Can epigenetic and inflammatory biomarkers identify clinically aggressive prostate cancer?
2020-03-21PedroBargSantosHitendraPatelRuiHenriqueAnalix
Pedro Bargão Santos, Hitendra Patel, Rui Henrique, Ana Félix
Abstract Prostate cancer (PCa) is a highly prevalent malignancy and constitutes a major cause of cancer-related morbidity and mortality. It emerges through the acquisition of genetic and epigenetic alterations. Epigenetic modifications include DNA methylation, histone modifications and microRNA deregulation. These generate heritable transformations in the expression of genes but do not change the DNA sequence. Alterations in DNA methylation (hypo and hypermethylation) are the most characterized in PCa. They lead to genomic instability and inadequate gene expression. Major and minor-specific modifications in chromatin recasting are involved in PCa, with signs suggesting a dysfunction of enzymes modified by histones. MicroRNA deregulation also contributes to the initiation of PCa, including involvement in androgen receptor signalization and apoptosis. The influence of inflammation on prostate tumor carcinogenesis is currently much better known. Recent discoveries about microbial species resident in the urinary tract suggest that these are the initiators of chronic inflammation, promoting prostate inflammatory atrophy and eventually leading to PCa. Complete characterization of the relationship between the urinary microbiome and prostatic chronic inflammation will be crucial to develop plans for the prevention of PCa. The prevalent nature of epigenetic and inflammatory alterations may provide potential biomarkers for PCa diagnosis,treatment decisions, evaluation of prognosis and posttreatment surveillance.
Key words: Prostate cancer; Epigenetics; DNA methylation; Histone modifications;MicroRNAs; Inflammation; Initiation and progression; Prognosis
INTRODUCTION
Prostate cancer (PCa) is the most prevalent noncutaneous malignancy in men in the western world, and it is the second cause of male cancer-related deaths[1]. It is a major cause of cancer-related morbidity and mortality. The prostate gland is composed of four zones: Central, fibromuscular, transitional and peripheral zone. Although the epithelium of the prostate also harbors androgen-independent basal cells and neuroendocrine cells, 95% of PCa are adenocarcinomas; most originate in the peripheral zone and are characterized by multifocality, as well as morphological and molecular heterogeneity[2,3].
Is prostate specific antigen replaceable?
The best biomarker for assessing PCa recurrence remains the prostate specific antigen(PSA) test, and it has been partly responsible for the higher awareness of PCa. In the majority of screening studies, the conventional cut-off for abnormal PSA level is 4.0 ng/mL. PSA performance is systematically reviewed in the literature by the American Cancer Society[4]. In a grouped analysis and with PSA levels of cut-off of 4.0 ng/mL,the sensitivity for detecting any PCa or Gleason ≥ 8 was 21% and 51%, respectively.The specificity was 91%. With PSA levels of 3.0 ng/mL, the sensitivity increased to 32% and 68%, respectively, and the specificity was 85%. In men with symptomatic benign prostatic hyperplasia, there is a weak discriminatory capability from PSA.Therefore, screening for PCa using serum PSA is much debated, and, at best, the survival benefit is marginal[5,6]. Based on established prognostic risk factors (PSA,TNM and Gleason score)[7,8], PCa patients are stratified into low, intermediate, high or very high-risk categories[9]. Low-risk patients are increasingly being offered active surveillance with a curative option in case of progression, while intermediate, highrisk and very high-risk patients are generally offered curative-intent intervention.However, there is a significant shortcoming of the present prognostication, as some low-risk patients progress rapidly, while many of the higher risk patients will not develop symptomatic disease or die from PCa if left untreated. Hence, there is a need for improved prognostic assessment of PCa to better identify patients who do not need radical treatment, sparing them from side effects (incontinence, impotence,lymphocele and other), and those that should receive more intensive treatment[9-11].Although there has been extensive research on prognostic markers, only a few are used routinely: PSA, Gleason score and TNM status. PSA velocity or doubling time is currently emerging as strong predictor of PCa death[12]. Several novel tumor biomarkers have been investigated, but recent reviews criticize the poor quality/statistical power and heterogeneity of many of those studies. Unfortunately,this renders many of the results inconclusive[13,14]. Short follow-up times (often < 5 years) make long-term prediction for clinically useful endpoints unpredictable[10,15].The low cost and noninvasiveness of PSA are difficult to replace. The ideal alternative would be a set of diagnostic and prognostic biomarkers, including PSA, that could detect various analytes. The treatment strategy should be individualized and performed early, taking into account the information from the test. Tissue samples as a biomaterial are far from ideal due to the significant sampling error (limited to portions of the gland) and its highly invasive approach. The ideal PCa biomarkers should not be invasive, and instead collected from blood or urine, for example, and have a strong and reproducible methodology[16]. However, tissue samples might offer a base for initial biomarker investigation that might be subsequently validated in other types of clinical samples[17,18].
Epigenetic balancing: A short overview
Transformations of proteins associated with DNA or transformations of DNA itself that occur during cell division, different from the habitual sequence of DNA and that will be expressed genetically are termed epigenetics[19]. There are three primary mechanisms of epigenetics: MicroRNA (miRNA) regulation, chromatin remodeling and methylation of DNA.
Methylation of DNA
This mechanism is involved in carcinogenesis at local and global levels because it is essential in the control of innumerable cellular events[20,21]. The alteration and extent of epigenetics are responsible for these cellular events. Insufficient gene silencing is associated with DNA hypermethylation, while genetic instability and activation of oncogenes is induced by DNA hypomethylation[20,22].
Chromatin remodeling and histone modifications
The nucleosome is the fundamental unit of the nuclear DNA, and chromatin is the higher order of organization. DNA comprising 147 base pairs is involved, forming a frame, with the protein core and its eight histones[23,24]. Histones are implicated in the control of DNA replication, repair and transcription. They are functional biomolecules that provide sustention to DNA[23,25,26]. In healthy cells, modifications of histones are involved in embryonic stem cell growth and specialization, deactivation of chromosome X and genomic imprinting[23,27]. In neoplastic cells, alterations in DNA methylation and modifications of histones happen in a large percentage of the genome[20,21,28]. Important marks of human cancer are, for instance, hypomethylation of DNA in repetitive sequences, such as decreased lysine 20 trimethylation (H4K20me3)and decreased lysine 16 acetylation (H4K16ac) of H4[29]. Another example is hypermethylation of DNA in silenced genes. Here, we can see association of loss of acetylation of histone 3 (H3ac), methylation of lysines 9 and 27 of histone 3 (H3K9me and H3K27me) and monomethylation of H3K4me[20,30].
Curiously, identical inhibitory histone signs were found in some specific genes with tumor-suppressor actions that are not stopped by DNA methylation[29].Therefore, cancer growth and progression have been linked to modifications in the expression of decisive histone regulating enzymes (HDMs, HMTs, HDACs and HATs)[20,21,23,24].
Micro RNAs
MiRNA are a class of small, noncoding RNA, usually an extension of 18 to 25 nucleotides. The synthesis (pri-miR) and the processing steps (pre-miR) occur in the nucleus. After export to the cytoplasm, mature miR ligate to their corresponding mRNA sequences and change their expression via an RNA-induced silencing complex[31-33]. Every miRNA generally modulates many mRNAs, and mRNAs could be targeted by many miRNAs[34]. MiRNAs control and regulate approximately 30 percent of human genes. This process occurs in a specific tissue and under temporal circumstances[31]. The importance of miRNAs in malignance is dependent upon the particular target genes[31,32]. In terms of programming genes, miRNA expression is changed because of gene mutation, deletion, amplification, abnormalities of chromosomes, alterations in transcription factors, and epigenetic mechanisms[31,32,35].MiRNAs, curiously, can target the posttranscriptional command of crucial enzyme modifiers of chromatin, and therefore are also involved in chromatin structure control. Additionally, miRNAs can establish a ligation with the principal epigenetic routes, including the usual goals for epigenetic regulation via methylation of DNA or modifications of chromatin of promoters[31,32].
Inflammatory biomarkers
One of the presumed risk factors for PCa evolution is chronic inflammation. The mechanism appears to be the creation of lesions that are the genesis of tumor initiation and progression[3,36,37]. Chronic inflammation has been appointed as an enabling characteristic of human cancer growth[38]. Prostate carcinogenesis allegedly drives from epigenetic modifications or mutagenesis induced by reactive oxygen species via oxidative stress[39,40]. Infection of the prostatic gland includes the presence of an inflammatory stromal microenvironment that permits the exposure to pathogenic organisms described by the urinary microbiome[41-47]. Once started,prostatic epithelial barrier disruption and inflammation could produce a feed-forward mechanism resulting in a chronic and persistent inflammatory condition[4,48,49]. Thus,prevention strategies for PCa could clarify the connection between the urinary microbiome and chronic inflammation of prostate.
STUDY ANALYSIS
PubMed was the source of publications on PCa epigenetics and inflammatory pathways. Keywords used were PCa, histone modifications, DNA methylation,miRNAs and inflammation. The search was done on December 29, 2018, and only papers in English were used. A total of 86 original reports were selected.
Methylation of DNA
Irshad et al[50]have performed a search for biomarkers that might discriminate between clinically indolent and clinically aggressive PCa. In 2013, they identified a 19-gene signature enriched in indolent PCa using a gene set enrichment analysis, and classified this signature with a decision tree learning model. They were able to identify 3 genes-CDKN1A, PMP22 and FGFR1 - that together and with accuracy predict the evolution of PCa with low grade Gleason scores. Moreover, in prostate biopsy samples, it was possible to differentiate the prognosis at 10 years of low Gleason scores (Gleason 6) through the expression of proteins from this panel of 3 genes.
Histone modifications and chromatin remodeling
The available data on PCa diagnosis implicated by miRNAs and histone modifications are growing. Levels of H4Ac, H3Ac, H3K4, H3K9me3, H3K9me2, and H3K4me1 are considerably reduced in PCa compared with healthy tissue. With almost over 90%specificity and almost 80% sensitivity, H3K9me2 and H3Ac could differentiate between neoplastic and nonneoplastic tissue[51].
MicroRNA deregulation
Recently, two-gene promoter methylation panels-MiR-193b and miR-34b/c-were studied in 209 patients with the objective of perceive their diagnostic and prognostic capabilities[52]. Tissue biopsies and urine from PCa and control patients were used[52,53].In another report from the same study group involving 336 patients, Torres-Ferreira et al[53]showed that methylation of miR-129-2 or miR-34b/c promoters defined clinically aggressive neoplasms, and MiR-193b promoter methylation correctly detected PCa in urine sediments. This panel may be a clinically helpful instrument for risk stratification of aggressiveness in urine and tissue biopsies.
The results of Moreira-Barbosa et al[52]were consistent with other research that quantitatively analyzed the methylation of RASSF1A, GSTP1 and APC in 350 samples of needle core biopsies. The negative predictive value was between 88%-100%. These findings corroborate tests evolving methylation as very important instruments for the decision of rebiopsy[54-56].
Long non-coding RNAs are nowadays arousing great interest. They have pertinent characteristics: They are tissue and cancer-specific, extremely abundant[57]and detectable in urine and blood[58,59]. In the diagnosis scenario, PCA3, FR0348383 and MALAT1, may counsel avoidance of biopsies without missing high risk tumors[60,61]. In the prognosis setting, SChLAP1, PCAT-14 and PCAT-18 seem to be the most promising. SChLAP1, detected in urine, showed significance in predicting biochemical relapse, clinical progression and PCa specific mortality[58,62]. PCAT-14 was associated with worse overall and metastasis free survival[63]and PCAT-18, detected in plasma, seems to be highly specific for metastatic castration resistant PCa in comparison with localized PCa[64].
Current molecular taxonomy of primary PCa
Primary PCa heterogeneity is notorious in clinical course as well as in the variety of molecular characteristics. The Cancer Genome Atlas Research Network, in 2015,presented a molecular analysis of 333 primary PCa[65]. The outcomes showed 74% of the study tumors were present in one of the seven subgroups of gene fusions (FL1,ETV1/4 and ERG) or mutations (IDH1, FOXA1 and SPOP). Remarkable heterogeneity was observed in epigenetic profiles that included an IDH1-mutant subcategory.Tumors having FOXA1 and SPOP mutations had the highest levels of androgen receptor (AR) induced transcription. Furthermore, 25% of PCa showed a supposed injury in signaling pathways of MAPK or PI3K. Inactivation of DNA repair genes occurred in 19%[65]. One of the most important pieces of evidence corroborated by this study was the presence of molecular heterogeneity and molecular defects potentially triggered in primary PCa.
Inflammatory biomarkers
Current evidence, described recently by Sfanos et al[66], showed that the urinary tract,instead of being completely sterile, as was thought, contains a large variety of microorganisms. The discovery of DNA from bacteria of a distinct flora questioned the principle of sterile urine[67]. Another discovery implicates chronic prostatic inflammation as the main etiological factor of what was called proliferative inflammatory atrophy (PIA). PIA was described as composed of cells highly sensitive to genomic alterations that could be transformed into prostatic intraepithelial neoplasia (PIN) and PCa[3,68,69]. The same authors make an association between these two facts. They consider that the microorganisms resident in the urinary tract can be the precursors of prostatic chronic inflammation, thus developing PIA and PCa(Figure 1). The precise mechanisms of this transformation are not known. Direct DNA damage and genetic instability caused by reactive oxygen species (ROS) and reactive nitrogen species liberated by immune cells is one theory[3,70]. Another mechanism is related to the recruitment of epigenetic machinery to sites of DNA damage provoked by oxidative stress, which includes DNA methyltransferases, chromatin remodelers and repressor complexes[39,40]. This mechanism could be an explanation for the silencing of transcription and vast methylation of aberrant DNA in promoters of genes that occur over PCa progression and metastasis[71,72]. The model, studied in vitro,demonstrated that prostate epithelial cells, in association with androgen receptor (AR)signaling, develop TMPRSS2-ERG gene fusions when exposed to oxidative stress,contributing to PCa formation[73]. The precise mechanisms by which this occurs are not entirely known, but the researchers proposed that formation of ROS and DNA breaks results from signaling of epithelial cells by inflammatory cytokines, such as tumor necrosis factor (TNF)[73].
Another theory involves transcriptional function induced by AR that requires DNA topoisomerase 2β (TOP2B) and ROS. TOP2B, after binding AR, is recruited to certain loci, such as TMPRSS2, and then can create a break in double-strand DNA[74].
In this model, TOP2B may get stuck on the DNA as a consequence of an increase of ROS, generating breaks in double-strand DNA. This can lead to genomic rearrangements during PCa initiation[74,75]. Prostate carcinogenesis may also be determined by inflammation through the formation of intermediate cells that are suspected targets for this process, specifically enriched in areas of PIA[77]. These kinds of lesions are normally seen in direct relation to PIN and occasionally adenocarcinoma[76,77]. Furthermore, hypermethylation of the CpG islands sometimes occurs in PIA (less than 10%). This phenomenon arises in epithelial cells and at the GSTP1 promoter. It is commonly seen in PIN and carcinoma, but not in normal epithelium[78].
In 2016[79], a study with dissociated cells isolated from benign human prostate tissue concluded that a large number of the epithelial cells of the luminal compartment of PIA expressed low levels of CD38. In contrast, mature luminal cells expressed high levels of CD38. The first cells (CD38low) were termed inflammation-associated luminal cells (IALs). They showed, compared with CD38hi, an increase in the signaling of nuclear factor-κB (NFκB) and a decrease in the signaling of AR (measured by decreased expression of AR-target genes KLK2, KLK3, KLK4, MSMB, ACPP and FKBP5). Moreover, IALs improved GSTP1 expression along with anti-apoptotic factor Bcl-2 and were positive for CK8 and CK5 but negative for keratin 14 (a basal cell cytokeratin) and tumor protein[79]. These facts also favor the composition of IALs by intermediate cells.
In an in vivo tissue trial (rodent models of prostatitis), IALs, compared with CD38hi cells, had a greater ability to create lesions initiated by oncogenes (e.g., AR, AKT,MYC) and with similarity to human PCa[80]. These studies support the idea that inflammation induces the formation of progenitor-like target cells (intermediate cells)that are susceptible to tumorigenesis.
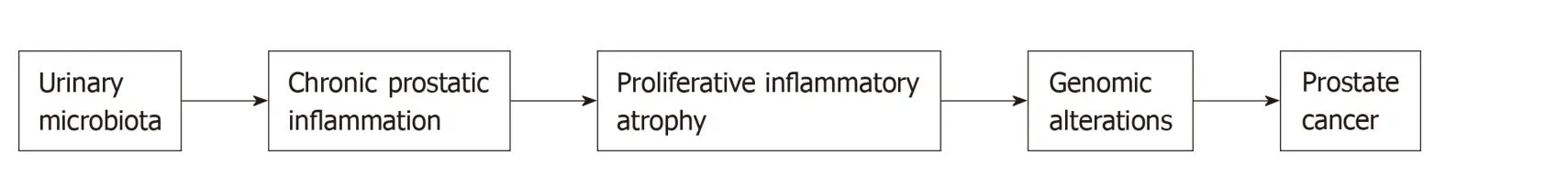
Figure 1 Hypothetical theory of preinitiation and initiation of prostate cancer. Two important recent discoveries were the presence of resident microbial species in the urinary tract and their role in the initiation of chronic inflammation, proliferative inflammatory atrophy and development of Prostate cancer (PCa). Facts that may explain the higher prevalence of PCa in western countries include elevated inflammation due to metabolic syndrome and associated comorbidities. It is essential to completely characterize the link between these facts to allow the development of strategies for PCa prevention. PCa: Prostate cancer.
In 2013, Fang et al[81]induced prostate tumorigenesis by coculturing immortalized prostate epithelial cells (“RWPE-1 and benign prostatic hyperplasia -1 cells-the nonneoplastic, immortalized human prostatic epithelial cell lines and THP-1 cells-the human acute monocytic leukemia cell line”) with macrophages and without adding any carcinogens. They showed that this phenomenon included the “signaling change of activation of macrophage androgen receptor (AR)-inflammatory chemokine CCL4-STAT3”,along with the “epithelial-to-mesenchymal transition” and the downregulation of p53/PTEN tumor suppressors. Their outcomes highlight the importance of infiltrating macrophages and inflammatory cytokines in prostate cancerogenesis and identified the AR-CCL4-STAT3 axis as determinant governors during prostate tumour initiation.Gueron et al[82], in 2012, hypothesized that the molecular signaling triggered by inflammatory mediators may develop in PCa progression. Thus, chronic inflammation may represent an important therapeutic target in advanced PCa.According to those authors, the most relevant chemokine receptors in PCa dissemination are CXCR4, CXCR7 and CXCR6. On the other hand, the expression of CXCL8 (IL-8), one of the best-characterized members of the chemokine family,correlates with increased angiogenesis, tumorigenicity and lymph node metastasis in vivo. Moreover, IL-6, one of the most relevant inflammatory mediators clearly implicated in PCa, has been associated with proliferation, angiogenesis, apoptosis and the modulation of tumor growth and differentiation in many cancers. High levels of IL-6 and its soluble receptor in circulating plasma have been documented in PCa patients, correlating with more advanced disease stage, therapy resistance, and poor prognosis, and may be predictive of recurrence after treatment of localized PCa. Arya et al[83]also demonstrated that metastases express functional CXCR4 receptor and CXCL12 ligand enhances the migratory capabilities of PCa cells. These results propose that the CXCL12:CXCR4 pathway may influence PCa during metastasis.
Another important issue is the control mechanisms that underlie the development of PCa and the resistance to androgen-deprivation treatment. Androgen deprivation therapy has become one of the major therapies for patients at distinct stages of the disease. Nonetheless, a significant fraction of patients progress to androgenindependence. There is important positive and negative interaction between signalization of steroid hormones, including androgen receptors, and inflammatory signalization done by NF-kB and other transcription elements[84,85]. High NF-κB expression is associated with CXCR4 expression, and they are coexpressed in approximately one-third of patients with organ-confined PCa[86]. Larger studies are required to accurately determine the frequency of coexpression and prognostic utility of NF-κB and CXCR4 alone and in combination.
CONCLUSION
Epigenetic modifications are a common feature of PCa and play an important role in prostate carcinogenesis as well as in disease progression. Even though aberrant DNA methylation is the best-studied cancer-related epigenetic alteration in PCa, the study of alterations in chromatin remodeling and miRNA regulation constitute a growing research field that will provide an overall view of the PCa epigenome as well as of the interaction between epigenetic and genetic mechanism involved in prostate carcinogenesis. Two important recent discoveries were made: The presence of resident microbial species in the urinary tract and their role in the initiation of chronic inflammation, PIA and development of PCa. Facts that may explain the higher prevalence of PCa in the western countries include elevated inflammation due to metabolic syndrome and associated comorbidities. It is essential to completely characterize the link between these facts - chronic prostatic inflammation and epigenetic alterations - to allow the development of strategies for PCa prevention.
杂志排行
World Journal of Clinical Oncology的其它文章
- Metastatic clear cell renal cell carcinoma in isolated retroperitoneal lymph node without evidence of primary tumor in kidneys: A caes report
- Pituitary carcinoma: Two case reports and review of literature
- Pancreatic adenocarcinoma with early esophageal metastasis:A case report and review of literature
- Abdominal metastases of primary extremity soft tissue sarcoma:A systematic review
- Objective response rate assessment in oncology:Current situation and future expectations