Streptococcus agalactiae: Sensitivity profile in pregnant women attending health units in northeastern Brazil
2020-03-11TaisVianaLedodeOliveiraFabrciaAlmeidaFernandesSantanaCalineNovaisTeixeiraOliveiraMariaLusaCordeiroSantosFabrcioFreiredeMeloCludioLimaSouzarcioVasconcelosOliveira
Tais Viana Ledo de Oliveira, Fabrícia Almeida Fernandes Santana, Caline Novais Teixeira Oliveira, Maria Luísa Cordeiro Santos, Fabrício Freire de Melo, Cláudio Lima Souza, Márcio Vasconcelos Oliveira
Tais Viana Ledo de Oliveira, Fabrícia Almeida Fernandes Santana, Caline Novais Teixeira Oliveira, Maria Luísa Cordeiro Santos, Fabrício Freire de Melo, Cláudio Lima Souza, Márcio Vasconcelos Oliveira, Instituto Multidisciplinar em Saúde, Universidade Federal da Bahia, Vitória da Conquista 45029-094, Bahia, Brazil
Abstract BACKGROUND Group B Streptococcus agalactiae (GBS) is the main etiologic agent associated with early-onset neonatal sepsis, and of all newborns of parturients colonized by GBS, approximately 1%-2% develop invasive, early-onset disease. The risk of infection increases to 15.2% in premature neonates, to 10.7% when the parturient has chorioamnionitis or premature rupture of membranes for more than 24 h and to 9.7% if the mother has postpartum bacteremia. In addition to causing perinatal, neonatal and postnatal deaths, neonatal hospital infection is associated with high costs, as hospitalization is three times longer than in uninfected children. The identification of pregnant women colonized by GBS, through universal screening, associated with the adoption of appropriate antibiotics at the time of delivery are the most successful preventive measures.AIM To evaluate the sensitivity profile of GBS isolated from pregnant women attending Vitória da Conquista-BA.METHODS This is a cross-sectional study with a quantitative approach carried out in the municipality of Vitória da Conquista-Bahia between February 2017 and March 2018. The study population was composed of 210 pregnant women, with a gestational age of 32 to 40 wk, who were aged 18 years or older living in the urban area of the municipality of Vitória da Conquista. After a brief explanation about the research and obtaining a signed an informed consent form, data and vaginorectal swabs were collected from the women for GBS research. Examination of the samples in order to identify the presence of GBS was by culture on sheep blood agar and chromogenic agar for GBS and then, seeded on plates containing streptococcal culture medium and incubated for 18 h to 24 h at 35°C. The antimicrobial sensitivity profile of positive GBS samples was determined by the disk diffusion technique, according to the Clinical and Laboratory Standards Institute manual (2017). The data obtained were stored in a database using Microsoft Office Excel spreadsheets and a descriptive analysis was performed with the aid of the EPI-INFO statistical package (version 3.5.2).RESULTS Among the 210 pregnant women participating in the study, 38 (18.1%) had a positive GBS culture. All strains isolated from GBS were sensitive to 10 U penicillin, 10 µg ampicillin, 30 µg cefotaxime and 30 µg vancomycin. Seven strains (18.4%) resistant to clindamycin 2 µg and eight (21.1%) resistant to erythromycin 15 µg were found. Of these, six were concomitantly resistant to erythromycin and clindamycin, two resistant only to erythromycin and one resistant only to clindamycin. All nine GBS isolates that showed resistance to erythromycin and/or clindamycin showed negative results on the D-test. Two thirds of the isolates showed cMLSB phenotype and resistance only to erythromycin in specimens in this study (02), refers to strains with phenotype M and resistance to clindamycin (01) only with phenotype L.CONCLUSION Chemoprophylaxis for GBS in pregnant women, especially for those allergic to penicillin, should be guided by an antimicrobial susceptibility test as resistant GBS strains were reported in this study.
Key Words: Streptococcus agalactiae; Sensitivity profile; Pregnancy; Clindamycin; Erythromycin; Group B streptococcal disease
INTRODUCTION
Streptococcus agalactiaeor group B streptococcus (GBS) is a known agent of maternal and neonatal infections. Although in most pregnant women colonization by this bacterium is generally asymptomatic, GBS may be responsible for the appearance of chorioamnionitis, endometritis, cystitis, pyelonephritis and febrile bacteremia[1,2].
Vertical transmission of this microorganism can occur in 30% to 70% of neonates whose mothers have a positive culture for this microorganism, in the absence of adequate chemoprophylaxis. In addition, one to two newborns per 1000 live births develop disease caused by this bacterium[3,4]. In this group, GBS is the main cause of sepsis and meningitis, and is a frequent cause of pneumonia[5]. The main measure to prevent neonatal GBS infection is to identify and prophylactically treat pregnant women, thus avoiding puerperal problems and, especially, early neonatal infection[5].
In the most recent update, the Center for Disease Control and Prevention (CDC)[6]reinforces the recommendations for universal screening in the third trimester of pregnancy, through prenatal screening of GBS in material collected from the vaginal opening and the perianal region of all pregnant women who are between 35 wk and 37 wk of gestation. To prevent vertical transmission of GBS, intrapartum prophylaxis with crystalline penicillin G is recommended with 5 million units as an attack dose and 2.5 million units, every 4 h, until delivery[6].
The alternative of using erythromycin and clindamycin has increased, mainly due to patient allergy to penicillin, and as a pharmacological alternative in the absence of the antibiotic of first choice. It is important to consider the signs of increasing GBS resistance rates to these antimicrobials, according to studies carried out in different countries[7].
Resistance to macrolides, such as erythromycin, can occur by methylation of the ribosomal target site, which is the most frequent mechanism. Methylation of the RNA 23s subunit is mediated by methylases encoded by the erm (A) and erm (B) genes that confer resistance to macrolides, lincosamides, such as clindamycin, and streptogramin B, forming the MLSB phenotype, and this expression of resistance can be constitutive (cMLSB) or inducible (iMLSB)[8,9]. Alternatives to this mechanism provide resistance to only one or two of the classes of antibiotics in the MLSB8 complex.
Considering that the prevention and treatment of neonatal infection by GBS in pregnant women are not addressed in the Technical Manual for Prenatal and Puerperium-Qualified and Humanized Attention of the Ministry of Health[10], scientific research on this topic helps to substantiate the production of guidelines for adequate prophylaxis in different populations.
Thus, the objective of this work was to verify the sensitivity profile ofStreptococcus agalactiaeisolated in pregnant women attending health units in the urban area of Vitória da Conquista, Bahia State, Brazil.
MATERIALS AND METHODS
This is a cross-sectional study with a quantitative approach that was carried out in the municipality of Vitória da Conquista-Bahia between February 2017 and March 2018. The study population was composed of pregnant women, with a gestational age of 32 wk to 40 wk, attending 09 basic health units and family health units in the municipality, all located in the urban area, which were selected from the municipality's zoning and followed by drawing lots of units by area.
To calculate the sample size, an error of 5% and a 95% confidence interval were accepted, taking into account the 5191 births performed in the city in 2014 and the prevalence of colonization by GBS of 17%-referenced in a study carried out in the municipality[11]. To define the number of pregnant women in each health unit, the sample N was considered and divided proportionally into the units involved in the study. Pregnant women outside the required gestational period and under the age of 18 years who did not have authorization from those responsible for participating in the study were excluded from the study.
To collect data and samples, the pregnant women and/or guardians were approached, and, after explaining the research and signing the informed consent form, the samples were collected for GBS research. A single vaginal/rectal swab was collected from the women without a speculum by properly trained health professionals at the health units, during prenatal consultations or at scheduled times for sample collection.
The vaginorectal swabs collected from 210 pregnant women between 32 wk and 40 wk of gestation were inoculated in Stuart transport medium, placed inside boxes for biological material, at room temperature, and sent to the Clinical Analysis Laboratory of the Universidade Federal da Bahia–Campus Anísio Teixeira–Instituto Multidisciplinar em Saúde, Vitória da Conquista, Bahia State, Brazil.
The samples were placed in a chromogenic medium (Biomérieux®) for streptococci by the depletion technique, and incubated for 18 h to 24 h at 35°C to 37°C. Subsequently, the samples were placed on blood agar (Isofar®) 5% (sheep blood) and incubated for 18 h to 24 h at 35°C to 37°C in an atmosphere of 5% CO2. Following the protocol, in order to increase the sensitivity detection, the swabs were inoculated into tubes containing Todd-Hewitt medium (Biomérieux®) at 35°C to 37°C from 18 h to 24 h. The samples were then placed in chromogenic medium (Biomérieux®) for streptococci and blood agar (Isofar®) 5% (lamb), under the same incubation conditions as before.
For blood agar cultures suggestive of GBS (small colony growth with a grayish pattern, surrounded by a discrete halo of β-hemolysis, or without hemolysis), the catalase test, conventional Gram staining followed by microscopic analysis were performed. For Gram-positive, catalase-negative colonies, obtained from blood agar and for pink or red colonies obtained from chromogenic medium, a CAMP test (Christie, Atkins and Munch-Petersen) was performed using the kit composed of Todd-Hewitt and Hemolisinabac®(Probac do Brasil) and latex agglutination (serogroupage) using the Slidex®Strepto Plus B kit (Biomeriéux), to confirm the species.
The antimicrobial sensitivity profile of positive GBS samples was determined by the disk diffusion technique, according to the Clinical and Laboratory Standards Institute (CLSI)12 manual[12].
The evaluation of antimicrobial susceptibility was performed in Mueller Hinton medium (Isofar®) supplemented with 5% sheep blood for antibiotics: penicillin 10 U, ampicillin 10 µg, cefotaxime 30 µg, clindamycin 2 µg, erythromycin 15 µg and vancomycin 30 µg. The choice of antibiotics was made based on the technical indications of the CLSI12 manual and on the availability of medicines in the municipal health system.
To perform the D-test, bacterial suspensions were prepared in sterile saline (0.9%), with a turbidity equivalent to 0.5 on the McFarland scale obtained from recent cultures. This suspension was added to dissemination culture medium and erythromycin (15 µg) and clindamycin (2 µg) antibiotic discs were placed 12 mm apart to determine the resistance phenotype. The plates were incubated at 35-37°C and the reading was performed after 20 h to 24 h of incubation. Growth inhibition halos were measured and interpreted according to the CSLI12 manual[12].
The data were stored in a database using Microsoft Office Excel spreadsheets and a descriptive analysis was performed with the aid of the EPI-INFO statistical package (version 3.5.2).
This research was approved by the Teaching and Research Committee of the Municipal Health Secretariat of Vitória da Conquista and approved by the Research Ethics Committee of the Universidade da Federal da Bahia, under the number CAAE 58104116.8.0000.5556 and protocol number 1.736.058.
RESULTS
Of 210 pregnant women who participated in the study, 38 had a positive culture for GBS, corresponding to a prevalence of 18.1%. Table 1 presents the analysis of the sensitivity profile of GBS strains isolated from the pregnant women included in the study.
All isolated samples of GBS were sensitive to penicillin 10 U, ampicillin 10 µg, cefotaxime 30 µg and vancomycin 30 µg. Seven samples (18.4%) were resistant to clindamycin 2 µg and eight (21.1%) were resistant to erythromycin 15 µg. Of these, six were concomitantly resistant to erythromycin and clindamycin, two were resistant only to erythromycin and one resistant only to clindamycin. All nine GBS isolates that showed resistance to erythromycin and/or clindamycin showed negative results on the D-test.
DISCUSSION
The CDC6 recommendations indicate penicillin as the drug of choice for the prophylaxis of neonatal intrapartum disease. The description of GBS resistance to this antibiotic remains very low, maintaining it as the antibiotic of choice[5]. All strains of GBS isolated in this study were sensitive to penicillin. However, it is important to discuss allergy to penicillin. The literature indicates that approximately 10% of the population is allergic to B-lactams, such as penicillin[13]. For these patients, international protocols recommend the use of erythromycin and/or clindamycin, although there are reports of a significant increase in GBS resistance to these antimicrobials[7,13].
In this study, resistance to clindamycin and erythromycin was estimated at 18.4% and 21.1% respectively. These resistance rates are high when compared to the findings of Borgeret al[7], Dutraet al[14]and Santoset al[15]in the Southeast; however, they are similar to the results found in a study carried out in the Northeast of Brazil[16].
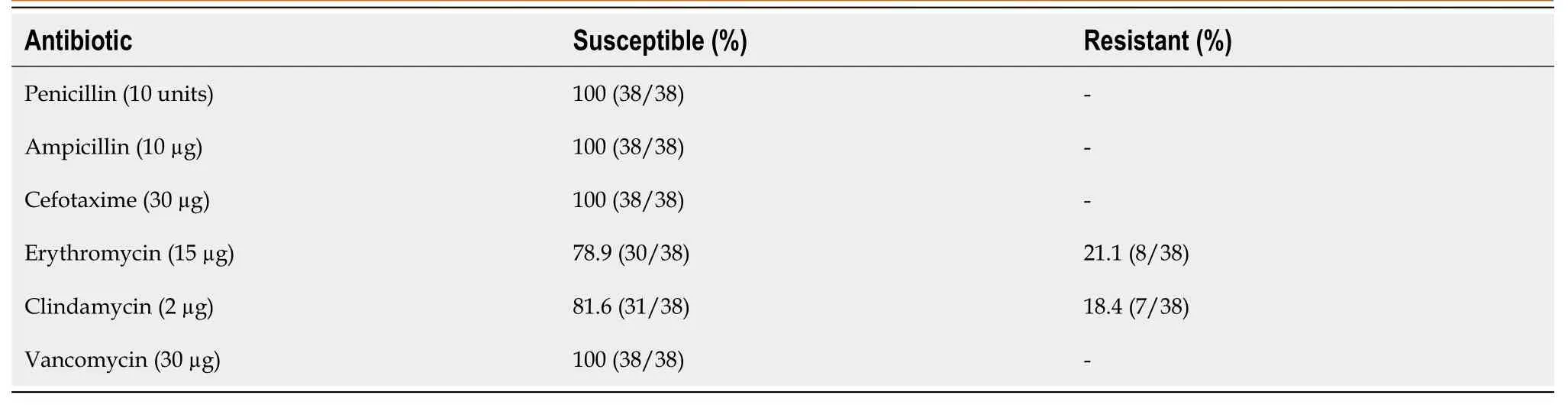
Table 1 Susceptibility profile of group B Streptococcus samples isolated from pregnant women participating in the study (n = 38)
The rates of resistance of GBS to erythromycin and clindamycin give rise to caution when using these antimicrobials for GBS prophylaxis and ratify the importance of using susceptibility tests to guide the correct choice of antimicrobials for prophylaxis in pregnant women[15].
In this study, the results of the D-test were negative for 100% of the strains of GBS isolated, indicating that there was no reduction in sensitivity induced by erythromycin or clindamycin. Two thirds of the isolates showed a cMLSB phenotype, in agreement with the results of Martínezet al[17]. Resistance only to erythromycin in specimens in this study (02), refers to strains with phenotype M and resistance to clindamycin (01) only with phenotype L[18,19].
In these same GBS strains analyzed in the present investigation, resistance genes -mefA gene and genes of theermfamily[20]- were identified in another study developed in parallel, corroborating the findings described here. These genes confer resistance to macrolides and the MSLB complex, respectively[19]. However, according to Santana[20], resistance to clindamycin could be associated with other resistance genes that were not tested in the study in question.
All strains were sensitive to ampicillin, cefotaxime and vancomycin, corroborating findings in the national literature by Borgeret al[7], Dutraet al[14], Santoset al[15]. In the present study, GBS sensitivity to ceftriaxone was not evaluated; however, it is important to note that Andradeet al[16]found resistance of 12.7% to this antibiotic.
CONCLUSION
The results of this work reinforce the importance of knowing the sensitivity profile for GBS. The observed rates of resistance to erythromycin and clindamycin indicate the need for more adequate and responsible management, especially in patients with a history of allergy to penicillin or when this drug is not available. Adequate management is very relevant in the clinical context as it prevents the evolution of possible complications in neonates and thus contributes greatly to reducing morbidity and mortality. It also effectively reduces costs due to hospitalizations and more complex procedures, and decreases the occupancy of beds in neonatal ICUs, optimizing their use for non-preventable causes.
ARTICLE HIGHLIGHTS
Research background
Streptococcus agalactiae (Group B Streptococcus, GBS) is a bacterium known to be a causative agent of maternal and neonatal infections. The colonization of pregnant women by GBS, although most patients are asymptomatic, represents a risk for several pathologies, from chorioamnionitis, endometritis, cystitis, and pyelonephritis to febrile bacteremia. In addition, this infection can trigger pneumonia, meningitis and sepsis in neonates. To prevent this vertical transmission, prophylaxis with crystalline penicillin G or macrolides is recommended. However, with increasing levels of resistance, it is necessary to know the local resistance profile regarding adequate antimicrobial use.
Research motivation
It is important to identify and prophylactically treat pregnant women to avoid puerperal problems, especially early neonatal infection. In this sense, knowledge on GBS colonization detection and resistance rates to standard treatments is essential for clinical practice on GBS disease.
Research objectives
To verify the sensitivity profile ofStreptococcus agalactiaeisolated in pregnant women attending health units in the urban area of Vitória da Conquista, in Bahia State, Brazil.
Research methods
This is a cross-sectional study with a quantitative approach where 210 vaginorectal swabs collected from pregnant women attending health units in the county of Vitória da Conquista, in Bahia State, Brazil were analyzed. Pregnant women with gestational ages from 32 wk to 40 wk were eligible for this study. A single vaginal/rectal swab was collected from the women without a speculum, inoculated into Stuart transport medium, and placed in a chromogenic medium (Biomérieux®) for streptococci by the depletion technique. Subsequently, the samples were added to blood agar (Isofar®) 5% (sheep blood) incubated for 18 h to 24 h at 35°C to 37°C in an atmosphere of 5% CO2.The swabs were then inoculated into tubes containing Todd-Hewitt medium (Biomérieux®) at 35°C to 37°C from 18 h to 24h and then into chromogenic medium (Biomérieux®) for streptococci and blood agar (Isofar®) 5% (lamb).
All small colony growth with a grayish pattern, surrounded by a discrete halo of βhemolysis, or without hemolysis (characteristics for GBS identification) underwent the catalase test and conventional Gram staining followed by microscopic analysis. For Gram-positive, catalase-negative colonies, obtained from blood agar and pink or red colonies obtained from chromogenic medium, a CAMP test (Christie, Atkins and Munch-Petersen) was performed using the kit composed of Todd-Hewitt and Hemolisinabac®(Probac do Brasil) and latex agglutination (serogroupage) using the Slidex®Strepto Plus B kit (Biomeriéux), to confirm the species. The antimicrobial sensitivity profile of positive GBS samples was determined by the disk diffusion technique, according to the CLSI12 manual, in Mueller Hinton medium (Isofar®) supplemented with 5% sheep blood.
Research results
Among the 210 pregnant women participating in the study, 38 (18.1%) had a positive GBS culture. All GBS strains isolated were sensitive to 10 U penicillin, 10 µg ampicillin, 30 µg cefotaxime and 30 µg vancomycin. Seven strains (18.4%) resistant to clindamycin 2 µg and eight (21.1%) resistant to erythromycin 15 µg were observed. Of these, six were concomitantly resistant to erythromycin and clindamycin, two resistant only to erythromycin and one resistant only to clindamycin. All nine GBS isolates that showed resistance to erythromycin and/or clindamycin showed negative results on the D-test. Two thirds of the isolates showed cMLSB phenotype and resistance only to erythromycin in specimens in this study (02), refers to strains with phenotype M and resistance to clindamycin (01) only with phenotype L.
Research conclusions
Chemoprophylaxis for GBS in pregnant women, especially for those allergic to penicillin, should be guided by an antimicrobial susceptibility test as resistant GBS strains were reported in this study.
Research perspectives
The information provided by this study is applicable for the elaboration of GBS guidelines for adequate prophylaxis in different populations.