Clinical utility of treatment method conversion during single-session endoscopic ultrasound-guided biliary drainage
2020-03-13KosukeMinagaMamoruTakenakaKentaroYamaoKenKamataShunsukeOmotoAtsushiNakaiTomohiroYamazakiAyanaOkamotoReiIshikawaTomoeYoshikawaYasutakaChibaTomohiroWatanabeMasatoshiKudo
Kosuke Minaga, Mamoru Takenaka, Kentaro Yamao, Ken Kamata, Shunsuke Omoto, Atsushi Nakai,Tomohiro Yamazaki, Ayana Okamoto, Rei Ishikawa, Tomoe Yoshikawa, Yasutaka Chiba, Tomohiro Watanabe,Masatoshi Kudo
Abstract BACKGROUND Although several techniques for endoscopic ultrasound-guided biliary drainage(EUS-BD) are available at present, an optimal treatment algorithm of EUS-BD has not yet been established.AIM To evaluate the clinical utility of treatment method conversion during single endoscopic sessions for difficult cases in initially planned EUS-BD.METHODS This was a single-center retrospective analysis using a prospectively accumulated database. Patients with biliary obstruction undergoing EUS-BD between May 2008 and April 2016 were included. The primary outcome was to evaluate the improvement in EUS-BD success rates by converting the treatment methods during a single endoscopic session. Secondary outcomes were clarification of the factors leading to the conversion from the initial EUS-BD and the assessment of efficacy and safety of the conversion as judged by technical success, clinical success, and adverse events (AEs).RESULTS A total of 208 patients underwent EUS-BD during the study period. For 18.8%(39/208) of the patients, the treatment methods were converted to another EUSBD technique from the initial plan. Biliary obstruction was caused by pancreatobiliary malignancies, other malignant lesions, biliary stones, and other benign lesions in 22, 11, 4, and 2 patients, respectively. The reasons for the difficulty with the initial EUS-BD were classified into the following 3 procedures:Target puncture (n = 13), guidewire manipulation (n = 18), and puncture tract dilation (n = 8). Technical success was achieved in 97.4% (38/39) of the cases and clinical success was achieved in 89.5% of patients (34/38). AEs occurred in 10.3%of patients, including bile leakage (n = 2), bleeding (n = 1), and cholecystitis (n =1). The puncture target and drainage technique were altered in subsequent EUSBD procedures in 25 and 14 patients, respectively. The final technical success rate with 95%CI for all 208 cases was 97.1% (95%CI: 93.8%-98.9%), while that of the initially planned EUS-BD was 78.8% (95%CI: 72.6%-84.2%).CONCLUSION Among multi-step procedures in EUS-BD, guidewire manipulation appeared to be the most technically challenging. When initially planned EUS-BD is technically difficult, treatment method conversion in a single endoscopic session may result in successful EUS-BD without leading to severe AEs.
Key words: Endoscopic ultrasound; Endoscopic ultrasound-guided biliary drainage;Interventional endoscopic ultrasound; Biliary drainage; Biliary obstruction
INTRODUCTION
Transpapillary biliary drainage under endoscopic retrograde cholangiopancreatography (ERCP) is a standard treatment for biliary obstruction. However,endoscopists encounter technical difficulties with biliary drainage under ERCP guidance in approximately 5%-10% of cases[1-3]. Even though percutaneous transhepatic biliary drainage (PTBD) has been established as an alternative for therapeutic relief of biliary obstruction in such situations, its morbidity and mortality rates have been reported to be high[4-6]. For overcoming the problems associated with PTBD, a novel alternative endoscopic procedure termed endoscopic ultrasoundguided biliary drainage (EUS-BD) was developed in 2001 for patients with unsuccessful conventional ERCP[7]. Over the past two decades, EUS-BD has attracted significant attention and the number of patients who have received this procedure after unsuccessful ERCP has been increasing.
At present, several EUS-BD techniques, including various approach routes and drainage methods, have been developed[8-11]. Regarding the approach routes, two major routes are used: The transgastric intrahepatic approach and the transduodenal extrahepatic approach. Biliary drainage can usually be achieved by one of three drainage methods: Transmural stenting, antegrade stenting, and the rendezvous technique (EUS-RV)[8-11]. Endoscopists select one or two safe techniques with a high probability of success among the many EUS-BD techniques. Although patient anatomy, underlying disease, location of the biliary stricture, and the diameter of the intrahepatic bile duct are regarded as important factors for the selection of the approach routes and drainage methods[9,12], the optimal treatment strategy for EUS-BD has not yet been established. EUS-BD comprises multiple steps, including target puncture, guidewire manipulation, puncture tract dilation, and stent placement.Among these steps, technical difficulties can arise in each approach route and drainage method. However, the technically critical steps have not yet been clarified.Furthermore, no consensus has been reached regarding troubleshooting when the initial EUS-BD technique appears to be challenging. Thus, both the technical issues and treatment algorithms have been poorly defined in EUS-BD, despite overall technical success rates having been reported to be 90%-96%[13-17]. At our institution, we have attempted to change the puncture target or drainage method in a single endoscopic session upon encountering difficulty with accomplishing the initial plan.In this study, we have analyzed the outcomes of conversion during EUS-BD and identified technically difficult steps in each EUS-BD technique. We provide data regarding the utility and safety of treatment method conversion from the initially planned EUS-BD during a single endoscopic session.
MATERIALS AND METHODS
Patients
Patients who underwent EUS-BD between May 2008 and April 2016 were identified from the prospectively accumulated database of the Kindai University Hospital(Osaka-Sayama, Japan). Among these, cases with conversion of treatment methods from the initial EUS-BD plan in the same endoscopic session were extracted by reviewing electronic medical records and endoscopic reports. The protocol employed to perform this study was approved by the Institutional Review Board of Kindai University Faculty of Medicine (approval number: 28-173). The following data were retrieved from the patients’ medical records: Patient characteristics (age, sex,performance status, underlying disease, blood tests), reasons for EUS-BD, reasons for changing the treatment methods, and details of the endoscopic procedures, including technical and clinical success, procedure times, and adverse events (AEs). Patients with attempted EUS-BD were defined as those who received bile duct punctures under EUS at least once. Patients who discontinued the study after observation with EUS were excluded from this study. Patients enrolled in other clinical trials were also excluded. All patients provided written informed consent before undergoing the endoscopic procedures.
Endoscopic procedures of EUS-BD
All EUS-BD procedures were performed by endoscopists trained and experienced in both ERCP and EUS procedures. Patients were placed in the prone position with moderate sedation using intravenous propofol. A linear-array echoendoscope (GFUCT240 or 260; Olympus Medical Systems, Tokyo, Japan) was used to achieve initial biliary access from the gastrointestinal lumen. As described above, the drainage methods for EUS-BD are divided into the following: Transmural stenting, antegrade stenting, and EUS-RV. Among those three, EUS-BD with transmural stenting can be performed via two main access routes: EUS-guided choledochoduodenostomy (EUSCDS) and EUS-guided hepaticogastrostomy (EUS-HGS). In EUS-CDS, a dilated extrahepatic bile duct was visualized from the duodenal bulb and punctured using a 19-gauge aspiration needle. After cholangiography, a 0.025-inch guidewire(VisiGlide2; Olympus Medical Systems, Revowave; Piolax, Yokohama, Japan) was placed and advanced into the biliary tree, and then a tapered catheter was inserted(StarTip V; Olympus Medical Systems, ERCP-Catheter Filiform; MTW Endoskopie,Düsseldorf, Germany). The puncture tract was dilated using a bougie dilator(Soehendra Biliary Dilation Catheter; Cook Endoscopy, Winston Salem, NC, United States) or a 4-mm balloon dilator (Hurricane RX; Boston Scientific Corporation,Natick, MA, United States) over the guidewire. Finally, a covered metal stent (8 mm in diameter, 6 or 8 cm in length) or a double-pigtail plastic stent (7 Fr in diameter, > 6 cm in length) was deployed between the extrahepatic bile duct and the duodenal bulb. In EUS-HGS, the dilated left intrahepatic bile duct was punctured from the stomach using a 19-gauge needle. After inserting the guidewire into the biliary tree and dilating the puncture site in the same manner as in EUS-CDS, a covered metal stent (8 mm in diameter, 10 or 12 mm in length) or a double-pigtail plastic stent (7 Fr in diameter, > 10 cm in length) was deployed between the left intrahepatic bile duct and the stomach.
In antegrade stenting, as with EUS-HGS, the left intrahepatic bile duct was punctured from the gastrointestinal lumen. A 0.025-inch guidewire was inserted deep into the biliary tree and was manipulated into the gastrointestinal lumen across the papilla or anastomosis site. To prevent bile leakage, dilation of the puncture site was minimized with the ERCP catheter alone, given the puncture tract was temporarily created and unsealed after stent placement. An uncovered metal stent with a thin delivery system (8 or 10 mm in diameter, 6 or 8 cm in length) or a 7-Fr straight plastic stent was deployed to cover the biliary stricture.
In EUS-RV, initial biliary access was achieved from the stomach or duodenum under EUS guidance, then a 0.025-inch guidewire (Revowave, Piolax) was inserted into the biliary tree. The guidewire was manually advanced across the ampulla and was coiled within the duodenum. Then, the needle and the echoendoscope were withdrawn, leaving the guidewire in place. Alongside the guidewire, a duodenoscope(TJF-260V, Olympus Medical Systems) was inserted and the biliary cannulation was performed with an ERCP catheter under the guidance of the EUS-placed guidewire.After access to the bile duct was achieved, transpapillary biliary stenting was performed under conventional ERCP guidance. In the study period, diathermic dilators were not used for puncture tract dilation because their use had been reported to increase AEs[18].
Selection of initial drainage methods
In principle, ERCP has been performed in our institution as a primary biliary drainage technique in cases of biliary obstruction. EUS-BD has been considered when initial ERCP was unsuccessful or reintervention with ERCP was unsuccessful or ineffective.Thus, all EUS-BD procedures have been performed as rescue biliary drainage after failed conventional ERCP. EUS-BD is judged to be contraindicated in the following situations: Eastern Cooperative Oncology Group performance status of 4, bleeding tendency (prothrombin time international normalized ratio > 1.5 or < 50000 platelets),the continuous use of antithrombotic agents, or the presence of massive ascites. The treatment algorithm for initial EUS-BD in our institution is shown in Figure 1. The algorithm was tentatively established, mainly based on patient anatomy, underlying disease, and the location of the biliary stricture as described previously[9,12]. In brief,transmural stenting was selected as an initial EUS-BD procedure when the papilla was endoscopically inaccessible due to an anatomical issue or duodenal stricture.EUS-HGS was used as an initial plan of EUS-BD in cases with hilar biliary obstruction, whereas either EUS-CDS or EUS-HGS was considered the initial plan in distal biliary obstruction with patent duodenal bulb. If the duodenal bulb was inaccessible, EUS-HGS was selected. On the other hand, if the papilla was endoscopically accessible, EUS-RV was considered the first-choice EUS-BD technique in cases with benign or resectable malignant biliary obstruction. In inoperable cases,transmural stenting was indicated as the first choice. As with cases with an inaccessible papilla, the choice of EUS-CDS or EUS-HGS for transmural stenting was based on the site of biliary obstruction. In summary, EUS-RV or transmural stenting with EUS-CDS or EUS-HGS were used as the first-choice drainage method for EUSBD in this study. Antegrade stenting was not chosen as the initial EUS-BD method.
Conversion of treatment methods in EUS-BD
When the initial EUS-BD failed, endoscopists selected alternative EUS treatment methods to achieve successful biliary drainage after careful consideration of several factors. If the initial EUS-RV had failed, EUS-RV via another approach route or transmural stenting (EUS-CDS or EUS-HGS) could be considered as an alternative drainage technique. When the initial EUS-HGS was unsuccessful, antegrade stenting or EUS-CDS was considered as an alternative approach. In cases with distal biliary obstruction, EUS-guided gallbladder drainage (EUS-GBD) was also indicated if the gallbladder was swollen due to biliary obstruction[19]. Thus, there could be multiple conversion techniques as an alternative to EUS-BD, and the endoscopists selected the technique that seemed most appropriate for each case.
Study endpoints and definitions
The primary outcome of the current study was to assess improvements in the technical and clinical success rates of EUS-BD by converting the treatment method during a single endoscopic session. Secondary outcomes assessed reasons for the conversion of the initial EUS-BD and the methods that were altered; and clinical outcomes of the secondary EUS-BD, including technical and clinical success rates,procedure times, and AE rates. Technical success was defined as successful stent deployment at the target site, as confirmed by a combination of endoscopy and fluoroscopy. Clinical success was defined as an improvement in cholangitis or a decrease in serum bilirubin levels either to a normal level or reduced by more than 50% within 2 weeks following EUS-BD. AE severity was classified according to the American Society for Gastrointestinal Endoscopy lexicon[20].

Figure 1 Treatment algorithm for initial endoscopic ultrasound-guided biliary drainage in this study. ERCP:Endoscopic retrograde cholangiopancreatography; EUS-RV: EUS-guided rendezvous technique; EUS-HGS: EUSguided hepaticogastrostomy; EUS-CDS: EUS-guided choledochoduodenostomy.
Statistical analysis
Continuous variables are presented as medians and ranges, and categorial variables as numbers and percentages. The rates of technical and clinical success and AEs are presented with a 95%CI. Statistical analyses were performed using SAS version 9.4 software (SAS Institute Inc., Cary, NC, United States).
RESULTS
Patient characteristics
During the study period, a total of 208 patients underwent EUS-BD as rescue biliary drainage at our institution. As an initial EUS-BD technique, EUS-RV, transmural stenting with EUS-CDS, and EUS-HGS were performed in 43, 52, and 113 patients,respectively. In 18.8% (39/208) of the cases, the initial EUS-BD technique was converted to a different EUS-BD technique. The initial EUS-BD technique used for the patients who required conversion was EUS-RV in 11, EUS-CDS in 12, and EUS-HGS in 16 patients. Demographic and clinical characteristics of this population (n = 39) are shown in Table 1. The median patient age was 74 years (range, 40-89), and 26 were men. Biliary obstructions were caused by pancreatobiliary malignancies, other malignant lesions, biliary stones, and other benign lesions in 22, 11, 4, and 2 patients,respectively. Malignant lesions in locations other than the pancreatobiliary systems included 6 cases of gastric cancer, 4 cases of colon cancer, and 1 case of malignant lymphoma. Two benign lesions other than biliary stones included anastomotic biliary strictures and inflammatory biliary wall thickening.
These 39 cases consisted of 19 (48.7%) with failure of duodenal scope insertion, 5(12.8%) with inability to access the papilla after duodenal stent placement, 11 (28.2%)with failure of biliary deep cannulation or selection, and 4 (10.3%) with surgically altered anatomy (Table 2). The reasons for technical difficulty with the initial EUS-BD techniques are shown in Figure 2. Three major factors causing difficulties with the initial EUS-BD were noted: Failure of target puncture (n = 13, 33.3%), failure of puncture tract dilation (n = 8, 20.5%), and failure of guidewire manipulation (n = 18,46.2%). Thus, the proportion of patients who required conversion was 18.8% of 208 total initial EUS-BD procedures. Moreover, target puncture and guidewire manipulation were identified as critical steps for successful initial EUS-BD.
Treatment method conversion from the initial EUS-BD
We examined final outcomes and causes of failure in patients who required treatment conversion in terms of the initial EUS-BD procedures.
Outcomes of patients with attempted EUS-RV as the initial EUS-BD plan
EUS-RV was attempted as the initial EUS-BD in 43 (20.7%) of 208 patients. The initial EUS-RV was successful in 30 (69.8%) patients. Among the 13 unsuccessful treatments,2 patients were successfully treated with reattempted ERCP without considering analternative EUS-BD. Alternative EUS-BD techniques were performed in the remaining 11 patients. Difficulty with guidewire manipulation led to unsuccessful EUS-RV in all 11 patients. Regarding the alteration of treatment methods, the puncture target was altered in 1 (9.1%) patient, and the drainage technique was changed from RV to transmural stenting in the remaining 10 (90.9%) patients. EUS-RV, EUS-HGS, and EUS-CDS were performed as the EUS-BD conversion technique in 1 (9.1%), 4 (36.4%),and 6 (54.5%) patients, respectively (Figure 3A).

Table 1 Demographic and clinical characteristics of 39 patients who underwent treatment method conversion from the initially planned endoscopic ultrasound-guided biliary drainage
Outcomes of patients with attempted EUS-CDS as the initial EUS-BD plan
Transmural stenting with EUS-CDS was attempted as the initial EUS-BD plan in 52(25.0%) of 208 patients. The initial EUS-CDS was successful in 40 (76.9%) patients. The initial EUS-CDS was converted to another EUS-BD technique in the 12 unsuccessful treatments. Failures in the initial EUS-CDS were caused by difficulty with the puncture target (n = 6, 50%), guidewire manipulation (n = 3, 25%), and puncture tract dilation (n = 3, 25%). The puncture target was changed in all 12 patients in the subsequent EUS-BD procedures, including EUS-HGS (n = 8, 66.7%) and EUS-GBD (n= 4, 33.3%). No changes in the drainage method were noted (Figure 3B).
Outcomes of patients who attempted EUS-HGS as the initial EUS-BD plan
Transmural stenting with EUS-HGS was attempted in 113 (54.3%) of 208 patients. The initial EUS-HGS was successful in 94 (83.2%). Among the 19 unsuccessful treatments,surgical drainage was performed in 1 patient because the stent had migrated into the abdominal cavity during EUS-HGS. In addition, PTBD was immediately performed in 2 patients after failed initial EUS-HGS. For the remaining 16 patients, the initial EUSHGS was changed to an alternative EUS-BD technique. Failures in the initial EUSHGS were caused by difficulty with the target puncture (n = 7, 43.8%), guidewire manipulation (n = 4, 25%), and puncture tract dilation (n = 5, 31.3%). The puncture target was altered in 12 (75%) patients, whereas the drainage method was altered in the remaining 4 (25%). For patients in whom the puncture target was changed, EUSCDS (n = 4), EUS-HGS (n = 4), and EUS-GBD (n = 4) were performed as the alternative EUS-BD technique. In 1 patient, EUS-HGS was attempted via a different biliary branch, but was unsuccessful due to difficulty with the puncture. In this case, PTBD was performed after failed EUS-BD. For 4 patients in whom the drainage method was changed, EUS-RV (n = 2) and antegrade stenting (n = 2) were performed (Figure 3C).
Clinical outcome and impact of alteration from initial EUS-BD methods
Technical success was achieved in 38 (97.4%) of 39 patients who underwent conversion of EUS-BD techniques in a single endoscopic session, and clinical success was verified in 34 (89.5%) of 38 patients. In 1 patient with an unsuccessful alternativeEUS-BD, the initial HGS failed due to difficulty with guidewire manipulation, and an alternative HGS via another biliary branch was also unsuccessful due to difficulty with the target puncture. As previously described, this patient was successfully treated with PTBD.
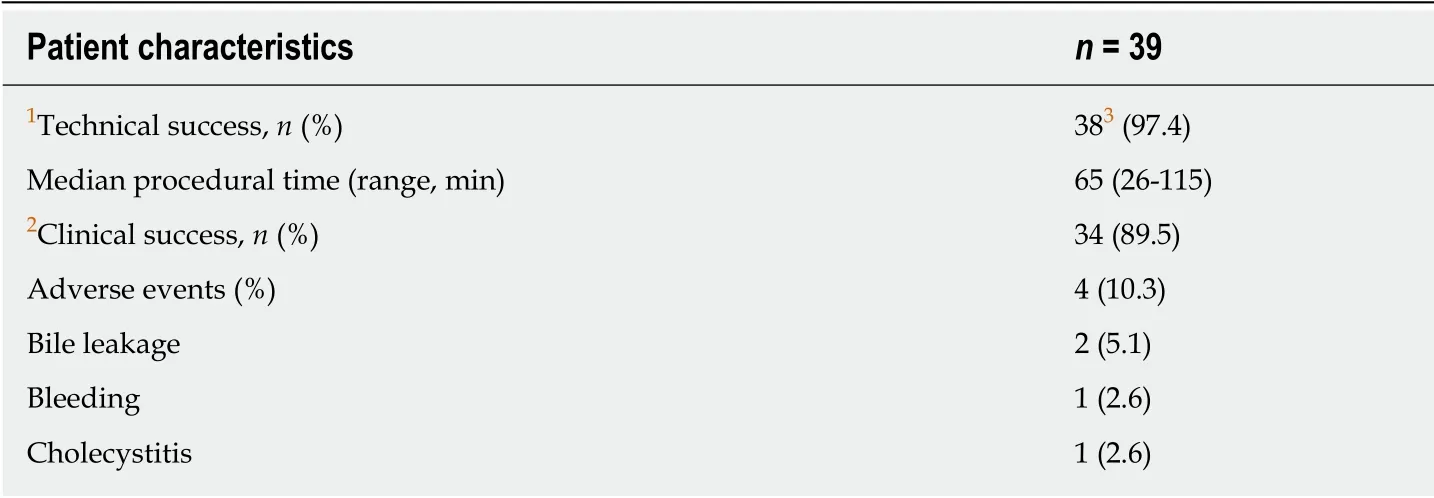
Table 2 Clinical outcomes of patients who underwent treatment method conversion from initially planned endoscopic ultrasound-guided biliary drainage
AEs occurred in 4 (10.3%) of 39 patients. These AEs included bile leakage (n = 2),bleeding (n = 1), and cholecystitis (n = 1), all of which were conservatively managed.The median procedure time was 65 min (range, 26-115 min). The overall technical success rate, including alternative EUS-BD procedures, was 97.1% (202/208, 95%CI:0.938-0.989) though that of the initially planned EUS-BDs was 78.8% (164/208, 95%CI:0.727-0.842). Similarly, the clinical success rate was 74.0% (154/208, 95%CI: 0.675-0.799) for EUS-BD with initial treatment alone, but this increased to 90.4% (188/208,95%CI: 0.855-0.940) when alternative EUS-BD procedures were included. The rate of AEs with the initial EUS-BD was 17.8% (37/208, 95%CI: 0.128-0.237), whereas that of all cases, including those treated with alternative EUS-BD procedures, was 19.7%(41/208, 95%CI: 0.145-0.258).
DISCUSSION
In this study, we retrospectively evaluated the usefulness of treatment method conversion from the initial EUS-BD technique during a single endoscopic session. We found that the conversions contributed to significant improvements in the overall technical and clinical success of EUS-BD, regardless of the initial EUS-BD technique used (EUS-RV, EUS-CDS, or EUS-HGS). Thus, we have found evidence that treatment method conversion immediately after failure of initial EUS-BD can be beneficial for patients in whom ERCP-based biliary drainage is impossible or unsuccessful. In the subgroup analyses based on the type of initial EUS-BD technique, we found that the success of EUS-BD depended upon the management of the target puncture, the dilation of puncture tract, and guidewire manipulation. Given the limited data on the conversion methods after initial EUS-BD, our results might be useful not only for establishing the treatment algorithm but also for troubleshooting guidance in EUSBD.
It is generally accepted that patient anatomy, underlying diseases, and location of the biliary stricture are important factors affecting the selection of the initial EUS-BD technique. Along these lines, the treatment algorithm for EUS-BD in our institution(Figure 1) is based on the accessibility of the papilla by endoscopy, the presence or absence of malignant diseases, and the location of biliary strictures (distal or hilar).According to this algorithm, EUS-HGS was selected as the initial EUS-BD in more than half of the cases, and EUS-RV was the least often chosen. The technical success rate of the initial EUS-BD was highest for EUS-HGS at 83.2%, followed by EUS-CDS at 76.9%, and lowest in EUS-RV at 69.8%. However, the ideal method as a first-choice technique among a wide variety of EUS-BD techniques is under debate. Thus, we emphasize that future studies are required to verify the safety and efficacy of our tentative algorithm for EUS-BD.

Figure 2 Reasons for difficulties in initial endoscopic ultrasound-guided biliary drainage. CDS:Choledochoduodenostomy; HGS: Hepaticogastrostomy; RV: Rendezvous technique.
Previous reviews focusing on the utility of drainage methods have shown that the technical success rate of EUS-RV was 81%[8,21]lower than that of transmural stenting.Indeed, the success rate of EUS-RV was lower than EUS-HGS and EUS-CDS in this study. EUS-RV is superior to transmural stenting techniques in that it preserves the anatomical integrity of the biliary tracts without creating a permanent anastomosis.On the other hand, EUS-RV procedures are complicated, given scope exchange and skillful guidewire manipulation are required. Thus, the lower success rates of EUS-RV can be partially explained by its complicated procedures. In fact, all the 11 unsuccessful treatments of initial EUS-RV had difficulty with guidewire manipulation in passing through the biliary stricture or the papilla. As shown in Figure 3A, most of these cases were rescued by converting to transmural stenting without changing the access route. A recent study has shown that the extrahepatic approach from the second portion of the duodenum, called the D2 approach, had the highest technical success rate because this route facilitates guidewire manipulation[22]. However,unsuccessful EUS-RV via this approach compels endoscopists to change the access route in subsequent EUS-BD. Given that change of access route was unnecessary for the success of subsequent transmural stenting in this study, we need to be cautious about the selection of the D2 approach. This idea is supported by a novel individualized EUS-BD algorithm based on patient anatomy[23]. In this algorithm,Tyberg et al[23]have proposed that the intrahepatic approach should be chosen when the intrahepatic bile duct is dilated. The extrahepatic approach needs to be considered if the intrahepatic bile duct is not dilated or when the intrahepatic method is unsuccessful. From the viewpoint of troubleshooting in cases of unsuccessful initial EUS-RV, the intrahepatic approach could be the first choice of EUS-RV for patients exhibiting intrahepatic bile duct dilation, given this approach is easy to convert to transmural stenting. Support for this idea comes from recent studies in which no significant difference in success or AE rates have been observed between the intrahepatic and extrahepatic bile duct approaches[24,25]. In any case, our results provide evidence that transmural stenting is useful as a rescue EUS-BD method when the initial EUS-RV is unsuccessful.
In this study, 4 cases of bile duct stones treated with EUS-BD were included.Among these 4 cases, 3 cases were converted from EUS-RV to transmural stenting. In these cases, the rendezvous technique via the fistula was performed after fistula formation by transmural stenting, and the stones were successfully extracted. These results suggest that transmural stenting and biliary drainage followed by the rendezvous technique via the created fistula might be a useful treatment strategy for patients exhibiting obstructive jaundice or cholangitis due to biliary stones[26].

Figure 3 Technical outcomes of each initial endoscopic ultrasound-guided biliary drainage technique in this study. A: EUS-guided rendezvous technique; B:EUS-guided choledochoduodenostomy; C: EUS-guided hepaticogastrostomy. EUS-RV: EUS-guided rendezvous technique; EUS-CDS: EUS-guided choledochoduodenostomy; EUS-HGS: EUS-guided hepaticogastrostomy; EUS-AS: EUS-guided antegrade stenting; PTBD: Percutaneous transhepatic biliary drainage.
The technical success rate of the initial EUS-CDS in this study was 76.9%, which is lower than that published in recent reviews[16,25]. Failures in target puncture and puncture tract dilatation comprised 75% of the unsuccessful cases in this study.Currently, several useful dilators dedicated to EUS-BD have been developed, such as a tip-tapered bougie dilator (ES Dilator; Zeon Medical Co., Tokyo, Japan)[27], a finegauge balloon dilator (REN Biliary Dilation Catheter; Kaneka Co., Ltd, Osaka,Japan)[28], and a fine-gauge electrocautery dilator (Fine 025; Medico’s Hirata Inc.,Osaka, Japan)[29]. Unfortunately, these useful dilators were not available during the study period. Therefore, the lack of diathermic dilator use might have contributed to the low technical success of EUS-CDS in this study. Regarding conversion from the initial EUS-CDS technique, EUS-HGS is theoretically a good indication, and EUS-GBD can also be a treatment option in cases with a patent cystic duct[19]. As shown in Figure 3B, the treatment methods were converted to EUS-HGS in two-thirds of the unsuccessful EUS-CDS cases.

Figure 4 Technical and clinical outcomes of endoscopic ultrasound-guided biliary drainage in all 208 cases. Treatment method conversion for unsuccessful initial EUS-BD cases improved both technical and clinical success rates. EUS-BD: EUS-guided biliary drainage; ERCP: Endoscopic retrograde cholangiopancreatography; PTBD: Percutaneous transhepatic biliary drainage; AE: Adverse event.
The indications for EUS-HGS are much broader than EUS-CDS because the latter technique is contraindicated in cases with surgically altered anatomy and duodenal obstruction. EUS-HGS can be performed in those cases as well as in cases with distal bile duct obstruction. In fact, more than half of the cases underwent EUS-HGS as the initial EUS-BD in this study. Regarding troubleshooting for unsuccessful initial EUSHGS, it is difficult to select the optimal conversion treatment method among the following: Rechallenge of EUS-HGS on another bile duct branch, change of puncture target from the intrahepatic bile duct to the extrahepatic bile duct or gallbladder, or change of drainage methods to EUS-RV or antegrade stenting. Selection of the treatment methods requires careful consideration of a combination of factors, such as patient anatomy, underlying disease, and the location of the biliary stricture. Even in the presence of the influential factors described above, the selection of the intrahepatic approach as the initial EUS-BD allows us to perform transmural stenting, antegrade stenting, and EUS-RV without changing the puncture route. Although some studies have shown a higher incidence of AEs with the intrahepatic approach than that in the extrahepatic[30,31], a recent meta-analysis found no difference[24]. Considering that various dedicated devices for EUS-BD are available and the safety of EUS-BD has been confirmed, giving priority to the intrahepatic approach might be acceptable from the viewpoint of ease of conversion. A recent study proposed the algorithm of conversion from the intrahepatic to the extrahepatic approach after unsuccessful intrahepatic drainage based on 2 cases of this conversion[24]. Along the lines of this small case study, our results could provide further clinical evidence of the usefulness of the conversion technique to select in cases of initial failure of EUS-HGS.
There are some limitations in this study. First, it was a retrospective study conducted in a single center with a relatively small number of patients. Second,selection bias might have occurred due to the nonrandomized nature of the study,although the EUS-BD treatment algorithm was established to minimize the selection bias. Third, lumen-apposing metal stents (LAMSs) were not used in this study. Recent studies have described the efficacy and safety of LAMSs for EUS-BD procedures, and LAMSs are increasingly applied in EUS-BD[32-34]. The advantage of the LAMSs is a reduction in the risk of stent migration and bile leakage, given they facilitate the creation of a sealed transmural conduit between the drainage lumen and the gastrointestinal tract. Unfortunately, LAMSs were not commercially available in Japan during the study period.
In conclusion, target puncture, puncture tract dilation, and guidewire manipulation are 3 major procedural steps associated with failure of initial EUS-BD. Among the 3 steps, guidewire manipulation is the most technically challenging aspect, especially in the EUS-RV technique. To date, no consensus for the choice of initial EUS-BD technique has been reached. Given the high success rate in this study, when initially planned EUS-BD is difficult, treatment method conversion during a single endoscopic session appears to be feasible and safe. Further multicenter and prospective studies with a larger cohorts are necessary to confirm the suitability and utility of the conversion to another EUS-BD technique from the initial one.
ARTICLE HIGHLIGHTS
Research background
Since it was initially described in 2001, endoscopic ultrasound-guided biliary drainage (EUS-BD)has been developed as an alternative therapeutic technique for biliary obstruction. Although many EUS-BD techniques are available, the optimal algorithm of EUS-BD techniques has not yet been well established.
Research motivation
To date, limited data are available on troubleshooting when the initial EUS-BD plan is challenging. When it was difficult to accomplish the initial EUS-BD procedure, we attempted to convert the puncture target or drainage method in the same endoscopic session.
Research objectives
This study aimed to evaluate the usefulness of converting the treatment methods during a single endoscopic session for difficult cases in initially planned EUS-BD.
Research methods
Patients with biliary obstruction undergoing EUS-BD between May 2008 and April 2016 in a single tertiary-care center were retrospectively reviewed based on our prospectively accumulated database.
Research results
During the study period, 208 patients underwent EUS-BD. In 18.8% of the patients, the treatment methods were converted from the initial plan. The technical and clinical success rates of the conversion cases were 97.4% and 89.5%, respectively. The rate of AEs was 10.3% and all were graded as mild. Puncture target and drainage technique were altered in 25 and 14 cases,respectively. The final technical success rate of all the 208 cases was 97.1%, and that of the initially planned EUS-BD was 78.8%.
Research conclusions
When initially planned EUS-BD is technically challenging, alteration of treatment methods during the single endoscopic session contributed to improvements in the technical success of EUS-BD, without incurring serious AEs.
Research perspectives
Future, multicenter, and prospective studies with larger cohorts are necessary to confirm the suitability and utility of converting the treatment methods in the same endoscopic session from the initially planned EUS-BD technique.
杂志排行
World Journal of Gastroenterology的其它文章
- Results of meta-analysis should be treated critically
- Two case reports of novel syndrome of bizarre performance of gastrointestinal endoscopy due to toxic encephalopathy of endoscopists among 181767 endoscopies in a 13-year-university hospital review:Endoscopists, first do no harm!
- Effect and safety of mark-guided vs standard peroral endoscopic myotomy: A retrospective case control study
- Differentiation of atypical hepatic hemangioma from liver metastases: Diagnostic performance of a novel type of color contrast enhanced ultrasound
- Exosomal miR-182 regulates the effect of RECK on gallbladder cancer
- Kynurenine plays an immunosuppressive role in 2,4,6-trinitrobenzene sulfate-induced colitis in mice