Intussusception in an infant with two non-diagnostic abdominal ultrasound studies
2019-11-24VanessaSantosJamesEspinosaAlanLucerna
Vanessa Santos, James Espinosa, Alan Lucerna
1 Emergency Medicine Department, Orange Regional Medical Center, Middletown, New York 10940-4133, USA
2 Emergency Medicine Department, Rowan University School of Osteopathic Medicine, Stratford, New Jersey 08084-1500, USA
Dear editor,
Intussusception is the invagination of one portion of the intestines into another, and is the most common form of intestinal obstruction in infants.[1]The vast majority of cases of intussusception are idiopathic, and are thought to be due to hyperplasia of the lymphoid tissue in the Peyer’s patches of the terminal ileum. The clinical diagnosis of intussusception may be difficult to make as it may be masked by its propensity to occur in the context of viral gastroenteritis. The diagnosis of intussusception can be made with sonography, plain abdominal radiographs or contrast enema. Ultrasonography has been found to have a negative predictive value of 100%.However, we report a case of a full term 7-month-old male with no significant medical history who presented to the emergency department with fever, decreased PO intake, decreased urine output, and vomiting for three days, that was subsequently diagnosed with a small bowel obstruction secondary to intussusception without sonographic evidence of intussusception on two ultrasound studies.
CASE
A full term 7-month-old male presented to the emergency department (ED) with vomiting and fevers for the past 3 days. The patient was having multiple bouts of non-bilious, non-bloody emesis throughout the day every day. He had no abdominal pain or diarrhea. He was not as active as he normally was. The patient’s mother reported that he was in his normal state of health the day before the onset of symptoms. She stated his vaccines were up-to-date and he had no recent travel or known sick contacts. The infant had no significant medical or surgical history. Initial vital signs were as follows:temperature 101.0 degrees Fahrenheit, heart rate 120 beats/minute, blood pressure 124/80 mmHg, respiratory rate 36 breaths per minute and oxygen saturation 98%on room air. Physical exam revealed an ill-appearing male who was lethargic but non-toxic and in no acute distress. Neck was supple with no jugular venous distension. Heart was regular with no murmurs, rubs or gallops. Lungs were clear to auscultation bilaterally. The abdomen was soft, non-tender, non-distended with no hepatosplenomegaly or peritoneal signs. The abdominal exam also showed a small reducible umbilical hernia,and there was no palpable olive mass.
After evaluation, the infant was given ondansetron PO, and a trial of Pedialyte without further emesis. The infant successfully drank 6 oz of Pedialyte, and was discharged with the diagnosis of gastroenteritis.
Additionally, at home the next day, the caregiver noticed that his abdomen was slightly distended,and he continued to have multiple episodes of nonbilious vomiting. His mother stated that he was having normal bowel movements. She stated she spoke with the pediatrician who informed her that abdominal distension could occur from vomiting. The following day, the caregiver raised the same concerns. However,she remembers touching his abdomen and noting that it was soft, and appeared slightly larger than normal.That night, the patient’s mother noted the infant had not slept at all, continued to have fevers, and had been having uncontrollable intermittent crying spells. She also noted that the patient’s abdomen was a bit firm when she placed him on the bed to check his diaper. She was additionally alarmed when the patient was found to have a small amount of bright red blood in his stool. The patient returned to the ED where he had a more extensive workup. Initial labs included a complete blood count with platelet & differential, complete metabolic panel,C-reactive protein (CRP), blood cultures and urinalysis.The patient had no urine output upon catherization. Vital signs were as follow: temperature 101.1 degrees F, heart rate 162 beats per minute, respiratory rate 26 breaths per minute, pulse oximetry 100% on room air, and blood pressure was not recorded initially. Pertinent physical exam revealed a well-developed male who was febrile,lethargic, and appeared dehydrated, with a nasogastric tube in place with bilious drainage. Neck was supple.Heart was tachycardic with no murmurs, rubs or gallops.Lungs were cleared to auscultation bilaterally with no wheezes, rales or rhonchi. The abdomen was rigid,distended, and diffusely tender, with no guarding or rebound.
Initial laboratory data was noteworthy for platelets 581×103/mcL (206-445) with 46% segmented neutrophils & 3% bands and a CRP 2.90 mg/dL(≤0.5). An abdomen flat and erect two view X-ray was performed showing diffuse gaseous distention of multiple loops of predominantly small bowel with air- fluid levels and minimal gas in the rectum (Figure 1).
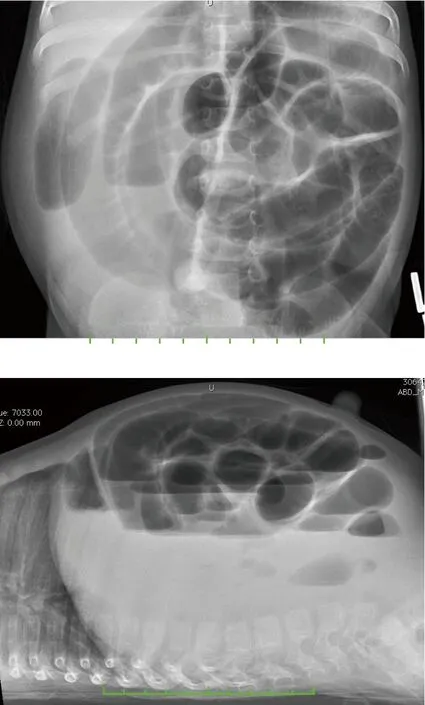
Figures 1. Gaseous distension of multiple bowel loops and air- filled levels in the upright and supine position respectively.
He was subsequently sent for an abdominal ultrasound specific for intussusception and appendicitis that demonstrated no ileocolic intussusception, and multiple dilated gas and fluid-filled levels of bowel throughout the abdomen (Figure 2). The infant also had an anterior abdominal wall ultrasound (Figure 3)showing intact abdominal wall without evidence of bowel containing hernia. The patient was transferred to a children’s hospital with pediatric surgeons on staff, in case a surgical intervention was necessary.

Figure 2. Sonogram with no evidence of ileocolic Intussusception in the right lower quadrant.

Figure 3. Abdominal wall without incarcerated hernia on ultrasound.
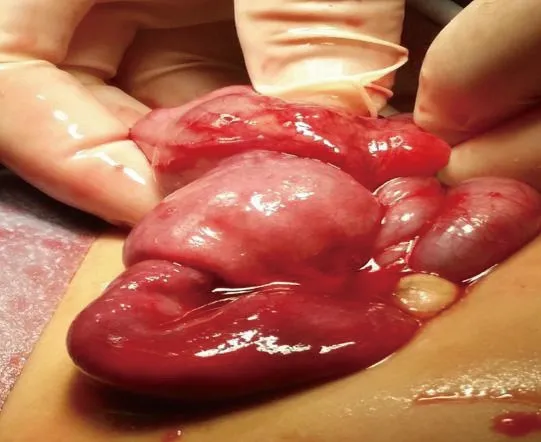
Figure 4. Intraoperative view of ileoileocolic intussusception prior to reduction.
In the ED of the receiving hospital, the child had a repeat abdominal ultrasound demonstrating again, a small bowel obstruction with no evidence of intussusception.The pediatric surgeon that was consulted reviewed the images with the radiologist. It was decided that while no evidence of intussusception was noted on either ultrasound, intussusception was highly suspected.The possibility of performing an enema was explored but due to a high chance of failure was subsequently rejected. The pediatric surgeon therefore recommended exploratory laparoscopy. The patient was taken to the operating room and was indeed found to have ileoileocolic intussusception (Figure 4). The patient had a successful outcome during surgery. The patient remained in the hospital for approximately 6 days, and made a great recovery.
DISCUSSION
Intussusception, although uncommon condition,is the most common cause of bowel obstruction classically presenting in infants and children aged 4 months to 2 years of age. The classic triad is comprised of paroxysmal abdominal pain, vomiting, and “currant jelly” stool. However, the full triad is present only 20%of the time and the diagnosis may be obscured by the tendency for intussusception to occur in the context of viral gastroenteritis (especially adenovirus).[2]Abdominal pain is usually absent in an infant upon presentation.
Radiological reduction of intussusception (air or saline enema) is the first-line treatment and is successful in more than 80% of patients.[3]Absolute contraindications to radiological reduction include intestinal perforation, peritonitis and shock. Relative contraindications to non-operative reduction include chronic and neonatal Intussusceptions, history greater than 48 hours, small bowel obstruction on plain radiograph, and children older than 2 years.[1]Moreover,if any of these situations are present there is an increased risk of complications and lower likelihood of success with non-operative management. Pediatric laparoscopic surgery has significantly increased over the past 20 years,and it is considered safe, and efficacious for the treatment of intussusception. Additionally, pediatric laparoscopy has been linked to a major reduction in length of stay compared to open surgery, regardless of the etiology.[3]
In recent years, several studies have found ultrasonography, with a false-negative rate approaching zero, to be reliable screening tool for children deemed at low risk of intussusception.[4]In a study conducted by Harrington et al,[4]sonography had a negative predictive value of 100%, and only one ultrasound demonstrated a false-positive result for intussusception. However,in the case we presented, two experienced radiologists performed two separate abdominal ultrasounds that were both negative for intussusception on our patient.Stanley et al,[5]support the notion that in their series all the intussusceptions were identified by ultrasound and none were missed. Thus, ultrasound appears to be a reliable screening tool for intussusception. However,an ultrasound may be falsely negative if there is a significant amount of gas blocking ultrasound waves or if there is intermittent intussusception. Nevertheless, this case demonstrates the need for a high index of suspicion for intussusception, in the appropriate clinical scenario,even in the face of an ultrasound that is negative for intussusception.
CONCLUSION
Clinical diagnosis of intussusception remains a tricky prospect and a challenging diagnosis.[6]The classic presentation of abdominal pain, bilious vomiting, and “currant jelly” stools, and a palpable abdominal mass is seldom entirely present. The case we presented demonstrated a patient with symptoms that initially resembled a viral syndrome, but upon return to the emergency department his symptoms were concerning for intussusception, despite having had two non-diagnostic ultrasounds. Sonography is a reliable diagnostic and non-invasive tool for suspected intussusception. Nonetheless, even with negative imaging studies, if the patient has symptoms concerning for intussusception, the physician must keep it in their differential, and consult a general surgeon for further evaluation.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:No any benefits have been received from a commercial party related directly or indirectly to the study.
Contributors:VS proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
杂志排行
World journal of emergency medicine的其它文章
- Information for Readers
- World Journal of Emergency Medicine
- Venous thromboembolism in the emergency department: A survey of current best practice awareness in physicians and nurses in China
- The use of outcome feedback by emergency medicine physicians: Results of a physician survey
- Rapid sequence induction (RSI) in trauma patients:Insights from healthcare providers
- Comparison between intravenous morphine versus fentanyl in acute pain relief in drug abusers with acute limb traumatic injury
