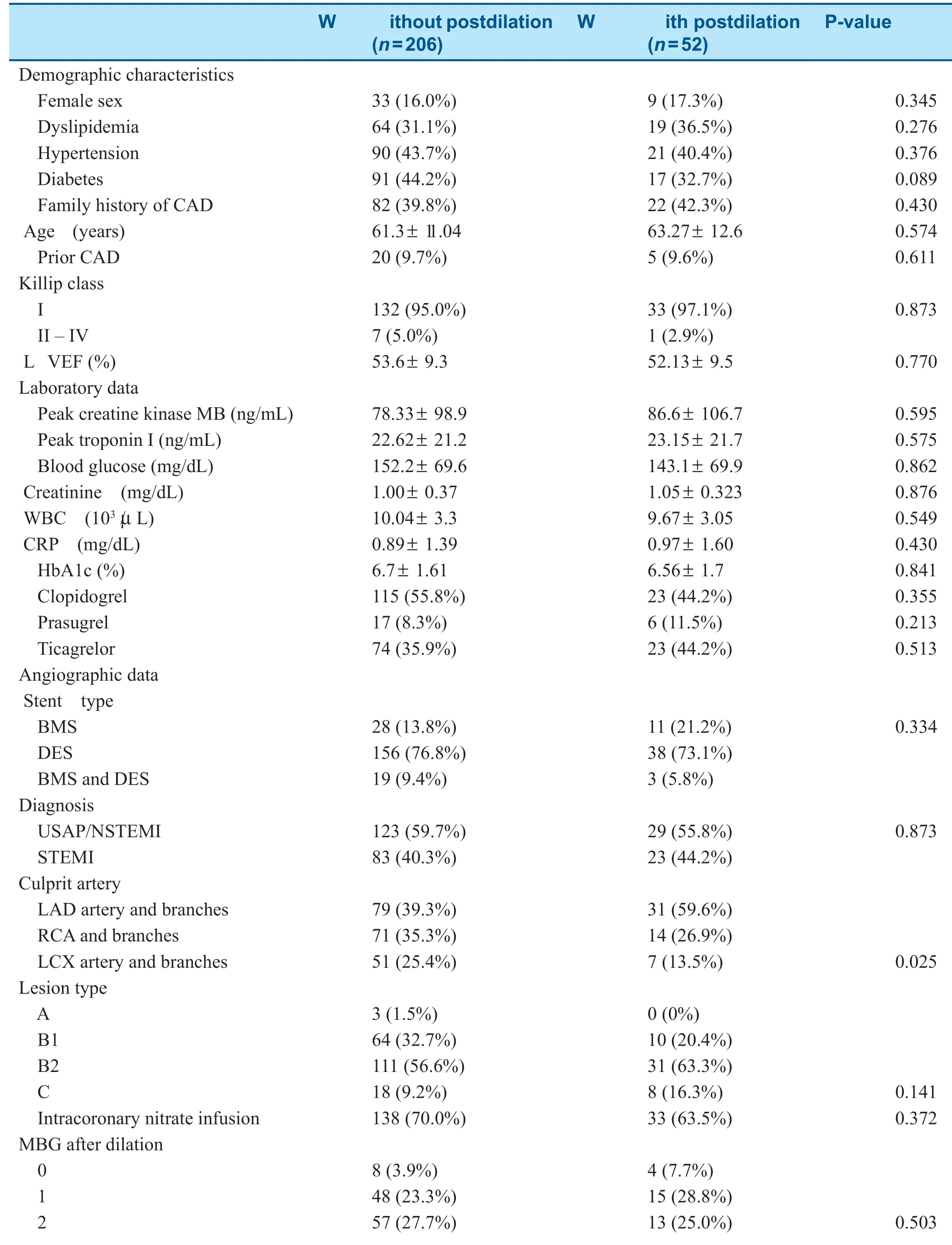
Table1 Characteristics of Study Patients According to Postdilation Status.
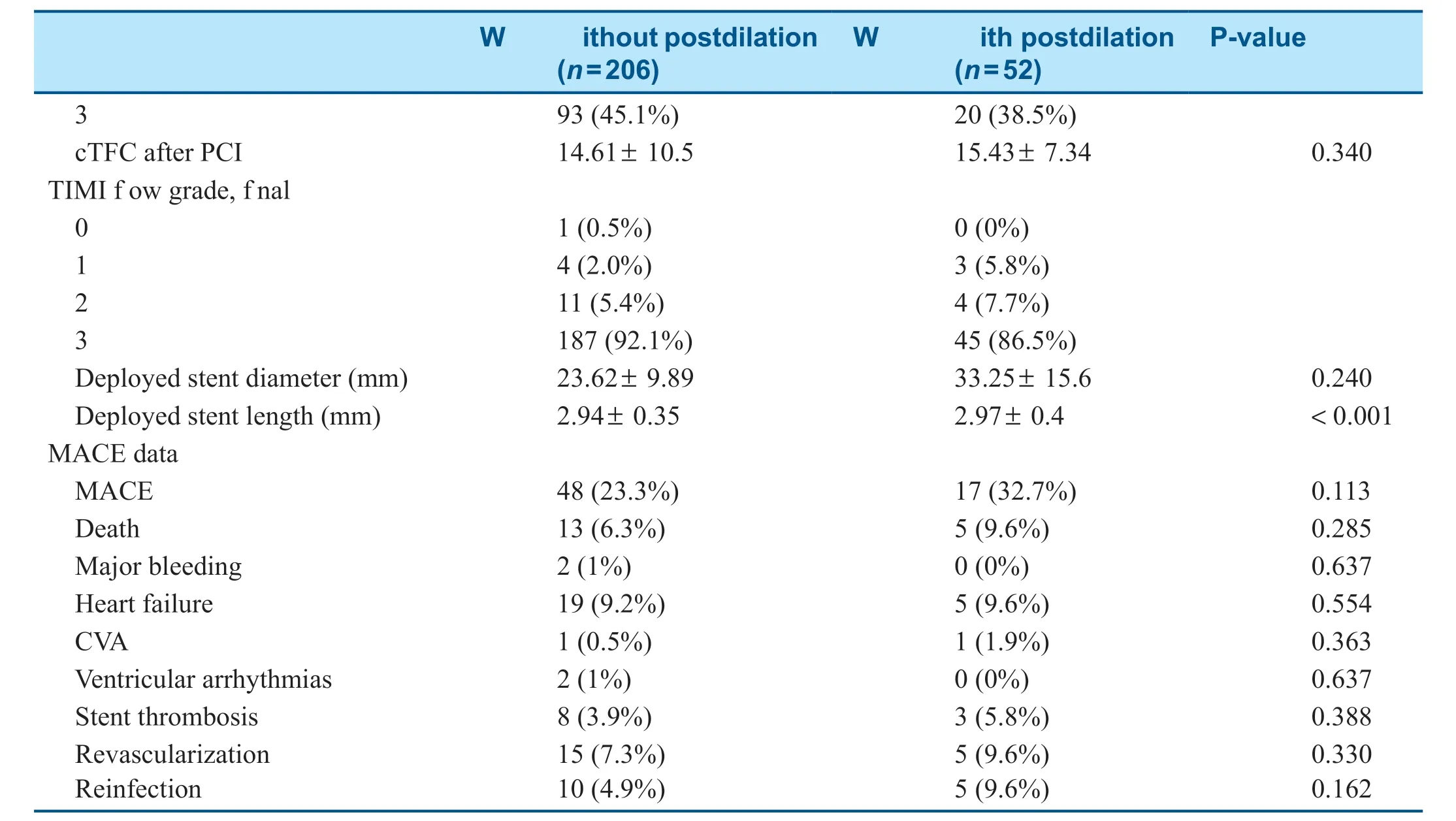
Table1(continued)
There is overwhelming evidence that stent underexpansion is one of the major causes of stent thrombosis [19].The underlying factors that can be associated with stent underexpansion include the techniques used during stent implantation,coronary vasospasm,and lesion characteristics [20].Patients with ACS are particularly susceptible to coronary vasospasm because of increased local inf ammation,and thus stent deployment without use of intracoronary nitrate infusion is traditionally thought to increase stent underexpansion.In addition,the operator ’ s own experience can also impact the development or prevention of stent underexpansion.There are several strategies to reduce the risk of stent under -expansion,including determining the optimal stent length and size,dilation before stent deployment,and inf ation of the stent balloon with maximal pressure.Incomplete stent apposition (ISA) is another important factor for optimal stent implantation,and is classif ed as early and late.Procedural factors are primarily responsible for early ISA,while degenerations in the lesion and stent are responsible for late ISA.The incidence of ISA was found to be as low as 4% and as high as 20% in studies conducted with intravascular ultrasonography [21].The discrepant results were considered to be due to dif ferent stent deployment techniques,distinct stent structures,and different clinical conditions [22].Adverse eventsassociated with ISA were milder than those associated with incomplete stent expansion,and the risk of stent thrombosis was lower [20].In the TAXUS study,the incidence of MACE was not increased in patients with acute ISA during 12-24 months of follow-up [23].
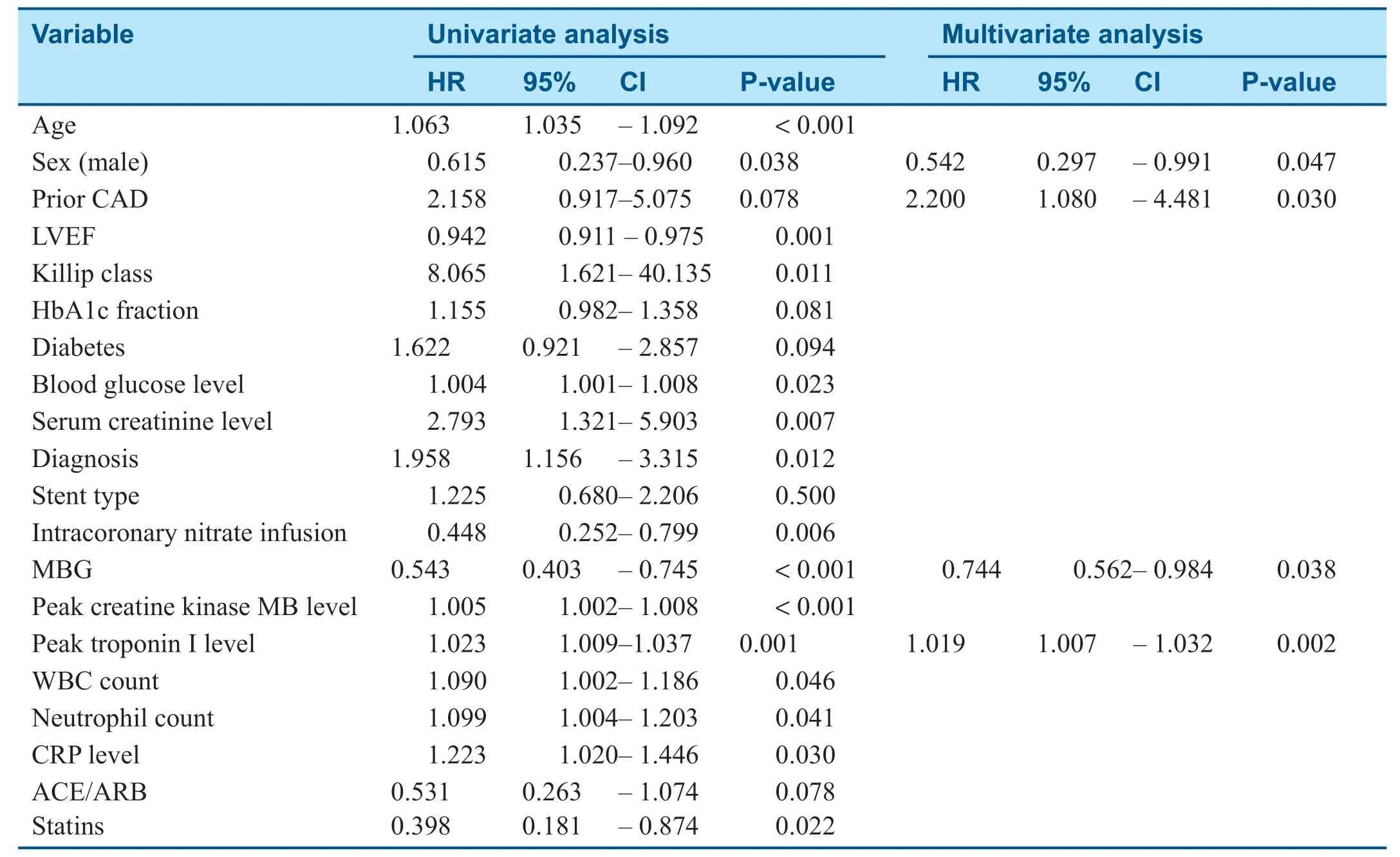
Table2 Independent Predictors of Major Adverse Cardiovascular Events.
Despite favorable outcomes of postdilation with regard to stent malapposition,the same is not applicable to clinical outcomes.Moreover,adverse cardiovascular outcomes were reported as were favorable outcomes with postdilation.In the SIRUS study,stent restenosis was signif cantly higher at the edges of the stent in patients to whom postdilation had been performed [24].Similarly,it was shown that postdilation increased neointimal hyperplasia and subsequent restenosis in studies conducted in both animals and humans [25].However,these data should be interpreted with caution as postdilation was most commonly used in long and calcif c lesions,which could neutralize potential favorable outcomes.
A possible explanation for the controversial results regarding the ef fect of postdilation on cardiovascular outcomes is the lack of the standardization of the technique and of patient selection.When (in which case) and how (at what pressure) to perform postdilation is decided arbitrar -ily by operators in accordance with their clinical experiences.Performing unnecessary and/or high-pressure postdilation causes adverse outcomes.On the other hand,withholding postdilation when deemed necessary could also cause adverse events.Further research is needed to define in which patients and for which lesions postdilation is needed and at what pressures noncompliant balloons should be inf ated.In the present study,the current coronary lesion classif cation was used but it fell short for guidance to identify patients who would benef t most from postdilation.Moreover,it is reasonable to suggest not performing postdilation because ofilack of standardization of the technique and of patient/lesion selection and lack of clinical evidence.
Limitations
The present study was a nonrandomized,singlecenter study with a limited number of patients.
Conclusion
In patients who were treated by PCI for ACS,performing postdilation did not predict final TIMI flow grade,cTFC,MBG,or MACE.
Confl icts of interest
The authors declare that they have no conf icts of interest.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Frailty and Anticoagulant Therapy in Patients Aged 65 Years or Older with Atrial Fibrillation
- The Temporal Relation between Cardiomyopathy and LBBB and Response to Cardiac Resynchronization Therapy:Case Series and Literature Review
- A Giant Right Atrial Myxoma with Blood Supply from the Left and Right Coronary Arteries:Once in a Blue Moon
- Does Coronary Microvascular Spasm Exist? Objective Evidence from lntracoronary Doppler Flow Measurements During Acetylcholine Testing
